Physician-Related Services Manual
Printing the manual material found at this website for long-term use is not advisable. Department Policy material is updated periodically and it is the responsibility of the users to check and make sure that the policy they are researching or applying has the correct effective date for their circumstances.
If you experience any difficulty opening a section or link from this page, please email the webmaster.
How to Search this manual:
This edition has three search options.
- Search the whole manual. Open the Complete Manual pane. From your keyboard press the Ctrl and F keys at the same time. A search box will appear. Type in a descriptive or key word (for example "Denials". The search box will show all locations where denials discussed in the manual.
- Search by Chapter. Open any Chapter tab (for example the "Billing Procedures" tab). From your keyboard press the Ctrl and F keys at the same time. A search box will appear. Type in a descriptive or key word (for example "Denials". The search box will show where denials discussed in just that chapter.
- Site Search. Search the manual as well as other documents related to a particular search term on the Montana Healthcare Programs Site Specific Search page.
Prior manuals may be located through the provider website archives.
Physician-Related Services Manual
Updated 03/05/2021
Physician-Related Services Manual
To print this manual, right click your mouse and choose "print". Printing the manual material found at this website for long-term use is not advisable. Department Policy material is updated periodically and it is the responsibility of the users to check and make sure that the policy they are researching or applying has the correct effective date for their circumstances.
Update Log
Publication History
This publication supersedes all previous Physician-Related Services handbooks. Published by the Montana Department of Public Health & Human Services, January 2005.
Updated September 2002, January 2003, June 2003, July 2003, August 2003, September 2003, December 2003, June 2004, September 2004, November 2004, January 2005, March 2005, January 2006, April 2006, July 2006, July 2008, July 2014, July 2015, August 2015, September 2016, November 2016, September 2017, and March 2021.
CPT codes, descriptions and other data only are copyright 2014 American Medical Association (or such other date of publication of CPT). All Rights reserved. Applicable FARS/DFARS Apply.
Update Log
03/05/2021
Updated the discrimination contact information in the Definitions and Acronyms chapter.
09/29/2017
Physician-Related Services Manual converted to an HTML format and adapted to 508 Accessibility Standards. Language throughout the manual was updated.
11/28/2016
In summary, the Page 5.6 of the Billing Procedures chapter was amended to add information for locum tenens, several links were updated, and two blank pages were removed. The Table of Contents and Index sections were adjusted, several links were updated in the Introduction and Covered Services Chapter, the entire manual was formatted as approved by the September 2016 Manuals Meeting for initial 508 adaptations, and the Cover page was amended with the current date.
09/12/2016
In summary, the entire manual has undergone formatting changes, the Billing Procedures section has had some minor language changes and the Cover reflects the current date.
08/31/2016
In summary, The cost share section was removed from the Billing Procedures Chapter, related entries were removed from the Index Section adjustments were made to the Index Section , and the date was changed on the Cover Page.
07/31/2015
Physician-Related Services, August 2015: Entire Manual, Removed EPSDT Well-Child
07/08/2014
Physician-Related Services, July 2014: Multiple Chapters
07/14/2008
Physician-Related Services, March 2008: Key Contacts, Completing a Claim Form, Prior Authorization, Billing for Immunizations
07/25/2006
Physician-Related Services, July 2006: Well-Child EPSDT Update
04/25/2006
Physician-Related Services, April 2006: Revised Instructions for Completing a Claim, Revised Information on How Cost-Sharing Affects Claim Payment
01/05/2006
Physician-Related Services, September 2005: New EPSDT, Hysterectomy Acknowledgement Form, Revised Information on Imaging Modifiers, Billing for Immunizations, and ER Visits for Clients Under Age 2
03/01/2005
Physician-Related Services, March 2005: Hysterectomy Acknowledgement Update
01/25/2005
Physician-Related Services, January 2005: Rule References Added, Updates to Covered Services, PA and Modifiers
11/16/2004
Physician-Related Services, November 2004: Updated Prescription Drug PA Criteria
09/15/2004
Physician-Related Services, September 2004: Team Care Added
06/16/2004
Physician-Related Services, July 2004: Clarification on Sterilizations, Hysterectomies, Abortions and HIPAA and Drug PA Update
12/23/2003
Physician-Related Services, December 2003: Immunizations, PA Criteria, Family Planning, and Using Modifiers
09/16/2003
Physician-Related Services, September 2003: Hysterectomies and Prescription Drug PA Update
08/20/2003
Physician-Related Services, June 2003: New Emergency Services Policy and Hard Card Information
07/28/2003
Physician-Related Services, Hysterectomy Requirements
06/01/2003
Physician-Related Services, New PA Requirements and Hysterectomy Information
01/02/2003
Physician-Related Services, January 2003: Prior Authorization
09/01/2002
Physician-Related Services, September 2002: Cost Sharing
End of Update Log Chapter
Table of Contents
Key Contacts and Websites
Introduction
Manual Organization
Manual Maintenance
Rule References
Claim Review (MCA 53-6-111, ARM 37.85.406)
Getting Questions Answered
Covered Services
General Coverage Principles
- Services within Scope of Practice (ARM 37.85.401)
- Services Provided by Physicians (ARM 37.86.101 - 105)
- Services Provided by Mid-Level Practitioners (ARM 37.86.201 - 205)
- Services Provided by Podiatrists (ARM 37.86.501 - 506)
- Services Provided by Independent Labs (ARM 37.86.3201 - 3205)
- Services Provided by Independent Imaging Facilities (ARM 37.86.3201 - 3205)
- Services Provided by Independent Diagnostic Testing Facilities (ARM 37.85.220)
- Services Provided by Public Health Clinics (ARM 37.86.1401 - 1406)
- Non-Covered Services (ARM 37.85.201 and ARM 37.86.205)
- Importance of Fee Schedules
Coverage of Specific Services
- Abortions (ARM 37.86.104)
- Cosmetic Services (ARM 37.86.107)
- Early and Periodic Screening, Diagnostic, and Treatment Services Program
- Family Planning Services (ARM 37.86.1701)
- Home Obstetrics (ARM 37.85.207)
- Immunizations
- Infertility (ARM 37.85.207)
- Prescriptions (ARM 37.86.1102)
- Routine Podiatric Care
- Sterilization (ARM 37.86.104)
- Surgical Services
- Telemedicine Services
- Transplants
- Weight Reduction
Prior Authorization
Prior Authorization for Retroactively Eligible Members
Coordination of Benefits
When Members Have Other Coverage
Identifying Other Sources of Coverage
When a Member Has Medicare
- Medicare Part A Claims
- Medicare Part B Crossover Claims
- When Medicare Pays or Denies a Service
- When Medicaid Does Not Respond to Crossover Claims
Submitting Medicare Claims to Medicaid
When a Member Has TPL (ARM 37.85.407)
- Exceptions to Billing Third Party First
- Requesting an Exemption
- When the Third Party Pays or Denies a Service
- When the Third Party Does Not Respond
Other Programs
Billing Procedures
Claim Forms
Timely Filing Limits (ARM 37.85.406)
- Tips to Avoid Timely Filing Denials
When to Bill Medicaid Members (ARM 37.85.406)
Member Cost Sharing (ARM 37.85.204 and ARM 37.85.402)
When Members Have Other Insurance
Billing for Retroactively Eligible Members
Place of Service
Multiple Visits (E/M Codes) on Same Date
Coding
Using the Medicaid Fee Schedule
Using Modifiers
Billing Tips for Specific Provider Types
- Mid-Level Practitioner Billing
- Physician Billing
- Podiatrist Billing
- Independent Diagnostic Testing Facilities
- Independent Labs
- Imaging
RHC/FQHC - Professional Services in Hospitals
Billing Tips for Specific Services
- Abortions
- Anesthesia
- Bundled Services
- Cosmetic Services
- EPSDT Well-Child Screens
- Family Planning Services
- Immunizations
- Obstetrical Services
- Reference Lab Billing
- Sterilization
- Surgical Services
- Assistant at Surgery
- Telemedicine Services
- Transplants
- Weight Reduction
- Unlisted Procedures
Submitting Electronic Claims
- Electronic Claims
Billing Electronically with Paper Attachments
Submitting Paper Claims
Claim Inquiries
The Most Common Billing Errors and How to Avoid Them
Submitting a Claim
CMS-1500 Agreement
Avoiding Claim Errors
How Payment is Calculated
Overview
The RBRVS Fee Schedule
- Fee Calculation
- Basis of Relative Values
- Composition of Relative Values
- Site of Service Differential
- Conversion Factor
- Policy Adjuster
- Global Periods
- Professional and Technical Components
- Other Modifiers
- How Modifiers Change Pricing
- Professional Differentials
- Charge Cap
- Bundled Codes
- Status Codes
Anesthesia Services
- Time Units
- Base Units
- Fee Calculation
- Modifiers
Clinical Lab Services (ARM 37.85.212)
Vaccines and Drugs Provided within the Office
How Cost Sharing Is Calculated on Medicaid Claims
How Payment Is Calculated on TPL Claims
How Payment Is Calculated on Medicare Crossover Claims
Other Department Programs
Appendix A: Forms
Appendix B: Place of Service Codes
Definitions and Acronyms
Index
End of Table of Contents Chapter
Key Contacts and Websites
End of Key Contacts and Websites Chapter
Introduction
Thank you for your willingness to serve members of the Montana Medicaid program and other medical assistance programs administered by the Department of Public Health and Human Services.
Manual Organization
This manual provides information specifically for physicians, mid-level practitioners, podiatrists, public health clinics, family planning clinics, independent laboratories independent imaging facilities, and independent diagnostic testing facilities.
Most chapters have a section titled Other Programs that includes information about other Department programs such as the Mental Health Services Plan (MHSP) and Healthy Montana Kids (HMK)/CHIP. Other essential information for providers is contained in the separate General Information for Providers manual. Each provider is asked to review both manuals.
A table of contents and an index allow you to quickly find answers to most questions There is a list of contacts on the Contact Us page on the Provider Information website. Find the Contact Us and other resources under the Site Index in the left menu.
Manual Maintenance
Manuals must be kept current.
Notification of manual updates are provided through the weekly web postings under “Recent Website Posts” on the home page of the provider website and under Provider Notices on the provider type page of the provider website. Older versions of the manual may be found through the Archive page on the Provider website. Printing the manual material found at this website for long-term use is not advisable. Department Policy material is updated periodically and it is the responsibility of the users to check and make sure that the policy they are researching or applying has the correct effective date for their circumstances.
Rule References
Providers, office managers, billers, and other medical staff must be familiar with current rules and regulations governing the Montana Medicaid program. Provider manuals are to assist providers in billing Medicaid; they do not contain all Medicaid rules and regulations. Rule citations in the text are a reference tool; they are not a summary of the entire rule. In the event that a manual conflicts with a rule, the rule prevails. Links to rules are available on the Provider Information website. Paper copies of rules are available through the Secretary of State’s office.
NOTE: Providers are responsible for knowing and following current laws and regulations
In addition to the general Medicaid rules outlined in the General Information for Providers manual, the following rules and regulations are also applicable to the physician related services programs:
- Code of Federal Regulations (CFR)
- 42 CFR 410 Supplementary Medical Insurance (SMI) Benefits
- 42 CFR 440 Services: General Provisions
- 42 CFR 441 Services: Requirements and Limits Applicable to Specific Services
- Montana Code Annotated (MCA)
- MCA Title 37-2-101 – 37-2-313 General Provisions Relating to Healthcare Practitioners
- MCA 37-3-101 – MCA 37-3-405 Medicine
- MCA 37-6-101 – MCA 37-6-312 Podiatry
- MCA 37-14-101 – MCA 37-14-102 Radiologic Technologists
- MCA 37-34-101 – MCA 37-34-307 Clinical Lab Science Practitioners
- Administrative Rules of Montana (ARM)
- ARM 37.85.220 Independent Diagnostic Testing Facilities
- ARM 37.86.101 – ARM 37.86.105 Physician Services
- ARM 37.86.201 – ARM 37.86.205 Mid-Level Practitioner Services
- ARM 37.86.501 – ARM 37.86.506 Podiatry Services
- ARM 37.86.3201 – ARM 37.86.3205 Non-Hospital Laboratory and Radiology (X-Ray) Services
- ARM 37.86.1401 – ARM 38.86.1406 Clinic Services
Claims Review (MCA 53-6-111, ARM 37.85.406)
The Department is committed to paying Medicaid providers’ claims as quickly as possible. Medicaid claims are electronically processed and usually are not reviewed by medical experts prior to payment to determine if the services provided were appropriately billed. Although the computerized system can detect and deny some erroneous claims, there are many erroneous claims it cannot detect. For this reason, payment of a claim does not mean the service was correctly billed or the payment made to the provider was correct. Periodic retrospective reviews are performed that may lead to the discovery of incorrect billing or incorrect payment. If a claim is paid, and the Department later discovers the service was incorrectly billed or paid or the claim was erroneous in some other way, the Department is required by Federal regulation to recover any overpayment, regardless of whether the incorrect payment was the result of Department or provider error or other cause (42 CFR 456.3).
Getting Questions Answered
The provider manuals are designed to answer most questions; however, questions may arise that require a call to a specific group (such as a program officer, provider relations, or a prior authorization unit). Medicaid manuals, provider notices, fee schedules, forms, and more are available on the Provider Information website.
End of Introduction Chapter
Covered Services
Montana Medicaid covers almost all services provided by physicians, mid-level practitioners, and podiatrists, including preventive care.
This chapter provides covered services information that applies specifically to services performed by physicians, mid-level practitioners, podiatrists, mid-level practitioners within public health clinics, family planning clinics, independent labs, independent imaging facilities, and independent diagnostic testing facilities. Like all healthcare services received by Medicaid members, services provided by these practitioners must also meet the general requirements listed in the Provider Requirements chapter of the General Information for Providers manual.
Services within Scope of Practice (ARM 37.85.401)
Services are covered only when they are within the scope of the provider’s license. As a condition of participation in the Montana Medicaid program, all providers must comply with all applicable state and federal statutes, rules, and regulations.
Services Provided by Physicians (ARM 37.86.101–105)
Physician services are those services provided by individuals licensed under the State Medical Practice Act to practice medicine or osteopathy, which as defined by state law, are within the scope of their practice.
Services Provided by Mid-Level Practitioners (ARM 37.86.201–205)
Mid-level practitioners include physician assistants licensed to practice medicine by the Montana Board of Medical Examiners and advanced practice registered nurses licensed to practice medicine by the Montana Board of Nursing. Advanced practice registered nurses include nurse anesthetists, nurse practitioners, clinical nurse specialists, and certified nurse midwives. Mid-level practitioners also include practitioners outside Montana who hold appropriate licenses in their own states. A mid-level practitioner must bill under his/her own NPI and taxonomy code, rather than under a physician’s. See the Billing Procedures chapter in this manual.
Services Provided by Podiatrists (ARM 37.86.501–506)
Podiatry services are those services provided by individuals licensed under state law to practice podiatry. Refer to Routine Podiatric Care in this chapter and the podiatrist fee schedule. Locate the Podiatrist Page and fee schedule on the Provider Website by visiting the Resources by Provider Type page.
Services Provided by Independent Labs (ARM 37.86.3201–3205)
Medicaid covers tests provided by independent (non-hospital) clinical laboratories when the following requirements are met:
- Services are ordered and provided by physicians, dentists, or other providers licensed within the scope of their practice as defined by law. Medicaid does not cover lab services ordered by chiropractors.
- Services are provided in an office or other similar facility, but not in a hospital outpatient department or clinic.
- Providers of lab services must be Medicare-certified.
- Providers of lab services must have a current Clinical Laboratory Improvement Amendments (CLIA) certification number. CLIA certification may be obtained in Montana through the Department. See the Contact Us link in the site index in the Provider Information website left menu.
- Medicaid does not cover reference lab services. Providers may bill Medicaid only for those lab services they have performed themselves. Modifier 90, used to indicate reference lab services, is not covered by Medicaid.
Services Provided by Independent Imaging Facilities (ARM 37.86.3201–3205)
Medicaid covers tests provided by independent (non-hospital) imaging facilities when the following requirements are met:
- Services are ordered and provided by physicians, dentists, or other providers licensed within the scope of their practices as defined by law.
- Services are provided in an office or similar facility, but not in a hospital outpatient department or clinic.
- Imaging providers must be supervised by a physician licensed to practice medicine within the state the services are provided.
- Imaging providers must meet state facility licensing requirements. Facilities must also meet any additional federal or state requirements that apply to specific tests (e.g., mammography). All facilities providing screening and diagnostic mammography services are required to have a certificate issued by the Federal Food and Drug Administration (FDA). For more information contact the FDA at 1-800-838-7715.
- For most imaging services and some other tests, the fee schedules show different fees depending on whether the practitioner provided only the technical component (performing the test), only the professional component (interpreting the test), or both components (also known as the global service). Practitioners must bill only for services they provided.
- Technical components of imaging services must be performed by appropriately licensed staff (e.g., x-ray technician) operating within the scope of their practice as defined by state law and under the supervision of a physician.
Services Provided by Independent Diagnostic Testing Facilities (ARM 37.85.220)
- Medicaid covers diagnostic testing services provided by independent diagnostic testing facilities (IDTF) under the supervision of a physician. (See the IDTF fee schedule.)
- Services may be performed in either a fixed location or mobile facility, but must be independent of a hospital.
- Before enrolling in Medicaid, IDTFs must be enrolled in Medicare.
Services Provided by Public Health Clinics (ARM 37.86.1401–1406)
- Public health clinic services are physician and mid-level practitioner services provided in a clinic designated by the Department as a public health clinic.
- Services must be provided directly by a physician or by a public health nurse under a physician’s immediate supervision (i.e., the physician has seen the patient and ordered the service).
- Minimal services are covered when provided by a registered nurse operating under protocols. These services do not require that the physician see the patient.
Services Provided by Mobile Imaging/Portable X-ray Supplier (ARM 37.85.219 )
Medicaid covers tests provided by a mobile imaging provider when the following requirements are met:
- Services are ordered by physicians or other providers licensed within the scope of their practices as defined by law.
- Services are provided at a patient’s locations such as home or nursing home.
- Providers must be enrolled in the federal Medicare program as a mobile imaging/portable X-ray supplier and certified by the DPHHS Quality Assurance Division.
- Providers must be enrolled with Montana Healthcare Programs.
- Mobile imaging providers must be supervised by a physician licensed to practice medicine within the state the services are provided.
- Services are provided by qualified X-ray technologists.
Services Provided by Licensed Direct Entry Midwife (ARM 37.86.1201 )
Medicaid covers services provided by a licensed direct entry midwife when the following requirements are met:
- Must be licensed by Montana Department of Labor and Industry.
- Services include prenatal and delivery or postpartum care only.
- Services must be performed in birthing center.
Non-Covered Services (ARM 37.85.207 and ARM 37.86.205)
Some services not covered by Medicaid include the following:
- Acupuncture
- Naturopath services
- Surgery for weight loss (gastric bypass, banding and other bariatric surgery)
- Services provided by surgical technicians who are not physicians or mid-level practitioners
- Services considered experimental or investigational
- Services provided to Medicaid members who are absent from the state, with the following exceptions:
- Medical emergency
- Required medical services are not available in Montana. Prior authorization may be required. See the Prior Authorization chapter in this manual and the Prior Authorization Information page found under the index in the left menu on the Provider Information website.
- The Department has determined that the general practice for members in a particular area of Montana is to use providers in another state.
- Out-of-state medical services and all related expenses are less costly than in-state services. Check the physician’s fee schedule to determine if the code is covered.
- Montana makes adoption assistance or foster care maintenance payments for a member who is a child residing in another state.
- Medicaid does not cover services that are not direct patient care such as the following:
- Missed or canceled appointments
- Mileage and travel expenses for providers
- Preparation of medical or insurance reports
- Service charges or delinquent payment fees
- Telephone services in home
- Remodeling of home
- Plumbing service
- Car repair and/or modification of automobile
Importance of Fee Schedules
The easiest way to verify coverage for a specific service is to check the Department’s fee schedule for your provider type. Fee schedules list Medicaid covered codes and provide clarification of indicators such as whether a code requires prior authorization, can be applied to a co-surgery, or can be billed bilaterally, etc. In addition to being listed on the fee schedule, all services provided must also meet the coverage criteria listed in the Provider Requirements chapter of the General Information for Providers manual and in this chapter. Use the fee schedule in conjunction with the more detailed coding descriptions listed in the CPT, HCPCS, and ICD coding books. Take care to use the fee schedule and coding books that pertain to the date of service.
NOTE: Use the current fee schedule for your provider type to verify coverage for specific services.
Fee schedules are available on the Provider Information website listed under each provider type page.
Locate Provider type pages on the Provider Website under "Resources by Provider Type".
Locate Physician Fee Schedules and ATP Tests and Fees Fee Schedules on the Physician Provider Type page.
Coverage of Specific Services
The following are coverage rules for specific services provided by physicians, mid-level practitioners, and podiatrists.
Abortions (ARM 37.86.104)
Abortions are covered when one of the following conditions is met:
- The member’s life would be endangered if the fetus is carried to term.
- The pregnancy is the result of rape or incest.
- The abortion is determined by the attending physician to be medically necessary, even if the member’s life is not endangered if the fetus is carried to term.
A completed Medicaid Healthcare Programs Physician Certification for Abortion Services (MA-37) form must be submitted with every abortion claim or payment will be denied. This form is the only form Medicaid accepts for abortion services. Complete only one section of this form.
When using mifepristone (Mifeprex or RU 486) to terminate a pregnancy, it must be administered within 49 days from the beginning of the last menstrual period by or under the supervision of a physician who:
- Can assess the duration of a pregnancy.
- Can diagnose ectopic pregnancies.
- Can provide surgical intervention in cases of incomplete abortion or severe bleeding, or can provide such care through other qualified physicians.
- Can assure access to medical facilities equipped to provide blood transfusion and resuscitation.
- Has read, understood, and explained to the member the prescribing information for mifepristone.
Cosmetic Services (ARM 37.86.104)
Medicaid covers cosmetic services only when the condition has a severe detrimental effect on the member’s physical and psychosocial well-being. Mastectomy and reduction mammoplasty services are covered only when medically necessary. Medical necessity for reduction mammoplasty is related to signs and symptoms resulting from macromastia. Medicaid covers surgical reconstruction following breast cancer treatment. Before cosmetic services are performed, they must be prior authorized. Services are authorized on a case-by-case basis. ( See the Prior Authorization Information on the Contact Us link located in the site index in the left menu of the Provider Website.
Early and Periodic Screening, Diagnostic, and Treatment (EPSDT) Services (ARM 37.86.2201–2235) Program
The EPSDT program covers all medically necessary services for children ages 20 and under. Providers are encouraged to use a series of screening and diagnostic procedures designed to detect diseases, disabilities, and abnormalities in the early stages. (See the EPSDT Well-Child chapter in the General Information for Providers manual. ) Some services are covered for children that are not covered for adults, such as the following:
- Nutritionist services
- Private duty nursing
- Respiratory therapy
- Therapeutic family and group home care
- Substance dependency inpatient and day treatment services
- School-based services
All prior authorization and Passport approval requirements must be followed. See the Prior Authorization chapter in this manual and the Passport to Health manual.
Family Planning Services (ARM 37.86.1701)
Family planning services include the following:
- Annual visit
- Comprehensive history
- Initial physical examination
- Initial visit
- Laboratory services
- Medical counseling
- Routine visits
Medicaid covers prescription contraceptive supplies, implantation, or removal of subcutaneous contraceptives, and fitting or removal of an IUD and fitting of a diaphragm. Approval by the Passport provider is not required for family planning services. See the Submitting a Claim chapter in this manual for Passport indicators. Specific billing procedures must be followed for family planning services. ( See Billing Procedures.)
Home Obstetrics (ARM 37.85.207)
Home deliveries are only covered on an emergency basis by a physician or licensed midwife. Home deliveries are those delivery services not provided in a licensed healthcare facility or nationally accredited birthing center and necessary to protect the health and safety of the woman and fetus from the onset of labor through delivery.
Immunizations
The Vaccines for Children (VFC) program makes selected vaccines available at no cost to providers for eligible children 18 years old and under. Medicaid will therefore pay only for the administration of these vaccines (oral, nasal, or injection) and only the federal mandated rate. VFC covered vaccines may quarterly. For more information on the VFC program and current VFC covered vaccines, call the Department’s Immunization program at (406) 444-5580, or refer to the most recent VFC provider notice.
Medicaid does not cover pneumonia and flu vaccines for members with Medicare Part B insurance because Medicare covers these immunizations. Other vaccines for Medicare patients should be billed through Medicare Part D.
Infertility (ARM 37.85.207)
Medicaid does not cover treatment services for infertility, including sterilization reversals.
Prescriptions (ARM 37.86.1102)
For detailed information about prescription drugs, refer to the Prescription Drug Program manual on the Pharmacy page of the website.
The page can be located by choosing the Resources by Provider Type link from the home page of the Provider Website.
The DUR Board has set monthly limits on certain drugs. Use over these amounts requires prior authorization. Refer to the Prior Authorization chapter of the Prescription Drug Program manual for limits.
Routine Podiatric Care
Medicaid pays for routine podiatric care when a medical condition affecting the legs or feet (such as diabetes or arteriosclerosis obliterans) requires treatment by a physician or podiatrist. Routine podiatric care includes the following:
- Cutting or removing of corns and calluses
- Trimming of nails
- Application of skin creams
- Debridement of nails
- Other hygienic or preventive maintenance care
Sterilization (ARM 37.86.104)
Elective Sterilization
Elective sterilizations are sterilizations done for the purpose of becoming sterile. Medicaid covers elective sterilization for men and women when all of the following requirements are met:
- Member must complete and sign the Informed Consent to Sterilization (MA-38 or HHS 687) form at least 30 days, but not more than 180 days, prior to the sterilization procedure. These forms are the only forms Medicaid accepts for elective sterilizations. If one of these forms is not properly completed, payment will be denied. See the Forms page on the Provider Information website for the forms and instructions for completion. Locate the Forms page by choosing the Forms link on the home page of the provider website.
- Member must be at least 21 years of age when signing the form.
- Member must not have been declared mentally incompetent by a federal, state, or local court, unless the member has been declared competent to specifically consent to sterilization.
- Member must not be confined under civil or criminal status in a correctional or rehabilitative facility, including a psychiatric hospital or other correctional facility for the treatment of the mentally ill.
The 30-day waiting period may be waived for either of the following reasons:
- Premature Delivery. The Informed Consent to Sterilization must be completed and signed by the member at least 30 days prior to the estimated delivery date and at least 72 hours prior to the sterilization.
- Emergency Abdominal Surgery. The Informed Consent to Sterilization form must be completed and signed by the member at least 72 hours prior to the sterilization procedure.
All forms required for sterilizations can be downloaded from the Provider Information website, Locate the Forms page by choosing the Forms link on the home page of the provider website.
Before performing a sterilization, the following requirements must be met:
- The member must have the opportunity to have questions regarding the sterilization procedure answered to his/her satisfaction.
- The member must be informed of his/her right to withdraw or withhold consent anytime before the sterilization without being subject to retribution or loss of benefits.
- The member must be made aware of available alternatives of birth control and family planning.
- The member must understand the sterilization procedure being considered is irreversible.
- The member must be made aware of the discomforts and risks which may accompany the sterilization procedure being considered.
- The member must be informed of the benefits and advantages of the sterilization procedure.
- The member must know that he/she must have at least 30 days to reconsider his/her decision to be sterilized.
- An interpreter must be present to translate or sign for those members who are blind, deaf, or do not understand the language to assure the person has been informed.
Informed consent for sterilization may not be obtained under the following circumstances:
- If the member is in labor or childbirth.
- If the member is seeking or obtaining an abortion.
- If the member is under the influence of alcohol or other substance which affects his/her awareness.
Medically Necessary Sterilization
When sterilization results from a procedure performed to address another medical problem, it is considered a medically necessary sterilization. These procedures include hysterectomies, oophorectomies, salpingectomies, and orchiectomies. Every claim submitted to Medicaid for a medically necessary sterilization must be accompanied by one of the following:
- A completed Medicaid Hysterectomy Acknowledgement form (MA-39) for each provider submitting a claim. It is the provider’s responsibility to obtain a copy of the form from the primary or attending physician. Complete only one section of this form. When no prior sterility (Section B) or life-threatening emergency (Section C) exists, the member (or representative, if any) and physician must sign and date Section A of this form prior to the procedure. (See 42 CFR 441.250 for the federal policy on hysterectomies and sterilizations.) Also, for Section A, signatures dated after the surgery date require manual review of medical records by the Department. The Department must verify that the member (and representative, if any) was informed orally and in writing, prior to the surgery, that the procedure would render the member permanently incapable of reproducing. The member does not need to sign this form when Sections B or C are used. Refer to the Forms page on the Provider Information website for instructions on completing the form.
- For members who have become retroactively eligible for Medicaid, the physician must certify in writing that the surgery was performed for medical reasons and must document one of the following:
- The individual was informed prior to the hysterectomy that the operation would render the member permanently incapable of reproducing.
- The reason for the hysterectomy was a life-threatening emergency.
- The member was already sterile at the time of the hysterectomy and the reason for prior sterility.
NOTE: A notation Not a Sterilization on a claim is not sufficient to fulfill these certification requirements.
When submitting claims for retroactively eligible members, attach a copy of the Notice of Retroactive Eligibility (Form 160-M) to the claim if the date of service is more than 12 months earlier than the date the claim is submitted.
Surgical Services
- The fee schedule shows Medicaid policies code by code on global periods, bilateral procedures, assistants at surgery, co-surgeons, and team surgery. These policies are almost always identical to Medicare policies but in cases of discrepancy, the Medicaid policy applies.
- Medicaid only covers assistant at surgery services when provided by physicians or mid-level practitioners who are Medicaid providers.
- Medicaid does not cover surgical technician services.
- See the Billing Procedures chapter regarding the appropriate use of modifiers for surgical services.
Telemedicine Services
Please refer to the Telemedicine section of the General Information for Providers Manual.
Transplants
- All Medicaid transplant services must be prior authorized. See the Prior Authorization Information page. Locate the Prior Authorization page in the Site Index in the left menu of the Provider Website.
- All transplants must be medically necessary.
- Each case receives individualized review and is evaluated for medical suitability.
Weight Reduction
- Physicians and mid-level practitioners who counsel and monitor members on weight reduction programs can be paid for those services. If medical necessity is documented, Medicaid will also cover lab work. Similar services provided by nutritionists are not covered for adults.
- Medicaid does not cover the following weight reduction services:
- Weight reduction plans/programs (e.g., Jenny Craig, Weight Watchers)
- Nutritional supplements
- Dietary supplements
- Health club memberships
- Educational services of nutritionists
End of Covered Services Chapter
Prior Authorization
Prior authorization refers to a list of services that require approval from the Medicaid program prior to the service being rendered. If a service requires prior authorization, the requirement exists for all Medicaid members. When prior authorization is granted, a prior authorization number is issued and must be on the claim.
Different codes are issued for Passport approval and prior authorization; when necessary, both must be on the claim form. Medicaid does not pay for services when prior authorization requirements are not met.
Prior Authorization for Retroactively Eligible Members
When a member is determined retroactively eligible for Medicaid, the member should give the provider a Notice of Retroactive Eligibility (160-M). The provider has 12 months from the date retroactive eligibility was determined to bill for those services. When a member becomes retroactively eligible for Medicaid the provider may:
- Accept the member as a Medicaid member from the current date.
- Accept the member as a Medicaid member from the date retroactive eligibility was effective.
- Require the member to continue as a private-pay member.
Providers may choose whether to accept retroactive eligibility. All prior authorization requirements must be met to receive Medicaid payment. When requesting prior authorization, attach a copy of the 160-M to the prior authorization request. It is the member’s responsibility to ensure his/her caseworker prepares an 160-M for each provider who participates in the member’s healthcare during this retroactive period. See the Billing Procedures chapter in this manual for retroactive eligibility billing requirements. When seeking prior authorization, keep in mind the following:
- The referring provider should initiate all authorization requests.
- Always refer to the current Medicaid fee schedule to verify if prior authorization is required for specific services.
- For a list of services that require prior authorization, who to contact, and documentation requirements, see the Contact Us link in site index in the Provider Information website menu. The Contact Us can be located in the site index in the left menu of the Provider Website.
- Prior authorization criteria forms for most services are available on the Forms page of the Provider Information website .
- When prior authorization is granted from Mountain-Pacific Quality Health (MPQH), providers receive notification from both MPQH and Conduent Claims Processing. The Prior Authorization Notice from Claims Processing has a prior authorization number which must be included on the claim.
End of Prior Authorization Chapter
Coordination of Benefits
Medicaid members often have coverage though Medicare, workers’ compensation, employment-based coverage, individually purchased coverage, etc. Coordination of benefits is the process of determining which source of coverage is the primary payer in a particular situation. In general, providers must bill other carriers before billing Medicaid, but there are some exceptions. (See Exceptions to Billing Third Party First later in this chapter.) Medicare coverage is processed differently than other sources of coverage.
Identifying Other Sources of Coverage
The member’s Medicaid eligibility information may list other payers such as Medicare or other third party payers. (See Member Eligibility and Responsibilities in the General Information for Providers manual.) If a member has Medicare, the Medicare ID number is listed on the eligibility verification. If a member has other coverage (excluding Medicare), it will be shown also. Some examples of third party payers include:
- Private health insurance
- Employment-related health insurance
- Workers’ compensation insurance*
- Health insurance from an absent parent
- Automobile insurance*
- Court judgments and settlements*
- Long-term care insurance
*These third party payers (and others) may not be listed on the member’s Medicaid eligibility information.
Providers must use the same procedures for locating third party sources for Medicaid members as for their non-Medicaid members. Providers cannot refuse service because of a third party payer or potential third party payer.
When a Member Has Medicare
Medicare claims are processed and paid differently than claims involving other payers. The other sources of coverage are referred to as third party liability (TPL), but Medicare is not.
Medicare Part A Claims
Medicare Part A covers inpatient hospital care, skilled nursing care, and other services. Medicare Part A carriers and Medicaid use electronic exchange of institutional claims covering Part A services. Providers must submit these claims first to Medicare. After Medicare processes the claim, an Explanation of Medicare Benefits (EOMB) is sent to the provider. The provider then reviews the EOMB and submits the claim to Medicaid.
Medicare Part B Crossover Claims
Medicare Part B covers outpatient hospital care, physician care and other services. Although outpatient hospital care is covered under Part B, it is processed by Medicare Part A. The Department has an agreement with Medicare Part B carriers for Montana (Noridian) and the Durable Medical Equipment Regional Carrier [DMERC]. Under this agreement, the carriers provide the Department with claims for members who have both Medicare and Medicaid coverage. Providers must tell Medicare that they want their claims sent to Medicaid automatically and must have their Medicare provider number on file with Medicaid.
NOTE: To avoid confusion and paperwork, submit Medicare Part B crossover claims to Medicaid only when necessary.
In these situations, providers need not submit Medicare Part B crossover claims to Medicaid. Medicare will process the claim, submit it to Medicaid, and send the provider an EOMB. Providers must check the EOMB for the statement indicating that the claim has been referred to Medicaid for further processing. It is the provider’s responsibility to follow up on crossover claims and make sure they are correctly billed to Medicaid within the timely filing limit. (See the Billing Procedures chapter.)
When Medicare Pays or Denies a Service
- When Medicare automatic crossover claims are paid or denied, they should automatically cross over to Medicaid for processing, so the provider does not need to submit the claim to Medicaid.
- When Medicare crossover claims are billed on paper and are paid or denied, the provider must submit the claim to Medicaid with the Medicare EOMB (and the explanation of denial codes).
When Medicaid Does Not Respond to Crossover Claims
When Medicaid does not respond within 45 days of the provider receiving the Medicare EOMB, submit a claim and a copy of the Medicare EOMB to Medicaid for processing.
NOTE: When submitting electronic claims with paper attachments, see the Billing Electronically with Paper Attachments section of the Billing Procedures chapter in this manual.
Submitting Medicare Claims to Medicaid
When submitting a claim to Medicaid, include the Medicare EOMB and use Medicaid billing instructions and codes. Medicare’s instructions, codes, and modifiers may not be the same as Medicaid’s. The claim must also include the Medicaid provider number and Medicaid member ID number.
Submit Medicare crossover claims to Medicaid only when:
- The referral to Medicaid statement is missing from the provider’s EOMB.
- The provider does not hear from Medicaid within 45 days of receiving the Medicare EOMB.
- Medicare denies the claim.
When a Member Has TPL (ARM 37.85.407)
When a Medicaid member has additional medical coverage (other than Medicare), the other insurance is often referred to as third party liability (TPL). In most cases,the providers must bill other insurance carriers before billing Medicaid.
Providers are required to notify their members that any funds the member receives from third party payers (when the services were billed to Medicaid) must be turned over to the Department. The following words printed on the member’s statement will fulfill this requirement: When services are covered by Medicaid and another source, any payment the member receives from the other source must be turned over to Medicaid.
Exceptions to Billing Third Party First
In a few cases, providers may bill Medicaid first.
- When a Medicaid member is also covered by Indian Health Service (IHS) or the Montana Crime Victims Compensation Fund, providers must bill Medicaid first. These are not considered third party liability.
- When a member has Medicaid eligibility and Mental Health Services Plan (MHSP) eligibility for the same month, Medicaid must be billed first.
- ICD prenatal and ICD preventive pediatric diagnosis conditions may be billed to Medicaid first. In these cases, Medicaid will pay-and-chase or recover payment from the third party payer.
- The following services may also be billed to Medicaid first:
- Audiology
- Dental (as billed on dental claim)
- Drugs (as billed on drug claims)
- Eyeglasses
- Hearing aids and batteries
- Home and community-based services (waiver)
- Nursing facility (as billed on nursing home claims)
- Optometry
- Oxygen in a nursing facility
- Personal assistance
- Transportation (other than ambulance)
- If the third party has only potential liability, the provider may bill Medicaid first. Do not indicate the potential third party on the claim. Instead, notify the Department of the potential third party by sending the claim and notification directly to the Third Party Liability Unit.
Requesting an Exemption
Providers may request to bill Medicaid first under certain circumstances. In each of these cases, the claim and required information must be sent directly to the Third Party Liability Unit.
- When a provider is unable to obtain a valid assignment of benefits, the provider must submit the claim with documentation that the provider attempted to obtain assignment and certification that the attempt was unsuccessful.
- When the Child Support Enforcement Division has required an absent parent to have insurance on a child, the claim can be submitted to Medicaid when the following requirements are met:
- The third party carrier has been billed, and 30 days or more have passed since the date of service.
- The claim is accompanied by a certification that the claim was billed to the third party carrier, and payment or denial has not been received.
- If another insurance has been billed, and 90 days have passed with no response, attach a note to the claim explaining that the insurance company has been billed or attach a copy of the letter sent to the insurance company. Include the date the claim was submitted to the insurance company and certification that there has been no response.
- When the provider has billed the third party insurance and has received a non-specific denial (e.g., no member name, date of service, amount billed), submit the claim with a copy of the denial and a letter of explanation directly to Medicaid in order to avoid missing the timely filing deadline.
When the Third Party Pays or Denies a Service
When a third party payer is involved (excluding Medicare) and the other payer:
- Pays the claim, indicate the amount paid in the “amount paid” field of the claim when submitting to Medicaid for processing. These claims may be submitted either electronically or on paper.
- Allows the claim, and the allowed amount went toward member's deductible, include the insurance Explanation of Benefits (EOB) when billing Medicaid.
- Denies the claim, include a copy of the denial (including the reason explanation) with the claim, and submit to Medicaid.
- Denies a line on the claim, bill the denied lines together on a separate claim and submit to Medicaid. Include the explanation of benefits (EOB) from the other payer as well as an explanation of the reason for denial (e.g., definition of denial codes).
When the Third Party Does Not Respond
If another insurance has been billed, and 90 days have passed with no response, bill Medicaid as follows:
- Attach a note to the claim explaining that the insurance company has been billed, or attach a copy of the letter sent to the insurance company.
- Include the date the claim was submitted to the insurance company.
- Send this information to the Conduent Third Party Liability Unit.
Other Programs
The information covered in this chapter also applies to members enrolled in the Mental Health Services Plan (MHSP) and Healthy Montana Kids (HMK) dental and vision providers.
End of Coordination of Benefits
Billing Procedures
Claim Forms
Services provided by the healthcare professionals covered in this manual must be billed either electronically on a professional claim 837P or on a CMS-1500 paper claim form. CMS-1500 forms are available from various publishing companies; they are not available from the Department or Provider Relations.
Timely Filing Limits (ARM 37.85.406)
Providers must submit clean claims to Medicaid within:
- Twelve months from the latest of:
- the date of service;
- the date retroactive eligibility is determined; or
- the date disability was determined;
- Six months from the date on the Medicare explanation of benefits approving the service, if the Medicare claim was timely filed and the recipient was Medicare eligible at the time the Medicare claim was filed; or
- Six months from the date on an adjustment notice from a third party payor, where the third party payer has previously processed the claim for the same service and the adjustment notice is dated after the periods described above.
Clean claims are claims that can be processed without additional information or action from the provider. The submission date is defined as the date that the claim was received by the Department or the claims processing contractor. All problems with claims must be resolved within this 12-month period.
Tips to Avoid Timely Filing Denials
- Correct and resubmit denied claims promptly. ( See the Remittance Advices and Adjustments chapter in the General Information for Providers manual.)
- If a claim submitted to Medicaid does not appear on the remittance advice within 30 days, contact Provider Relations for claim status.
- If another insurer has been billed and 90 days have passed with no response, you can bill Medicaid. ( See the Coordination of Benefits chapter in this manual for more information.)
- To meet timely filing requirements for Medicare/Medicaid crossover claims, see the Coordination of Benefits chapter in this manual.
When to Bill Medicaid Members (ARM 37.85.406)
In most circumstances, providers may not bill Medicaid members for services covered under Medicaid. The main exception is that providers may collect cost sharing from members.
More specifically, providers cannot bill members directly:
- For the difference between charges and the amount Medicaid paid.
- For a covered service provided to a Medicaid-enrolled member who was accepted as a Medicaid member by the provider, even if the claim was denied.
- When the provider bills Medicaid for a covered service, and Medicaid denies the claim because of billing errors.
- When a third party payer does not respond.
- When a member fails to arrive for a scheduled appointment.
- When services are free to the member and free to non-Medicaid covered individuals, such as in a public health clinic.
Under certain circumstances, providers may need a signed agreement to bill a Medicaid member (see the following table).
Providers may bill a member when:
Patient is Medicaid enrolled and provider accepted them as a Medicaid member
- If the service is covered by Medicaid, the provider can bill the member only for cost sharing.
- If the service is not covered by Medicaid, the provider can bill the member only if a custom agreement was signed between the member and the provider before the service was performed.
Patient is Medicaid enrolled and provider did not accept them as a Medicaid member
- The provider can bill the member only if a custom agreement was signed between the member and the provider before the service was performed.
Patient is not Medicaid Enrolled
- The provider may bill the patient.
NOTE: If a provider bills Medicaid and the claim is denied because the member is not eligible, the provider may bill the member directly.
Private-Pay Agreement: This may be a private-pay agreement between the provider and member that states that the member is not accepted as a Medicaid member, and that he/she must pay for the services received.
Custom Agreement: This agreement lists the service the member is receiving and states that the service is not covered by Medicaid and that the member will pay for the service. See the Custom Agreement for Medicaid non-covered service agreement under the Forms button found on the home page of the provider website.
Member Cost Sharing (ARM 37.85.204 and ARM 37.85.402)
When Members Have Other Insurance
If a Medicaid member is also covered by Medicare, has other insurance, or some other third party is responsible for the cost of the member’s healthcare, see the Coordination of Benefits chapter in this manual.
Billing for Retroactively Eligible Members
When the provider accepts the member’s retroactive eligibility, the provider has 12 months from the date retroactive eligibility was determined to bill for those services. When submitting claims for retroactively eligible members in which the date of service is more than 12 months earlier than the date the claim is submitted, attach a copy of the Provider Notice of Eligibility (Form 160-M). The provider must request the form from the member’s local Office of Public Assistance. See https://dphhs.mt.gov/hcsd/OfficeofPublicAssistance.
For more information on retroactive eligibility, see the Member Eligibility and Responsibilities chapter in the General Information for Providers manual.
Place of Service
Place of service must be entered correctly on each line. Medicaid typically reduces payment for services provided in hospitals and ambulatory surgical centers since these facilities typically bill Medicaid separately for facility charges.
Physician clinics that are affiliated with hospitals should be particularly careful. If the Department has granted a clinic provider-based status then the hospital can bill for facility charges even if the clinic is not on the hospital campus. In these situations the clinic must show outpatient (22) as the place of service.
Multiple Visits (E/M Codes) on Same Date
Medicaid generally covers only one visit (or hospital admission) per member per day. When a member requires additional visits on the same day, use a modifier to describe the reason for multiple visits. When a modifier is not appropriate for the situation, attach documentation of medical necessity to the claim, and submit it to the appropriate Department program officer.
Coding
Standard use of medical coding conventions is required when billing Medicaid. Provider Relations or the Department cannot suggest specific codes to be used in billing for services. For coding resources, see the table of Coding Resources section below.
The following suggestions may help reduce coding errors and unnecessary claim denials:
- Use current CPT, HCPCS, and ICD diagnosis coding books.
- Always read the complete description and guidelines in the coding books. Relying on short descriptions can result in inappropriate billing.
- Attend classes on coding offered by certified coding specialists.
- Use specific codes rather than miscellaneous codes.
- Follow CPT guidelines on the difference between a new patient and an established patient.
- Bill for the appropriate level of service provided.
- Services covered within global periods for certain CPT procedures are not paid separately and must not be billed separately. Most surgical and obstetric procedures and some medical procedures include routine care before and after the procedure. Medicaid fee schedules show the global period for each CPT service.
- Use the correct units measurement on claims. In general, Medicaid follows the definitions in the CPT and HCPCS billing manuals. Unless otherwise specified, one unit equals one visit or one procedure. For specific codes, however, one unit may be 15 minutes, a percentage of body surface area, or another quantity. Always check the long text of the code description.
- CPT codes that are billed based on the amount of time spent with the member must be billed with the code that is closest to the time spent. For example, a provider spends 60 minutes with the member. The code choices are 45 to 50 minutes or 76 to 80 minutes. The provider must bill the code for 45 to 50 minutes.
Coding Resources
Please note that the Department does not endorse the products of any particular publisher.
CPT - https://commerce.ama-assn.org/store/
Description:
CPT codes and definitions.
Updated each January.
Contact:
American Medical Association
(800) 621-8335
CPT Assistant - https://commerce.ama-assn.org/store/
Description:
A newsletter on CPT coding issues.
Contacts:
American Medical Association
(800) 621-8335
HCPCS Level II - Available through various publishers and bookstores or from CMS at www.cms.gov.
Description:
HCPCS codes and definitions.
Updated each January and throughout the year.
Contact:
ICD
Description:
ICD diagnosis and procedure code definitions.
Updated each October .
Contact:
Available through various publishers and bookstores.
Miscellaneous - www .shopingenix .com
Description:
Various newsletters and other coding resources.
Contact:
Medicode (Ingenix)
NCCI Policy and Edits Manual - https://www.cms.gov/Medicare/Coding/NationalCorrectCodInitEd/index.html
Description:
This manual contains National Correct Coding Initiative (NCCI) policy and edits, which are pairs of CPT or HCPCS codes that are not separately payable except under certain circumstances. The edits are applied to services billed by the same provider for the same member on the same date of service.
Contact:National Technical Information Service
NOTE: Always refer to the long descriptions in coding books.
Using the Medicaid Fee Schedule
When billing Medicaid, it is important to use the Department’s fee schedule for your provider type in conjunction with the detailed coding descriptions listed in the current CPT and HCPCS diagnosis coding books. In addition to covered services and payment rates, fee schedules often contain helpful information such as appropriate modifiers, global periods, if multiple surgery guidelines apply, if the procedure can be done bilaterally, if an assistant, co-surgeon, or team is allowed for the procedure, if the code is separately billable, and more. Department fee schedules are updated each January and July. Fee schedules are available on the Provider Information website under the Resources by Provider Type button.
Using Modifiers
- Review the guidelines for using modifiers in the CPT, HCPCS, or other helpful resources. Remember to use the modifiers in effect for the date of service of the claim.
- Always read the complete description for each modifier; some modifiers are described in the CPT manual while others are in the HCPCS book.
- The Medicaid claims processing system recognizes three pricing modifiers and one informational modifier per claim line. Providers are asked to place any modifiers that affect pricing in the first three modifier fields.
- When billing with Modifier 50 for bilateral services, put all information on one line with one unit.
- Check the fee schedule to see if Medicaid allows the use of the following modifiers for a particular code: bilateral (50), multiple procedures (51), cosurgery (62), assistant at surgery (80, 81, 82, AS), and team surgery (66).
- Always bill your main surgical procedure code on line 1 of the claim with one unit only. All other subsequent procedures should be billed with the number of units done for each code per line.
- Do not separate out subsequent procedure codes on separate lines. This will cause exact duplicate line denials. Subsequent procedure modifiers should be used when appropriate except when billing add-on codes and Modifier 51 exempt codes.
Billing Tips for Specific Provider Types
Mid-Level Practitioner Billing
Mid-level practitioners must bill under their own NPI and taxonomy number rather than under a physician number.
Physician Billing
Medicaid-enrolled providers may bill for locum tenens physician services when the following criteria are met:
- The regular physician is absent due to illness, pregnancy, vacation or continuing medical education;
- The Medicaid member has arranged or seeks to receive services from the regular physician;
- The regular physician pays the locum tenens for his/her services on a per diem or similar fee-for-time basis;
- The substitute physician does not provide services to Medicaid members over a continuous period of longer than 60 days; and
- Medicaid-enrolled physician may bill locum tenens services using modifier Q6.
Podiatrist Billing
Podiatrists must use appropriate codes and modifiers from their specific fee schedule.
Independent Labs
Independent labs must use appropriate fee schedules, codes, and modifiers for their provider type.
- The provider’s current CLIA certification number must be on file with Provider Relations or all lab claims will be denied. See the Contact Us link on the website for CLIA certification information.
- This requirement also applies to public health labs. Questions regarding public health labs may be directed to the Public Health Lab Assistance hotline. See the Contact Us link on the website.
Independent Diagnostic Testing Facilities (IDTF)
IDTF providers must use appropriate fee schedules, codes and modifiers for their provider type. If an IDTF performs laboratory services, they must enroll as an independent lab in addition to IDTF.
- Repeat modifiers should be used to indicate multiple radiology services of the same radiology code performed on the same day for the same member by the same or different providers. Repeat modifiers are specific modifiers used to indicate that a service is a repeat rather than a duplicate. Examples are Modifiers 76 and 77.
- For multiple radiology services of the same code provided by the same provider on the same date of service, bill the first unit as one unit on one line, followed by additional units of the same code on an additional line with Modifier 76.
- For radiology services of the same code provided by a different provider on the same date of service as another provider, bill all units on one line with Modifier 77.
- If a claim is denied as a duplicate, send copies of the radiology report, the denial statement, and the claim to the appropriate Department program officer for review. ( See the Contact Us link on the website site index , then choose the Lab and Imaging pane.)
- For bilateral x-rays, bill on separate lines, one line with Modifier RT and one line with Modifier LT. The exception would be codes that are described as bilateral in their code description. These are to be billed on one line with one unit.
- Imaging providers must take particular care in the use of modifiers. Modifier TC is used when only the technical portion of the service is provided. The provider who interprets the results uses Modifier 26. When both technical and professional services are performed by the same provider, no modifier is required.
Mobile Imaging/Portable X-ray Supplier
- Mobile imaging providers must utilize modifiers appropriately. Modifier TC is used when only the technical portion of the service is provided. The provider who interprets the results uses Modifier 26. When both technical and professional services are performed by the same provider, no modifier is required.
- R0070 and R0075 must be billed based on the number of members served at one location.
- Modifiers UN, UP, UQ, UR OR US must be billed with R0075, depending on the number of members served at the location.
- Q0092 may be billed for the set-up fee for each imaging procedure furnished to a member as long as X-rays taken at different areas of the member’s body.
RHC/FQHC – Professional Services in Hospitals
RHC and FQHC practitioners (e.g., physicians, mid-level practitioners) performing services in a hospital setting should bill those services using the appropriate manual/rules that apply for that practitioner.
Billing Tips for Specific Services
Abortions
A completed Montana Healthcare Programs Physician Certification for Abortion Services (MA-37) form must be attached to every abortion claim or payment will be denied. This is the only form Medicaid accepts for abortions.
Anesthesia
With the exception of moderate conscious sedation, Montana Medicaid does not allow separate reporting of anesthesia for a medical or surgical procedure when it is provided by the practitioner performing the procedure.
When billing for anesthesia services, the date of service on the claim form must match the date of service that anesthesia was administered. If the surgery overlaps days, then bill the anesthesia only with the start date.
CPT states: For continuous services that last beyond midnight, use the date in which the service began and report the total units of time provided continuously.
The following payment method is used for anesthesia services, regardless of whether the service is billed by an anesthesiologist or another professional. Though the method differs from the RBRVS payment method, the two methods are linked and contain similar provisions.
- Use appropriate CPT anesthesia codes.
- Do not use surgery codes with an anesthesia modifier.
- For services where codes or definitions differ between the CPT and the American Society of Anesthesiologists Relative Value Guide, Medicaid adopts the CPT version.
- Include the total number of minutes on the claim. Medicaid will convert the number of minutes to the number of time units. Do not include the base units on the claim as the claims processing system determines the number of base units. ( See the Submitting a Claim chapter in this manual.)
Bundled Services
Certain services with CPT codes (e.g., telephone advice, some pulse oximetry services) are covered by Medicaid but have a fee of zero. This means that the service is typically bundled with an office visit or other service. Since the bundled service is covered by Medicaid, providers may not bill the member separately for it.
Cosmetic Services
Include the prior authorization number on the claim. ( See the Submitting a Claim chapter in this manual.)
EPSDT Well-Child Screens
- Bill for a complete screen using the appropriate evaluation and management (E/M) code for preventive medicine services.
- When billing for partial screens, use the appropriate preventive medicine code with Modifier 52 (reduced services).
- See also the EPSDT Well-Child chapter in the General Information for Providers manual.
- For well-child EPSDT indicators, see the Submitting a Claim chapter in this manual.
Family Planning Services
Contraceptive supplies and reproductive health items provided free to family planning clinics cannot be billed to Medicaid. When these supplies are not free to the clinic, providers associated with a family planning clinic can bill Medicaid for the following items:
Code - Item
A4266 - Diaphragm
A4267 - Male Condoms
A4268 - Female Condoms
A4269 - Spermicide
S4993 - Oral Contraceptives
340B drugs may be billed for acquisition costs only. For family planning indicators, see the Submitting a Claim chapter in this manual.
Immunizations
Per CPT, Codes 90460 and 90461 replace deleted Code 90465– Code 90468 for Vaccines for Children (VCF), a program for members ages 0–18.
Code 90460 (non-VFC) is billed for the first component of a vaccine. Code 90461 SL is not allowed by the VFC Program.
VFC codes are reviewed quarterly and updates may be implemented; please consult current provider notices to see if there are any changes.
Follow the CPT coding instructions as outlined in the CPT coding book for the proper use of these codes (i.e., face-to-face physician or qualified healthcare counseling time) member age, and add-on coding rules. Also, a combination of these two sets for the same date of service, member, and provider will result in an NCCI denial, with or without an NCCI modifier, because Codes 90471, 90472, 90473, and 90474 are component codes to Codes 90460 and 90461.
You may only bill for administrative services if performed by or under the direct supervision of a reimbursable professional (i.e., physician, mid-level). All administration of VFC vaccines must be billed on a CMS-1500.
The administration codes should have the appropriate modifier (SL) to be reimbursed for the federally mandated administration rate. Codes for the VFC supplied vaccines must be billed on the same claim with no charge ($0.00). See the fee schedule on the Physician page on the Provider Information website.
Note: If a significant separately identifiable Evaluation and Management (E/M) service (e.g., office or other outpatient services, preventive medicine services) is performed, the appropriate E/M service code with the appropriate modifier should be reported in addition to the vaccine and toxoid administrative codes.
Note: Administrative Code 90460 (VFC) may have multiple units per line because the code can be used for all VFCs. Codes 90471, 90473, and 90474 define route of administration.
Note: If a significant separately identifiable E/M service (e.g., office or other outpatient services, preventive medicine services) is performed, the appropriate E/M service code with the appropriate modifier should be reported in addition to the vaccine and toxoid administration codes.
Obstetrical Services
If the provider’s care includes prenatal (antepartum) and/or postnatal (postpartum) care in addition to the delivery, the appropriate global OB code must be billed. Antepartum care includes all visits until delivery, and there are different codes for specified numbers of visits. There are also different codes for antepartum and postpartum care when only one or the other is provided. Please review your CPT coding book carefully.
When billing a medical or surgical procedure, the date of service on the claim form must match the date of service that the procedure was performed. If the procedure has a global component and the provider saw the patient before and after the procedure, then the provider must bill the global procedure code on the claim form with the date associated for services rendered. For instance, if a vaginal delivery with antepartum and postpartum care (CPT 59400) is performed, it must be billed using the date of delivery as the from and to dates of service.
Reference Lab Billing
Under federal regulations, all lab services must be billed to Medicaid by the lab that performed the service. Modifier 90, used to indicate reference lab services, is not covered by Medicaid.
Sterilization
For elective sterilizations, a completed Informed Consent to Sterilization (MA-38) form must be attached to the claim for each provider involved or payment will be denied. No fields may be left blank, except for the Interpreter’s Statement. This form must be legible and accurate. If revisions are made, they must be made with a single line through the incorrect information and initialed by the party making the change. patient information may only be changed by the patient and must be initialed by the patient. Documentation must be included explaining why revisions were made. It is the provider’s responsibility to obtain a copy of the form from the primary or attending physician.
For medically necessary sterilizations (including hysterectomies, oophorectomies, salpingectomies, and orchiectomies), one of the following must be attached to the claim, or payment will be denied:
- A completed Medicaid Hysterectomy Acknowledgement form (MA-39) for each provider submitting a claim. It is the provider’s responsibility to obtain a copy of the form from the primary or attending physician. Complete only one section of this form. When no prior sterility (Section B) or life-threatening emergency (Section C) exists, the member (or representative, if any) and physician must sign and date Section A of this form prior to the procedure (see 42 CFR 441.250 for the federal policy on hysterectomies and sterilizations). Also, for Section A, signatures dated after the surgery date require manual review of medical records by the Department. The Department must verify that the member (and representative, if any) was informed orally and in writing, prior to the surgery, that the procedure would render the member permanently incapable of reproducing. The member does not need to sign this form when Sections B or C are used. Refer to the Forms page on the website for instructions on completing the form.
- For members who have become retroactively eligible for Medicaid, the physician must certify in writing that the surgery was performed for medical reasons and must document one of the following:
- The individual was informed prior to the hysterectomy that the operation would render the member permanently incapable of reproducing.
- The reason for the hysterectomy was a life-threatening emergency.
- The member was already sterile at the time of the hysterectomy and the reason for prior sterility.
When submitting claims for retroactively eligible members, attach a copy of the MA-160 (eligibility determination letter) to the claim if the date of service is more than 12 months earlier than the date the claim is submitted. For more information on sterilizations, see the Covered Services chapter in this manual.Surgical Services Medicaid does not provide additional payment for the operating room in a physician’s office. Medicaid pays facility expenses only to licensed hospitals and ambulatory surgical centers.
Reporting surgical services
Certain surgical procedures must not be reported together, such as:
- Procedures that are mutually exclusive based on the CPT code description or standard medical practice.
- When both comprehensive and component procedures are performed, only the comprehensive procedure should be billed.
- When the CPT manual describes several procedures of increasing complexity, only the code describing the most extensive procedure performed should be reported.
Medicaid edits for some surgical services using Medicaid’s National Correct Coding Initiative (NCCI) edits and performs post-payment review on others. See Coding Resources earlier in this chapter for more information on NCCI.
Assistant at Surgery
When billing for an assistant at surgery, refer to the current Medicaid fee schedule to see if an assist is allowed for that procedure.
If an assistant at surgery does not use the appropriate modifier, then either the assistant’s claim or the surgeon’s claim (whichever is received later) will be denied as a duplicate service.
Physicians must bill assistant at surgery services using the appropriate surgical procedure code and Modifier 80, 81, or 82.
Mid-level practitioners must bill assistant at surgery services under their own NPI and taxonomy using the appropriate surgical procedure code and Modifier AS, 80, 81, or 82.
Global surgery periods: Global surgery periods are time spans assigned to surgery codes. During these time spans, services related to the surgery may not be billed. Group practice members that are of the same specialty must bill Medicaid as if a single practitioner provided all related follow-up services for a member. For example, Dr. Armstrong performs orthopedic surgery on a member. The member comes in for a follow-up exam, and Dr. Armstrong is on vacation. Dr. Armstrong’s partner, Dr. Black, performs the follow-up. Dr. Black cannot bill this service to Medicaid because the service was covered in the global period when Dr. Armstrong billed for the surgery.
For major surgeries, this span is 90 days and includes the day prior to the surgery and the following services: post-operative surgery related care and pain management and surgically-related supplies and miscellaneous services.
For minor surgeries and some endoscopies, the spans are either 1 day or 10 days. They include any surgically related follow-up care and supplies on the day of surgery, and for a 10-day period after the surgery.
For a list of global surgery periods by procedure code, see the current Department fee schedule for your provider type.
If the CPT manual lists a procedure as including the surgical procedure only (i.e., a “starred” procedure) but Medicaid lists the code with a global period, the Medicaid global period applies. Almost all Medicaid fees are based on Medicare relative value units (RVUs), and the Medicare relative value units were set using global periods even for starred procedures. Montana Medicaid has accepted these RVUs as the basis for its fee schedule.
In some cases, a physician (or the physician’s partner of the same specialty in the same group practice) provides care within a global period that is unrelated to the surgical procedure. In these circumstances, the unrelated service must be billed with the appropriate modifier to indicate it was not related to the surgery.
Telemedicine Services
When performing a telemedicine consult, use the appropriate CPT E/M consult code. The place of service is the location of the provider providing the telemedicine service. Medicaid does not pay for network use or other infrastructure charges.
Please refer to the Telemedicine section of the General Information for Providers Manual.
Transplants
Include the prior authorization number on the claim. See the Submitting a Claim chapter in this manual. All providers must have their own prior authorization number for the services. For details on obtaining prior authorization, see the Prior Authorization chapter in this manual.
Weight Reduction
Providers who counsel and monitor members on weight reduction programs must bill Medicaid using appropriate E/M codes.
Unlisted Procedures
Unlisted CPT or HCPCS codes are to be sent to the Department at the address below for review.
Claim Review
Physician-Related Services
P.O. Box 202951
Helena, MT 59624
Submitting Electronic Claims
Providers who submit claims electronically experience fewer errors and quicker payment. Claims may be submitted using the methods below. For detailed submission methods, see the electronic submissions manual on the Electronic Billing page of the website.
- WINASAP 5010. This free software provided by Conduent allows for the creation of basic claim submissions. Please note that this software is not compatible with Windows 10 and has limited support as it is free software.
o Utilizes either a dial-up modem or submissions through the Montana Access to Health (MATH) Web Portal.
o Requires completion of the X12N Transaction Packet to allow for claim submissions.
- Clearinghouses/Contracted Claim Submitter. Providers can make arrangements with a clearinghouse/contracted claim submitter for claim submission. Please note that the clearinghouse must be enrolled to submit claims to Montana Medicaid.
- Montana Access to Health (MATH) Web Portal . A secure website that allows providers to verify eligibility, check claim status, and view medical claims history. Valid X12N files can be uploaded through this website.
o Requires completion of the X12N Transactions Packet to allow for claim submissions.
- MoveIt DMZ. This secure transfer protocol is for providers and clearinghouses that submit large volumes of files (in excess of 20 per day) or are regularly submitting files larger than 2 MB. This utilizes SFTP and an intermediate storage area for the exchange of files.
o A request for this must be made through Conduent Provider Relations for established trading partners.
Providers should be familiar with federal rules and regulations related to electronic claims submission.
Billing Electronically with Paper Attachments
When submitting claims that require additional supporting documentation, the Attachment Control Number field must be populated with an identifier. Identifier formats can be designed by software vendors or clearinghouses, but the preferred method is the provider’s NPI followed by the member’s ID number and the date of service, each separated by a dash:
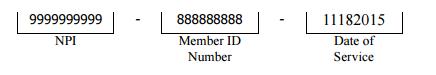
The supporting documentation must be submitted with a Paperwork Attachment Cover Sheet under the forms button on the provider website home page. The number in the paper Attachment Control Number field must match the number on the cover sheet.
Electronic claims that have the PWK indicator will pend for 30 days awaiting the appropriate paperwork to be submitted using the above procedure. If the claim has no PWK indicator, claims will proceed through the normal adjudication process.
Submitting Paper Claims
For instructions on completing a paper claim, see the Submitting a Claim chapter in this manual. Unless otherwise stated, all paper claims must be mailed to:
Claims Processing
P.O. Box 8000
Helena, MT 59604
Claim Inquiries
Contact Provider Relations for general claim questions and questions regarding member eligibility, payments, and denials.
Paper claims are often returned to the provider before they can be processed, and many other claims (both paper and electronic) are denied. To avoid unnecessary returns and denials, double-check each claim to confirm the following items are included and accurate.
How to Avoid the Most Common Billing Errors
Reasons for Return or Denial:
Provider’s NPI and/or taxonomy missing or invalid
Preventing Returned or Denied Claims:
Verify the correct NPI and taxonomy are on the claim.
Reasons for Return or Denial:
Authorized signature missing.
Preventing Returned or Denied Claims:
Each claim must have an authorized signature belonging to the provider, billing clerk, or office personnel. The signature may be typed, stamped, or handwritten.
Reasons for Return or Denial:
Signature date missing.
Preventing Returned or Denied Claims:
Each claim must have a signature date.
Reasons for Return or Denial:
Incorrect claim form used.
Preventing Returned or Denied Claims:
The claim must be the correct form for the provider type. Services covered in this manual require a CMS-1500 claim form (or electronic professional claim).
Reasons for Return or Denial:
Information on claim form not legible.
Preventing Returned or Denied Claims:
Information on the claim form must be legible. Use dark ink and center the information in the field. Information must not be obscured by lines.
Reasons for Return or Denial:
Recipient number not on file, or recipient was not eligible on date of service.
Preventing Returned or Denied Claims:
Before providing services to the member:
View the member’s eligibility information at each visit. Medicaid eligibility may change monthly.
Verify member eligibility by using one of the methods described in the Member Eligibility and Responsibilities chapter of the General Information for Providers manual.
Reasons for Return or Denial:
Duplicate claim.
Preventing Returned or Denied Claims:
Please check all remittance advices for previously submitted claims before resubmitting.
When making changes to previously paid claims, submit an adjustment form rather than a new claim. (See Remittance Advices and Adjustments in this manual.)
Please allow 45 days for the Medicare/Medicaid Part B crossover claim to appear on the remittance advice before submitting the claim directly to Medicaid.
Reasons for Return or Denial:
Procedure requires Passport provider referral – No Passport provider number on claim.
Preventing Returned or Denied Claims:
A Passport provider number must be on the claim when such a referral is required. See the Passport to Health manual.
Reasons for Return or Denial:
TPL on file and no credit amount on claim.
Preventing Returned or Denied Claims:
If the member has other insurance (or Medicare), bill the other carrier before Medicaid. See Coordination of Benefits in this manual.
If the member’s TPL coverage has changed, providers must notify Conduent TPL unit before submitting a claim.
End of Billing Procedures Chapter
Submitting a Claim
The services described in this manual are billed either electronically on a professional claim or on a CMS-1500 paper claim form. Claims submitted with all of the necessary information are referred to as clean and are usually paid in a timely manner. ( See the Billing Procedures chapter in this manual.)
Claims are completed differently for the different types of coverage a member has. The following are accepted codes for completing box 24h:
| Code | Member/Servide | Purpose |
|---|---|---|
| 1 | EPSDT | Used when the member is under age 21. |
| 2 | Family Planning | Used when providing family planning services. |
| 3 | EPSDT and family planning | Used when the member is under age 21 and is receiving family planning services. |
| 4 | Pregnancy (any service provided to a pregnant woman) | Used when providing services to to pregnant women. |
| 6 | Nursing facility member | Used when providing services to nursing facility residents. |
Unless otherwise stated, all paper claims must be mailed to the following address:
Claims Processing
P.O. Box 8000
Helena, MT 59604
CMS-1500 Agreement
Your signature on the CMS-1500 constitutes your agreement to the terms presented on the back of the form. This form is subject to change by the Centers for Medicare and Medicaid Services (CMS).
Avoiding Claim Errors
Claims are often denied or even returned to the provider before they can be processed. To avoid denials and returns, double-check each claim to confirm the following items are accurate. For more information on returned and denied claims, see the Billing Procedures chapter in this manual.
Common Claim Errors
Claim Errors:
Required field is blank.
Prevention:
If a required field is blank, the claim may either be returned or denied.
Claim Errors:
Member ID number missing or invalid.
Prevention:
This is a required field; verify that the member’s Medicaid ID number is listed as it appears on the member’s eligibility information.
Claim Errors:
Patient name missing.
Prevention:
This is a required field; check that it is correct.
Claim Errors:
Provider NPI and taxonomy missing or invalid.
Prevention:
Verify the correct NPI and taxonomy are on the claim.
Claim Errors:
Referring or Passport provider name and ID number missing.
Prevention:
When a provider refers a member to another provider, include the referring provider’s name and ID number or Passport number. See the Passport to Health manual.
Claim Errors:
Prior authorization number missing.
Prevention:
When prior authorization is required for a service, the prior authorization number must be listed on the claim. See the Prior Authorization chapter in this manual.
Claim Errors:
Not enough information regarding other coverage.
Prevention:
When a member has other coverage, related fields become required.
Claim Errors:
Authorized signature missing.
Prevention:
Each claim must have an authorized signature belonging to the provider, billing clerk, or office personnel. The signature may be typed, stamped, or hand-written.
Claim Errors:
Signature date missing.
Prevention:
Each claim must have a signature date.
Claim Errors:
Incorrect claim form used.
Prevention:
Services covered in this manual require a CMS-1500 claim form or an electronic professional claim.
Claim Errors:
Information on claim form not legible.
Prevention:
Information on the claim form must be legible. Use dark ink and center the information in the field. Information must not be obscured by lines.
Claim Errors:
Medicare EOMB not attached.
Prevention:
When Medicare is involved in payment on a claim, the Medicare EOMB must be attached to the claim or it will be denied.
Other Programs
This chapter also applies to claims forms completed for Mental Health Services Plan (MHSP) services and Healthy Montana Kids (HMK)/CHIP eyeglass services.
End of Submitting a Claim Chapter
How Payment Is Calculated
Overview
Though providers do not need the information in this chapter in order to submit claims to the Department, the information allows providers to understand how payment is calculated and to predict approximate payment for particular claims.
The RBRVS Fee Schedule
Most services by provider types covered in this manual are reimbursed for using he Department’s RBRVS fee schedule. RBRVS stands for Resource-Based Relative Value Scale. The fee schedule includes CPT codes and HCPCS codes. Within the CPT coding structure, only anesthesia services and clinical lab services are not reimbursed for using the RBRVS fee schedule.
NOTE: Many Medicaid payment methods are based on Medicare, but there are differences. In these cases, the Medicaid method prevails.
RBRVS was developed for the Medicare program. Medicare does a major update annually, with smaller updates performed quarterly. Montana Medicaid’s RBRVS-based fee schedule is based largely on the Medicare model, with a few differences as described below. By adapting the Medicare model to the needs of the Montana Medicaid program, the Department was able to take advantage of the research performed by the federal government and national associations of physicians and other healthcare professionals. RBRVS-based payment methods are widely used across the U.S. by Medicaid programs, workers’ compensation plans and commercial insurers.
Fee Calculation
Each fee is the product of a relative value times a conversion factor.
Basis of Relative Values
For almost all services, Medicaid uses the same relative values as Medicare in Montana. Nationally, Medicare adjusts the relative values for differences in practice costs between localities, but Montana is considered a single locality. For fewer than 1% of codes, relative values are not available from Medicare. For these codes, the Department has set the fee.
When Medicaid payment differs from the fee schedule, consider the following:
- The Department pays the lower of the established Medicaid fee or the provider’s charge
- Modifiers. (See Other Modifiers in this chapter.)
- Provider type (See Professional Differentials in this chapter.)
- Place of service (See Site of Service Differential in this chapter.)
- Date of service (Fees for services may change over time.)
- Also check for cost sharing and Medicare or TPL payments shown on the remittance advice.
Composition of Relative Values
For each code, the relative value is the sum of a relative value for the work effort (including time, stress, and difficulty), the associated transitional practice expense, and the associated malpractice expense.
Site of Service Differential
The Medicare program has calculated two sets of relative values for each code: one reflects the practitioner’s practice cost of performing the service in an office and one reflects the practitioner’s practice cost of performing the service in a facility.
Medicaid typically pays a lower fee if the service is provided in a facility because Medicaid typically also pays the facility.
Conversion Factor
The Department sets the conversion factor for the state fiscal year (July through June) and it is listed on the fee schedule.
Policy Adjuster
To encourage access to maternity services and family planning services, the Department increases fees for these codes using a policy adjuster that increases the fee. The fee listed on the fee schedule includes the policy adjuster.
Global Periods
For many surgical services and maternity services, the fee covers both the service and all related care within a specified global period. For almost all such codes, the global periods used by Medicaid are identical to those used by Medicare, but in cases of differences the Medicaid policy applies. See the Billing Procedures chapter in this manual for information on global periods.
Professional and Technical Components
Many imaging services and some diagnostic services are divided into the technical component (performing the test) and the professional component (interpreting the test). A practitioner who only performs the test would bill the service with modifier TC; a practitioner who only interprets the test would bill Modifier 26; and a practitioner who performs both components would bill the code without a modifier. Performance of both components is called the global service. The fee schedule has separate fees for each component and for the global service.
Other Modifiers
Under the RBRVS fee schedule, certain other modifiers also affect payment. Modifiers affecting reimbursement are listed in the table on the next page.
How Modifiers Change Pricing
- Modifiers may not be applicable for all services.
- For services paid via the RBRVS fee schedule, the fee schedule shows the list of services for which Modifiers 26, TC, 50, 51, 62, 66, and 80 apply.
- If a modifier does not appear in the list below, then it does not affect pricing.
- Use of Modifier 22 is prohibited for mental health services. In 2013, the CPT manual added two codes specifically for crisis with instructions and guidance for providers.
- The list shows summary modifier descriptions. See the CPT and HCPCS coding books for the full text.
Modifiers That Affect Pricing
Modifier: 22 Definition: Increased procedural service
How Payment is Affected: The services is paid at 110% of the fee.
Modifier: 26 Definition: Professional component
How Payment is Affected: For services paid via the RBRVS fee schedule, see the specific service. For other services, payment equals 40% of the fee.
Modifier: 47 Definition: Anesthesia by surgeon
How Payment is Affected: Modifier not allowed.
Modifier: 50 Definition: Bilateral procedure
How Payment is Affected: The procedure is paid at 150% of the fee.
Modifier: 51 Definition: Multiple procedures
How Payment is Affected: Each procedure is paid at 50% of the fee.
Modifier: 52 Definition: Reduced service
How Payment is Affected: The service is paid at 50% of the fee.
Modifier: 53 Definition: Discontinued procedure
How Payment is Affected: The service is paid at 50% of the fee.
Modifier: 54 Definition: Surgical care only
How Payment is Affected: The service is paid at 75% of the fee.
Modifier: 55 Definition: Postoperative management only
How Payment is Affected: The service is paid at 25% of the fee.
Modifier: 56 Definition: Preoperative management only
How Payment is Affected: The service is paid at 25% of the fee.
Modifier: 5 9 Definition: Distinct procedural service
How Payment is Affected: The service is paid at 50% of the fee unless the procedure is identified as ‘modifier 51 exempt’ or ‘add-on’.
Modifier: 62 Definition: Two surgeons
How Payment is Affected: Each surgeon is paid at 62.5% of the fee.
Modifier: 80 Definition: Assistant surgeon
How Payment is Affected: The service is paid at 16% of the fee.
Modifier: 81 Definition: Minimum assistant surgeon
How Payment is Affected: The service is paid at 16% of the fee.
Modifier: 82 Definition: Assistant surgeon; qualified resident surgeon not available
How Payment is Affected: The service is paid at 16% of the fee.
Modifier: 90 Definition: Reference laboratory
How Payment is Affected: Modifier not allowed
Modifier: AD Definition: Medical supervision of more than four concurrent anesthesia procedures
How Payment is Affected: Each service is paid at 52.5% of the fee.
Modifier: AS Definition: Physician assistant, nurse practitioner or clinical nurse specialist as assistant at surgery
How Payment is Affected: The service is paid at 16% of the fee.
Modifier: QK Definition: Medical supervision of 2–4 concurrent anesthesia procedures
How Payment is Affected: Each service is paid at 52.5% of the fee.
Modifier: QX Definition: Certified registered nurse anesthetist service: medically directed by MD
How Payment is Affected: Each service is paid at 52.5% of the fee.
Modifier: QZ Definition: Certified registered nurse anesthetist service without medical direction
How Payment is Affected: The modifier does not reduce the fee, but a professional differential of 90% is applied due to provider type. See Professional Differentials in this chapter.
Modifier: TC Definition: Technical component
How Payment is Affected: For services paid via the RBRVS fee schedule, see the specific service. For other services, payment equals 60% of the fee.
Professional Differentials
Mid-level practitioners generally receive 90% of the fee that a physician would receive for the same service. The exception is that mid-level practitioners receive 100% of the fee for immunizations, family planning, injectables, lab and pathology services, radiology, cardiography and echocardiography, and services to members under age 21 (i.e., well-child EPSDT services).
Charge Cap
For the services covered in this manual, Medicaid pays the lower of the established Medicaid fee or the provider’s charge.
Bundled Codes
A few services are covered by Medicaid but have a fee of zero, meaning that payment for the service is considered bundled into the payment for services that are usually provided with it. Because these services are covered by Medicaid, providers may not bill members for them on a private-pay basis.
Status Codes
The Medicare physician fee schedule includes status codes that show how each services is reimbursed. Medicaid also uses status codes.
Anesthesia Services
With the exception of moderate conscious sedation, Montana Medicaid does not allow separate reporting of anesthesia for a medical or surgical procedure when it is provided by the practitioner performing the procedure.
When billing for anesthesia services, the date of service on the claim form must match the date of service that anesthesia was administered. If the surgery overlaps days, then bill the anesthesia only with the start date.
NOTE: When billing Medicaid for anesthesia services, enter the number of minutes in the Units field of the CMS-1500 claim form.
CPT states: For continuous services that last beyond midnight, use the date in which the service began and report the total units of time provided continuously.
The following payment method is used for anesthesia services, regardless of whether the service is billed by an anesthesiologist or another professional. Though the method differs from the RBRVS payment method, the two methods are linked and contain similar provisions.
Time Units
A unit of time for anesthesia is 15 minutes, though Medicaid does pay for partial units. Providers enter the number of minutes on the claim; the claims processing contractor then converts the minutes to time units.
Base Units
Base units are adopted by Medicaid from the schedule of base units used by Medicare. Base units are calculated by the American Society of Anesthesiologists. Providers do not enter the number of base units on the claim.
Fee Calculation
For a particular service, Medicaid payment is calculated as follows: (Time units + base units) x anesthesia conversion factor = payment
Modifiers
Payment for anesthesia services is affected by the modifier pricing rules shown in this chapter; take note of the modifiers for anesthesia care provided under medical supervision. Medicaid follows Medicare in not paying extra for the patient status Modifiers P1 to P6.
Clinical Lab Services (ARM 37.85.212)
In general, Medicaid pays the same fees for clinical lab services as Medicare pays in Montana. If a Medicare fee is not available for a lab test covered by Medicaid, then payment is calculated by looking at the average charge and the amounts paid by other payers.
Vaccines and Drugs Provided within the Office
Many vaccines are available for free to physician offices through the Vaccines for Children (VFC) program. For information on obtaining these vaccines, call (406) 444-5580. For these vaccines, Medicaid does not pay separately. Medicaid does pay for the administration of the vaccine, however. Medicaid pays for most vaccines not available through the VFC program. (See the Immunizations section of the Billing Procedures chapter in this manual.)
Reimbursement for physician administered drugs (PAD), which are billed using HCPCS codes is made according to the Department’s fee schedule. The Department’s fee schedule is based on the Medicare Average Sale Price (ASP) Fee Schedule if there is an ASP fee, or the RBRVS fee if there is an RBRVS fee. If there is no ASP or RBRVS fee then the fee is calculated by National Drug Code (NDC) using the estimated acquisition cost to set reimbursement. Most must be billed with a HCPCS code and include the NDC, unit type, and number of units.
How Cost Sharing Is Calculated on Medicaid Claims
Member cost sharing fees are a set dollar amount per visit. ( See the Cost Sharing section in Billing Procedures chapter in the General Information for Providers Manual) The member’s cost sharing amount is shown on the remittance advice and deducted from the Medicaid allowed amount.
NOTE: When billing Medicaid for anesthesia services, enter the number of minutes in the Units field of the CMS-1500 claim form.
How Payment Is Calculated on TPL Claims
When a member has coverage from both Medicaid and Medicare, Medicare is the primary payer as described in the Coordination of Benefits chapter of this manual. Medicaid then makes a payment as the secondary payer. For the provider types covered in this manual, Medicaid’s payment is calculated so that the total payment to the provider is either the Medicaid allowed amount less the Medicare paid amount or the sum of the Medicare coinsurance and deductible, whichever is lower. This method is sometimes called “lower of” pricing.
Other Department Programs
The payment method described in this chapter also applies to services provided under the Mental Health Services Plan (MHSP).
End of How Payment Is Calculated Chapter
Appendix A: Forms
- Individual Adjustment Request
- Physician Certification for Abortion Services (MA-37)
- Informed Consent to Sterilization (MA-38)
- Medicaid Hysterectomy Acknowledgement (MA-39)
- Paperwork Attachment Cover Sheet
End of Appendix A: Forms Chapter
Appendix B: Place of Service Codes
End of Appendix B: Place of Service Codes Chapter
Definitions and Acronyms
HCPCS/CPT Codes
Montana Medicaid adds many codes from the yearly edition of the Current Procedural Terminology and HCPCS manuals. Refer to the fee schedules posted on the Provider Information website. If you are billing unlisted J codes (e.g., J3490), verify that a new J code does not exist before you bill. If one does not exist send the claim with a copy of the invoice directly to the State office.
Nondiscrimination (ARM 37.85.402)
The Department does not exclude, deny benefits to, or otherwise discriminate against any person on the basis of race, color, national origin, age, sex, handicap, political beliefs, religion or disability. This includes the admission to, participation in, or receipt of services or benefits of any of its programs, activities or employment, whether carried out by the Department or through a contractor or other entity.
For questions or to file a complaint alleging violations, contact the Montana Human Rights Bureau (800) 542-0807 or (406) 444-2884.
To file a complaint with the Office of Civil Rights, visit: http://www.hhs.gov/ocr/civilrights/complaints/index.html.
Sports Physicals
A sports physical is typically a non problem-oriented encounter in which the provider evaluate and certifies a patient’s involvement in organized sports, such as high school football. If a comprehensive history and physical examination are performed, report the age-appropriate code from the preventive medicine series. If less than a comprehensive history and exam, are performed, report the appropriate level office or other outpatient evaluation and management visit code.
Tamper-Resistant Prescription Pads
Federal law requires written Medicaid prescriptions to be on tamper-resistant pads. The Department, in accordance with CMS guidance, requires that a Medicaid prescription pad contain all of the following.
- One or more industry-recognized features designed to prevent unauthorized copying of a completed or blank prescription form,
- One or more industry-recognized features designed to prevent the erasure or modification of information written on the prescription by the prescriber; and
- One or more industry-recognized features designed to prevent the use of counterfeit prescription forms.
End of Definitions and Acronyms Chapter
Index
Previous editions of this manual contained an index.
This edition has three search options.
- Search the whole manual. Open the Complete Manual pane. From your keyboard press the Ctrl and F keys at the same time. A search box will appear. Type in a descriptive or key word (for example "Denials". The search box will show all locations where denials discussed in the manual.
- Search by Chapter. Open any Chapter tab (for example the "Billing Procedures" tab). From your keyboard press the Ctrl and F keys at the same time. A search box will appear. Type in a descriptive or key word (for example "Denials". The search box will show where denials discussed in just that chapter.
- Site Search. Search the manual as well as other documents related to a particular search term on the Montana Healthcare Programs Site Specific Search page.
End of Index Chapter
End of Physician-Related Services Manual
Update Log
Publication History
This publication supersedes all previous Physician-Related Services handbooks. Published by the Montana Department of Public Health & Human Services, January 2005.
Updated September 2002, January 2003, June 2003, July 2003, August 2003, September 2003, December 2003, June 2004, September 2004, November 2004, January 2005, March 2005, January 2006, April 2006, July 2006, July 2008, July 2014, July 2015, August 2015, September 2016, November 2016, September 2017, and March 2021.
CPT codes, descriptions and other data only are copyright 2014 American Medical Association (or such other date of publication of CPT). All Rights reserved. Applicable FARS/DFARS Apply.
Update Log
03/05/2021
Updated the discrimination contact information in the Definitions and Acronyms chapter.
09/29/2017
Physician-Related Services Manual converted to an HTML format and adapted to 508 Accessibility Standards. Language throughout the manual was updated.
11/28/2016
In summary, the Page 5.6 of the Billing Procedures chapter was amended to add information for locum tenens, several links were updated, and two blank pages were removed. The Table of Contents and Index sections were adjusted, several links were updated in the Introduction and Covered Services Chapter, the entire manual was formatted as approved by the September 2016 Manuals Meeting for initial 508 adaptations, and the Cover page was amended with the current date.
09/12/2016
In summary, the entire manual has undergone formatting changes, the Billing Procedures section has had some minor language changes and the Cover reflects the current date.
08/31/2016
In summary, The cost share section was removed from the Billing Procedures Chapter, related entries were removed from the Index Section adjustments were made to the Index Section , and the date was changed on the Cover Page.
07/31/2015
Physician-Related Services, August 2015: Entire Manual, Removed EPSDT Well-Child
07/08/2014
Physician-Related Services, July 2014: Multiple Chapters
07/14/2008
Physician-Related Services, March 2008: Key Contacts, Completing a Claim Form, Prior Authorization, Billing for Immunizations
07/25/2006
Physician-Related Services, July 2006: Well-Child EPSDT Update
04/25/2006
Physician-Related Services, April 2006: Revised Instructions for Completing a Claim, Revised Information on How Cost-Sharing Affects Claim Payment
01/05/2006
Physician-Related Services, September 2005: New EPSDT, Hysterectomy Acknowledgement Form, Revised Information on Imaging Modifiers, Billing for Immunizations, and ER Visits for Clients Under Age 2
03/01/2005
Physician-Related Services, March 2005: Hysterectomy Acknowledgement Update
01/25/2005
Physician-Related Services, January 2005: Rule References Added, Updates to Covered Services, PA and Modifiers
11/16/2004
Physician-Related Services, November 2004: Updated Prescription Drug PA Criteria
09/15/2004
Physician-Related Services, September 2004: Team Care Added
06/16/2004
Physician-Related Services, July 2004: Clarification on Sterilizations, Hysterectomies, Abortions and HIPAA and Drug PA Update
12/23/2003
Physician-Related Services, December 2003: Immunizations, PA Criteria, Family Planning, and Using Modifiers
09/16/2003
Physician-Related Services, September 2003: Hysterectomies and Prescription Drug PA Update
08/20/2003
Physician-Related Services, June 2003: New Emergency Services Policy and Hard Card Information
07/28/2003
Physician-Related Services, Hysterectomy Requirements
06/01/2003
Physician-Related Services, New PA Requirements and Hysterectomy Information
01/02/2003
Physician-Related Services, January 2003: Prior Authorization
09/01/2002
Physician-Related Services, September 2002: Cost Sharing
End of Update Log Chapter
Table of Contents
Key Contacts and Websites
Introduction
Manual Organization
Manual Maintenance
Rule References
Claim Review (MCA 53-6-111, ARM 37.85.406)
Getting Questions Answered
Covered Services
General Coverage Principles
- Services within Scope of Practice (ARM 37.85.401)
- Services Provided by Physicians (ARM 37.86.101 - 105)
- Services Provided by Mid-Level Practitioners (ARM 37.86.201 - 205)
- Services Provided by Podiatrists (ARM 37.86.501 - 506)
- Services Provided by Independent Labs (ARM 37.86.3201 - 3205)
- Services Provided by Independent Imaging Facilities (ARM 37.86.3201 - 3205)
- Services Provided by Independent Diagnostic Testing Facilities (ARM 37.85.220)
- Services Provided by Public Health Clinics (ARM 37.86.1401 - 1406)
- Non-Covered Services (ARM 37.85.201 and ARM 37.86.205)
- Importance of Fee Schedules
Coverage of Specific Services
- Abortions (ARM 37.86.104)
- Cosmetic Services (ARM 37.86.107)
- Early and Periodic Screening, Diagnostic, and Treatment Services Program
- Family Planning Services (ARM 37.86.1701)
- Home Obstetrics (ARM 37.85.207)
- Immunizations
- Infertility (ARM 37.85.207)
- Prescriptions (ARM 37.86.1102)
- Routine Podiatric Care
- Sterilization (ARM 37.86.104)
- Surgical Services
- Telemedicine Services
- Transplants
- Weight Reduction
Prior Authorization
Prior Authorization for Retroactively Eligible Members
Coordination of Benefits
When Members Have Other Coverage
Identifying Other Sources of Coverage
When a Member Has Medicare
- Medicare Part A Claims
- Medicare Part B Crossover Claims
- When Medicare Pays or Denies a Service
- When Medicaid Does Not Respond to Crossover Claims
Submitting Medicare Claims to Medicaid
When a Member Has TPL (ARM 37.85.407)
- Exceptions to Billing Third Party First
- Requesting an Exemption
- When the Third Party Pays or Denies a Service
- When the Third Party Does Not Respond
Other Programs
Billing Procedures
Claim Forms
Timely Filing Limits (ARM 37.85.406)
- Tips to Avoid Timely Filing Denials
When to Bill Medicaid Members (ARM 37.85.406)
Member Cost Sharing (ARM 37.85.204 and ARM 37.85.402)
When Members Have Other Insurance
Billing for Retroactively Eligible Members
Place of Service
Multiple Visits (E/M Codes) on Same Date
Coding
Using the Medicaid Fee Schedule
Using Modifiers
Billing Tips for Specific Provider Types
- Mid-Level Practitioner Billing
- Physician Billing
- Podiatrist Billing
- Independent Diagnostic Testing Facilities
- Independent Labs
- Imaging
RHC/FQHC - Professional Services in Hospitals
Billing Tips for Specific Services
- Abortions
- Anesthesia
- Bundled Services
- Cosmetic Services
- EPSDT Well-Child Screens
- Family Planning Services
- Immunizations
- Obstetrical Services
- Reference Lab Billing
- Sterilization
- Surgical Services
- Assistant at Surgery
- Telemedicine Services
- Transplants
- Weight Reduction
- Unlisted Procedures
Submitting Electronic Claims
- Electronic Claims
Billing Electronically with Paper Attachments
Submitting Paper Claims
Claim Inquiries
The Most Common Billing Errors and How to Avoid Them
Submitting a Claim
CMS-1500 Agreement
Avoiding Claim Errors
How Payment is Calculated
Overview
The RBRVS Fee Schedule
- Fee Calculation
- Basis of Relative Values
- Composition of Relative Values
- Site of Service Differential
- Conversion Factor
- Policy Adjuster
- Global Periods
- Professional and Technical Components
- Other Modifiers
- How Modifiers Change Pricing
- Professional Differentials
- Charge Cap
- Bundled Codes
- Status Codes
Anesthesia Services
- Time Units
- Base Units
- Fee Calculation
- Modifiers
Clinical Lab Services (ARM 37.85.212)
Vaccines and Drugs Provided within the Office
How Cost Sharing Is Calculated on Medicaid Claims
How Payment Is Calculated on TPL Claims
How Payment Is Calculated on Medicare Crossover Claims
Other Department Programs
Appendix A: Forms
Appendix B: Place of Service Codes
Definitions and Acronyms
Index
End of Table of Contents Chapter
Key Contacts and Websites
End of Key Contacts and Websites Chapter
Introduction
Thank you for your willingness to serve members of the Montana Medicaid program and other medical assistance programs administered by the Department of Public Health and Human Services.
Manual Organization
This manual provides information specifically for physicians, mid-level practitioners, podiatrists, public health clinics, family planning clinics, independent laboratories independent imaging facilities, and independent diagnostic testing facilities.
Most chapters have a section titled Other Programs that includes information about other Department programs such as the Mental Health Services Plan (MHSP) and Healthy Montana Kids (HMK)/CHIP. Other essential information for providers is contained in the separate General Information for Providers manual. Each provider is asked to review both manuals.
A table of contents and an index allow you to quickly find answers to most questions There is a list of contacts on the Contact Us page on the Provider Information website. Find the Contact Us and other resources under the Site Index in the left menu.
Manual Maintenance
Manuals must be kept current.
Notification of manual updates are provided through the weekly web postings under “Recent Website Posts” on the home page of the provider website and under Provider Notices on the provider type page of the provider website. Older versions of the manual may be found through the Archive page on the Provider website. Printing the manual material found at this website for long-term use is not advisable. Department Policy material is updated periodically and it is the responsibility of the users to check and make sure that the policy they are researching or applying has the correct effective date for their circumstances.
Rule References
Providers, office managers, billers, and other medical staff must be familiar with current rules and regulations governing the Montana Medicaid program. Provider manuals are to assist providers in billing Medicaid; they do not contain all Medicaid rules and regulations. Rule citations in the text are a reference tool; they are not a summary of the entire rule. In the event that a manual conflicts with a rule, the rule prevails. Links to rules are available on the Provider Information website. Paper copies of rules are available through the Secretary of State’s office.
NOTE: Providers are responsible for knowing and following current laws and regulations
In addition to the general Medicaid rules outlined in the General Information for Providers manual, the following rules and regulations are also applicable to the physician related services programs:
- Code of Federal Regulations (CFR)
- 42 CFR 410 Supplementary Medical Insurance (SMI) Benefits
- 42 CFR 440 Services: General Provisions
- 42 CFR 441 Services: Requirements and Limits Applicable to Specific Services
- Montana Code Annotated (MCA)
- MCA Title 37-2-101 – 37-2-313 General Provisions Relating to Healthcare Practitioners
- MCA 37-3-101 – MCA 37-3-405 Medicine
- MCA 37-6-101 – MCA 37-6-312 Podiatry
- MCA 37-14-101 – MCA 37-14-102 Radiologic Technologists
- MCA 37-34-101 – MCA 37-34-307 Clinical Lab Science Practitioners
- Administrative Rules of Montana (ARM)
- ARM 37.85.220 Independent Diagnostic Testing Facilities
- ARM 37.86.101 – ARM 37.86.105 Physician Services
- ARM 37.86.201 – ARM 37.86.205 Mid-Level Practitioner Services
- ARM 37.86.501 – ARM 37.86.506 Podiatry Services
- ARM 37.86.3201 – ARM 37.86.3205 Non-Hospital Laboratory and Radiology (X-Ray) Services
- ARM 37.86.1401 – ARM 38.86.1406 Clinic Services
Claims Review (MCA 53-6-111, ARM 37.85.406)
The Department is committed to paying Medicaid providers’ claims as quickly as possible. Medicaid claims are electronically processed and usually are not reviewed by medical experts prior to payment to determine if the services provided were appropriately billed. Although the computerized system can detect and deny some erroneous claims, there are many erroneous claims it cannot detect. For this reason, payment of a claim does not mean the service was correctly billed or the payment made to the provider was correct. Periodic retrospective reviews are performed that may lead to the discovery of incorrect billing or incorrect payment. If a claim is paid, and the Department later discovers the service was incorrectly billed or paid or the claim was erroneous in some other way, the Department is required by Federal regulation to recover any overpayment, regardless of whether the incorrect payment was the result of Department or provider error or other cause (42 CFR 456.3).
Getting Questions Answered
The provider manuals are designed to answer most questions; however, questions may arise that require a call to a specific group (such as a program officer, provider relations, or a prior authorization unit). Medicaid manuals, provider notices, fee schedules, forms, and more are available on the Provider Information website.
End of Introduction Chapter
Covered Services
Montana Medicaid covers almost all services provided by physicians, mid-level practitioners, and podiatrists, including preventive care.
This chapter provides covered services information that applies specifically to services performed by physicians, mid-level practitioners, podiatrists, mid-level practitioners within public health clinics, family planning clinics, independent labs, independent imaging facilities, and independent diagnostic testing facilities. Like all healthcare services received by Medicaid members, services provided by these practitioners must also meet the general requirements listed in the Provider Requirements chapter of the General Information for Providers manual.
Services within Scope of Practice (ARM 37.85.401)
Services are covered only when they are within the scope of the provider’s license. As a condition of participation in the Montana Medicaid program, all providers must comply with all applicable state and federal statutes, rules, and regulations.
Services Provided by Physicians (ARM 37.86.101–105)
Physician services are those services provided by individuals licensed under the State Medical Practice Act to practice medicine or osteopathy, which as defined by state law, are within the scope of their practice.
Services Provided by Mid-Level Practitioners (ARM 37.86.201–205)
Mid-level practitioners include physician assistants licensed to practice medicine by the Montana Board of Medical Examiners and advanced practice registered nurses licensed to practice medicine by the Montana Board of Nursing. Advanced practice registered nurses include nurse anesthetists, nurse practitioners, clinical nurse specialists, and certified nurse midwives. Mid-level practitioners also include practitioners outside Montana who hold appropriate licenses in their own states. A mid-level practitioner must bill under his/her own NPI and taxonomy code, rather than under a physician’s. See the Billing Procedures chapter in this manual.
Services Provided by Podiatrists (ARM 37.86.501–506)
Podiatry services are those services provided by individuals licensed under state law to practice podiatry. Refer to Routine Podiatric Care in this chapter and the podiatrist fee schedule. Locate the Podiatrist Page and fee schedule on the Provider Website by visiting the Resources by Provider Type page.
Services Provided by Independent Labs (ARM 37.86.3201–3205)
Medicaid covers tests provided by independent (non-hospital) clinical laboratories when the following requirements are met:
- Services are ordered and provided by physicians, dentists, or other providers licensed within the scope of their practice as defined by law. Medicaid does not cover lab services ordered by chiropractors.
- Services are provided in an office or other similar facility, but not in a hospital outpatient department or clinic.
- Providers of lab services must be Medicare-certified.
- Providers of lab services must have a current Clinical Laboratory Improvement Amendments (CLIA) certification number. CLIA certification may be obtained in Montana through the Department. See the Contact Us link in the site index in the Provider Information website left menu.
- Medicaid does not cover reference lab services. Providers may bill Medicaid only for those lab services they have performed themselves. Modifier 90, used to indicate reference lab services, is not covered by Medicaid.
Services Provided by Independent Imaging Facilities (ARM 37.86.3201–3205)
Medicaid covers tests provided by independent (non-hospital) imaging facilities when the following requirements are met:
- Services are ordered and provided by physicians, dentists, or other providers licensed within the scope of their practices as defined by law.
- Services are provided in an office or similar facility, but not in a hospital outpatient department or clinic.
- Imaging providers must be supervised by a physician licensed to practice medicine within the state the services are provided.
- Imaging providers must meet state facility licensing requirements. Facilities must also meet any additional federal or state requirements that apply to specific tests (e.g., mammography). All facilities providing screening and diagnostic mammography services are required to have a certificate issued by the Federal Food and Drug Administration (FDA). For more information contact the FDA at 1-800-838-7715.
- For most imaging services and some other tests, the fee schedules show different fees depending on whether the practitioner provided only the technical component (performing the test), only the professional component (interpreting the test), or both components (also known as the global service). Practitioners must bill only for services they provided.
- Technical components of imaging services must be performed by appropriately licensed staff (e.g., x-ray technician) operating within the scope of their practice as defined by state law and under the supervision of a physician.
Services Provided by Independent Diagnostic Testing Facilities (ARM 37.85.220)
- Medicaid covers diagnostic testing services provided by independent diagnostic testing facilities (IDTF) under the supervision of a physician. (See the IDTF fee schedule.)
- Services may be performed in either a fixed location or mobile facility, but must be independent of a hospital.
- Before enrolling in Medicaid, IDTFs must be enrolled in Medicare.
Services Provided by Public Health Clinics (ARM 37.86.1401–1406)
- Public health clinic services are physician and mid-level practitioner services provided in a clinic designated by the Department as a public health clinic.
- Services must be provided directly by a physician or by a public health nurse under a physician’s immediate supervision (i.e., the physician has seen the patient and ordered the service).
- Minimal services are covered when provided by a registered nurse operating under protocols. These services do not require that the physician see the patient.
Services Provided by Mobile Imaging/Portable X-ray Supplier (ARM 37.85.219 )
Medicaid covers tests provided by a mobile imaging provider when the following requirements are met:
- Services are ordered by physicians or other providers licensed within the scope of their practices as defined by law.
- Services are provided at a patient’s locations such as home or nursing home.
- Providers must be enrolled in the federal Medicare program as a mobile imaging/portable X-ray supplier and certified by the DPHHS Quality Assurance Division.
- Providers must be enrolled with Montana Healthcare Programs.
- Mobile imaging providers must be supervised by a physician licensed to practice medicine within the state the services are provided.
- Services are provided by qualified X-ray technologists.
Services Provided by Licensed Direct Entry Midwife (ARM 37.86.1201 )
Medicaid covers services provided by a licensed direct entry midwife when the following requirements are met:
- Must be licensed by Montana Department of Labor and Industry.
- Services include prenatal and delivery or postpartum care only.
- Services must be performed in birthing center.
Non-Covered Services (ARM 37.85.207 and ARM 37.86.205)
Some services not covered by Medicaid include the following:
- Acupuncture
- Naturopath services
- Surgery for weight loss (gastric bypass, banding and other bariatric surgery)
- Services provided by surgical technicians who are not physicians or mid-level practitioners
- Services considered experimental or investigational
- Services provided to Medicaid members who are absent from the state, with the following exceptions:
- Medical emergency
- Required medical services are not available in Montana. Prior authorization may be required. See the Prior Authorization chapter in this manual and the Prior Authorization Information page found under the index in the left menu on the Provider Information website.
- The Department has determined that the general practice for members in a particular area of Montana is to use providers in another state.
- Out-of-state medical services and all related expenses are less costly than in-state services. Check the physician’s fee schedule to determine if the code is covered.
- Montana makes adoption assistance or foster care maintenance payments for a member who is a child residing in another state.
- Medicaid does not cover services that are not direct patient care such as the following:
- Missed or canceled appointments
- Mileage and travel expenses for providers
- Preparation of medical or insurance reports
- Service charges or delinquent payment fees
- Telephone services in home
- Remodeling of home
- Plumbing service
- Car repair and/or modification of automobile
Importance of Fee Schedules
The easiest way to verify coverage for a specific service is to check the Department’s fee schedule for your provider type. Fee schedules list Medicaid covered codes and provide clarification of indicators such as whether a code requires prior authorization, can be applied to a co-surgery, or can be billed bilaterally, etc. In addition to being listed on the fee schedule, all services provided must also meet the coverage criteria listed in the Provider Requirements chapter of the General Information for Providers manual and in this chapter. Use the fee schedule in conjunction with the more detailed coding descriptions listed in the CPT, HCPCS, and ICD coding books. Take care to use the fee schedule and coding books that pertain to the date of service.
NOTE: Use the current fee schedule for your provider type to verify coverage for specific services.
Fee schedules are available on the Provider Information website listed under each provider type page.
Locate Provider type pages on the Provider Website under "Resources by Provider Type".
Locate Physician Fee Schedules and ATP Tests and Fees Fee Schedules on the Physician Provider Type page.
Coverage of Specific Services
The following are coverage rules for specific services provided by physicians, mid-level practitioners, and podiatrists.
Abortions (ARM 37.86.104)
Abortions are covered when one of the following conditions is met:
- The member’s life would be endangered if the fetus is carried to term.
- The pregnancy is the result of rape or incest.
- The abortion is determined by the attending physician to be medically necessary, even if the member’s life is not endangered if the fetus is carried to term.
A completed Medicaid Healthcare Programs Physician Certification for Abortion Services (MA-37) form must be submitted with every abortion claim or payment will be denied. This form is the only form Medicaid accepts for abortion services. Complete only one section of this form.
When using mifepristone (Mifeprex or RU 486) to terminate a pregnancy, it must be administered within 49 days from the beginning of the last menstrual period by or under the supervision of a physician who:
- Can assess the duration of a pregnancy.
- Can diagnose ectopic pregnancies.
- Can provide surgical intervention in cases of incomplete abortion or severe bleeding, or can provide such care through other qualified physicians.
- Can assure access to medical facilities equipped to provide blood transfusion and resuscitation.
- Has read, understood, and explained to the member the prescribing information for mifepristone.
Cosmetic Services (ARM 37.86.104)
Medicaid covers cosmetic services only when the condition has a severe detrimental effect on the member’s physical and psychosocial well-being. Mastectomy and reduction mammoplasty services are covered only when medically necessary. Medical necessity for reduction mammoplasty is related to signs and symptoms resulting from macromastia. Medicaid covers surgical reconstruction following breast cancer treatment. Before cosmetic services are performed, they must be prior authorized. Services are authorized on a case-by-case basis. (See the Prior Authorization Information on the Contact Us link located in the site index in the left menu of the Provider Website.
Early and Periodic Screening, Diagnostic, and Treatment (EPSDT) Services (ARM 37.86.2201–2235) Program
The EPSDT program covers all medically necessary services for children ages 20 and under. Providers are encouraged to use a series of screening and diagnostic procedures designed to detect diseases, disabilities, and abnormalities in the early stages. (See the EPSDT Well-Child chapter in the General Information for Providers manual.) Some services are covered for children that are not covered for adults, such as the following:
- Nutritionist services
- Private duty nursing
- Respiratory therapy
- Therapeutic family and group home care
- Substance dependency inpatient and day treatment services
- School-based services
All prior authorization and Passport approval requirements must be followed. See the Prior Authorization chapter in this manual and the Passport to Health manual.
Family Planning Services (ARM 37.86.1701)
Family planning services include the following:
- Annual visit
- Comprehensive history
- Initial physical examination
- Initial visit
- Laboratory services
- Medical counseling
- Routine visits
Medicaid covers prescription contraceptive supplies, implantation, or removal of subcutaneous contraceptives, and fitting or removal of an IUD and fitting of a diaphragm. Approval by the Passport provider is not required for family planning services. See the Submitting a Claim chapter in this manual for Passport indicators. Specific billing procedures must be followed for family planning services. (See Billing Procedures.)
Home Obstetrics (ARM 37.85.207)
Home deliveries are only covered on an emergency basis by a physician or licensed midwife. Home deliveries are those delivery services not provided in a licensed healthcare facility or nationally accredited birthing center and necessary to protect the health and safety of the woman and fetus from the onset of labor through delivery.
Immunizations
The Vaccines for Children (VFC) program makes selected vaccines available at no cost to providers for eligible children 18 years old and under. Medicaid will therefore pay only for the administration of these vaccines (oral, nasal, or injection) and only the federal mandated rate. VFC covered vaccines may quarterly. For more information on the VFC program and current VFC covered vaccines, call the Department’s Immunization program at (406) 444-5580, or refer to the most recent VFC provider notice.
Medicaid does not cover pneumonia and flu vaccines for members with Medicare Part B insurance because Medicare covers these immunizations. Other vaccines for Medicare patients should be billed through Medicare Part D.
Infertility (ARM 37.85.207)
Medicaid does not cover treatment services for infertility, including sterilization reversals.
Prescriptions (ARM 37.86.1102)
For detailed information about prescription drugs, refer to the Prescription Drug Program manual on the Pharmacy page of the website.
The page can be located by choosing the Resources by Provider Type link from the home page of the Provider Website.
The DUR Board has set monthly limits on certain drugs. Use over these amounts requires prior authorization. Refer to the Prior Authorization chapter of the Prescription Drug Program manual for limits.
Routine Podiatric Care
Medicaid pays for routine podiatric care when a medical condition affecting the legs or feet (such as diabetes or arteriosclerosis obliterans) requires treatment by a physician or podiatrist. Routine podiatric care includes the following:
- Cutting or removing of corns and calluses
- Trimming of nails
- Application of skin creams
- Debridement of nails
- Other hygienic or preventive maintenance care
Sterilization (ARM 37.86.104)
Elective Sterilization
Elective sterilizations are sterilizations done for the purpose of becoming sterile. Medicaid covers elective sterilization for men and women when all of the following requirements are met:
- Member must complete and sign the Informed Consent to Sterilization (MA-38 or HHS 687) form at least 30 days, but not more than 180 days, prior to the sterilization procedure. These forms are the only forms Medicaid accepts for elective sterilizations. If one of these forms is not properly completed, payment will be denied. See the Forms page on the Provider Information website for the forms and instructions for completion. Locate the Forms page by choosing the Forms link on the home page of the provider website.
- Member must be at least 21 years of age when signing the form.
- Member must not have been declared mentally incompetent by a federal, state, or local court, unless the member has been declared competent to specifically consent to sterilization.
- Member must not be confined under civil or criminal status in a correctional or rehabilitative facility, including a psychiatric hospital or other correctional facility for the treatment of the mentally ill.
The 30-day waiting period may be waived for either of the following reasons:
- Premature Delivery. The Informed Consent to Sterilization must be completed and signed by the member at least 30 days prior to the estimated delivery date and at least 72 hours prior to the sterilization.
- Emergency Abdominal Surgery. The Informed Consent to Sterilization form must be completed and signed by the member at least 72 hours prior to the sterilization procedure.
All forms required for sterilizations can be downloaded from the Provider Information website, Locate the Forms page by choosing the Forms link on the home page of the provider website.
Before performing a sterilization, the following requirements must be met:
- The member must have the opportunity to have questions regarding the sterilization procedure answered to his/her satisfaction.
- The member must be informed of his/her right to withdraw or withhold consent anytime before the sterilization without being subject to retribution or loss of benefits.
- The member must be made aware of available alternatives of birth control and family planning.
- The member must understand the sterilization procedure being considered is irreversible.
- The member must be made aware of the discomforts and risks which may accompany the sterilization procedure being considered.
- The member must be informed of the benefits and advantages of the sterilization procedure.
- The member must know that he/she must have at least 30 days to reconsider his/her decision to be sterilized.
- An interpreter must be present to translate or sign for those members who are blind, deaf, or do not understand the language to assure the person has been informed.
Informed consent for sterilization may not be obtained under the following circumstances:
- If the member is in labor or childbirth.
- If the member is seeking or obtaining an abortion.
- If the member is under the influence of alcohol or other substance which affects his/her awareness.
Medically Necessary Sterilization
When sterilization results from a procedure performed to address another medical problem, it is considered a medically necessary sterilization. These procedures include hysterectomies, oophorectomies, salpingectomies, and orchiectomies. Every claim submitted to Medicaid for a medically necessary sterilization must be accompanied by one of the following:
- A completed Medicaid Hysterectomy Acknowledgement form (MA-39) for each provider submitting a claim. It is the provider’s responsibility to obtain a copy of the form from the primary or attending physician. Complete only one section of this form. When no prior sterility (Section B) or life-threatening emergency (Section C) exists, the member (or representative, if any) and physician must sign and date Section A of this form prior to the procedure. (See 42 CFR 441.250 for the federal policy on hysterectomies and sterilizations.) Also, for Section A, signatures dated after the surgery date require manual review of medical records by the Department. The Department must verify that the member (and representative, if any) was informed orally and in writing, prior to the surgery, that the procedure would render the member permanently incapable of reproducing. The member does not need to sign this form when Sections B or C are used. Refer to the Forms page on the Provider Information website for instructions on completing the form.
- For members who have become retroactively eligible for Medicaid, the physician must certify in writing that the surgery was performed for medical reasons and must document one of the following:
- The individual was informed prior to the hysterectomy that the operation would render the member permanently incapable of reproducing.
- The reason for the hysterectomy was a life-threatening emergency.
- The member was already sterile at the time of the hysterectomy and the reason for prior sterility.
NOTE: A notation Not a Sterilization on a claim is not sufficient to fulfill these certification requirements.
When submitting claims for retroactively eligible members, attach a copy of the Notice of Retroactive Eligibility (Form 160-M) to the claim if the date of service is more than 12 months earlier than the date the claim is submitted.
Surgical Services
- The fee schedule shows Medicaid policies code by code on global periods, bilateral procedures, assistants at surgery, co-surgeons, and team surgery. These policies are almost always identical to Medicare policies but in cases of discrepancy, the Medicaid policy applies.
- Medicaid only covers assistant at surgery services when provided by physicians or mid-level practitioners who are Medicaid providers.
- Medicaid does not cover surgical technician services.
- See the Billing Procedures chapter regarding the appropriate use of modifiers for surgical services.
Telemedicine Services
Please refer to the Telemedicine section of the General Information for Providers Manual.
Transplants
- All Medicaid transplant services must be prior authorized. See the Prior Authorization Information page. Locate the Prior Authorization page in the Site Index in the left menu of the Provider Website.
- All transplants must be medically necessary.
- Each case receives individualized review and is evaluated for medical suitability.
Weight Reduction
- Physicians and mid-level practitioners who counsel and monitor members on weight reduction programs can be paid for those services. If medical necessity is documented, Medicaid will also cover lab work. Similar services provided by nutritionists are not covered for adults.
- Medicaid does not cover the following weight reduction services:
- Weight reduction plans/programs (e.g., Jenny Craig, Weight Watchers)
- Nutritional supplements
- Dietary supplements
- Health club memberships
- Educational services of nutritionists
End of Covered Services Chapter
Prior Authorization
Prior authorization refers to a list of services that require approval from the Medicaid program prior to the service being rendered. If a service requires prior authorization, the requirement exists for all Medicaid members. When prior authorization is granted, a prior authorization number is issued and must be on the claim.
Different codes are issued for Passport approval and prior authorization; when necessary, both must be on the claim form. Medicaid does not pay for services when prior authorization requirements are not met.
Prior Authorization for Retroactively Eligible Members
When a member is determined retroactively eligible for Medicaid, the member should give the provider a Notice of Retroactive Eligibility (160-M). The provider has 12 months from the date retroactive eligibility was determined to bill for those services. When a member becomes retroactively eligible for Medicaid the provider may:
- Accept the member as a Medicaid member from the current date.
- Accept the member as a Medicaid member from the date retroactive eligibility was effective.
- Require the member to continue as a private-pay member.
Providers may choose whether to accept retroactive eligibility. All prior authorization requirements must be met to receive Medicaid payment. When requesting prior authorization, attach a copy of the 160-M to the prior authorization request. It is the member’s responsibility to ensure his/her caseworker prepares an 160-M for each provider who participates in the member’s healthcare during this retroactive period. See the Billing Procedures chapter in this manual for retroactive eligibility billing requirements. When seeking prior authorization, keep in mind the following:
- The referring provider should initiate all authorization requests.
- Always refer to the current Medicaid fee schedule to verify if prior authorization is required for specific services.
- For a list of services that require prior authorization, who to contact, and documentation requirements, see the Contact Us link in site index in the Provider Information website menu. The Contact Us can be located in the site index in the left menu of the Provider Website.
- Prior authorization criteria forms for most services are available on the Forms page of the Provider Information website.
- When prior authorization is granted from Mountain-Pacific Quality Health (MPQH), providers receive notification from both MPQH and Conduent Claims Processing. The Prior Authorization Notice from Claims Processing has a prior authorization number which must be included on the claim.
End of Prior Authorization Chapter
Coordination of Benefits
Medicaid members often have coverage though Medicare, workers’ compensation, employment-based coverage, individually purchased coverage, etc. Coordination of benefits is the process of determining which source of coverage is the primary payer in a particular situation. In general, providers must bill other carriers before billing Medicaid, but there are some exceptions. (See Exceptions to Billing Third Party First later in this chapter.) Medicare coverage is processed differently than other sources of coverage.
Identifying Other Sources of Coverage
The member’s Medicaid eligibility information may list other payers such as Medicare or other third party payers. (See Member Eligibility and Responsibilities in the General Information for Providers manual.) If a member has Medicare, the Medicare ID number is listed on the eligibility verification. If a member has other coverage (excluding Medicare), it will be shown also. Some examples of third party payers include:
- Private health insurance
- Employment-related health insurance
- Workers’ compensation insurance*
- Health insurance from an absent parent
- Automobile insurance*
- Court judgments and settlements*
- Long-term care insurance
*These third party payers (and others) may not be listed on the member’s Medicaid eligibility information.
Providers must use the same procedures for locating third party sources for Medicaid members as for their non-Medicaid members. Providers cannot refuse service because of a third party payer or potential third party payer.
When a Member Has Medicare
Medicare claims are processed and paid differently than claims involving other payers. The other sources of coverage are referred to as third party liability (TPL), but Medicare is not.
Medicare Part A Claims
Medicare Part A covers inpatient hospital care, skilled nursing care, and other services. Medicare Part A carriers and Medicaid use electronic exchange of institutional claims covering Part A services. Providers must submit these claims first to Medicare. After Medicare processes the claim, an Explanation of Medicare Benefits (EOMB) is sent to the provider. The provider then reviews the EOMB and submits the claim to Medicaid.
Medicare Part B Crossover Claims
Medicare Part B covers outpatient hospital care, physician care and other services. Although outpatient hospital care is covered under Part B, it is processed by Medicare Part A. The Department has an agreement with Medicare Part B carriers for Montana (Noridian) and the Durable Medical Equipment Regional Carrier [DMERC]. Under this agreement, the carriers provide the Department with claims for members who have both Medicare and Medicaid coverage. Providers must tell Medicare that they want their claims sent to Medicaid automatically and must have their Medicare provider number on file with Medicaid.
NOTE: To avoid confusion and paperwork, submit Medicare Part B crossover claims to Medicaid only when necessary.
In these situations, providers need not submit Medicare Part B crossover claims to Medicaid. Medicare will process the claim, submit it to Medicaid, and send the provider an EOMB. Providers must check the EOMB for the statement indicating that the claim has been referred to Medicaid for further processing. It is the provider’s responsibility to follow up on crossover claims and make sure they are correctly billed to Medicaid within the timely filing limit. (See the Billing Procedures chapter.)
When Medicare Pays or Denies a Service
- When Medicare automatic crossover claims are paid or denied, they should automatically cross over to Medicaid for processing, so the provider does not need to submit the claim to Medicaid.
- When Medicare crossover claims are billed on paper and are paid or denied, the provider must submit the claim to Medicaid with the Medicare EOMB (and the explanation of denial codes).
When Medicaid Does Not Respond to Crossover Claims
When Medicaid does not respond within 45 days of the provider receiving the Medicare EOMB, submit a claim and a copy of the Medicare EOMB to Medicaid for processing.
NOTE: When submitting electronic claims with paper attachments, see the Billing Electronically with Paper Attachments section of the Billing Procedures chapter in this manual.
Submitting Medicare Claims to Medicaid
When submitting a claim to Medicaid, include the Medicare EOMB and use Medicaid billing instructions and codes. Medicare’s instructions, codes, and modifiers may not be the same as Medicaid’s. The claim must also include the Medicaid provider number and Medicaid member ID number.
Submit Medicare crossover claims to Medicaid only when:
- The referral to Medicaid statement is missing from the provider’s EOMB.
- The provider does not hear from Medicaid within 45 days of receiving the Medicare EOMB.
- Medicare denies the claim.
When a Member Has TPL (ARM 37.85.407)
When a Medicaid member has additional medical coverage (other than Medicare), the other insurance is often referred to as third party liability (TPL). In most cases,the providers must bill other insurance carriers before billing Medicaid.
Providers are required to notify their members that any funds the member receives from third party payers (when the services were billed to Medicaid) must be turned over to the Department. The following words printed on the member’s statement will fulfill this requirement: When services are covered by Medicaid and another source, any payment the member receives from the other source must be turned over to Medicaid.
Exceptions to Billing Third Party First
In a few cases, providers may bill Medicaid first.
- When a Medicaid member is also covered by Indian Health Service (IHS) or the Montana Crime Victims Compensation Fund, providers must bill Medicaid first. These are not considered third party liability.
- When a member has Medicaid eligibility and Mental Health Services Plan (MHSP) eligibility for the same month, Medicaid must be billed first.
- ICD prenatal and ICD preventive pediatric diagnosis conditions may be billed to Medicaid first. In these cases, Medicaid will pay-and-chase or recover payment from the third party payer.
- The following services may also be billed to Medicaid first:
- Audiology
- Dental (as billed on dental claim)
- Drugs (as billed on drug claims)
- Eyeglasses
- Hearing aids and batteries
- Home and community-based services (waiver)
- Nursing facility (as billed on nursing home claims)
- Optometry
- Oxygen in a nursing facility
- Personal assistance
- Transportation (other than ambulance)
- If the third party has only potential liability, the provider may bill Medicaid first. Do not indicate the potential third party on the claim. Instead, notify the Department of the potential third party by sending the claim and notification directly to the Third Party Liability Unit.
Requesting an Exemption
Providers may request to bill Medicaid first under certain circumstances. In each of these cases, the claim and required information must be sent directly to the Third Party Liability Unit.
- When a provider is unable to obtain a valid assignment of benefits, the provider must submit the claim with documentation that the provider attempted to obtain assignment and certification that the attempt was unsuccessful.
- When the Child Support Enforcement Division has required an absent parent to have insurance on a child, the claim can be submitted to Medicaid when the following requirements are met:
- The third party carrier has been billed, and 30 days or more have passed since the date of service.
- The claim is accompanied by a certification that the claim was billed to the third party carrier, and payment or denial has not been received.
- If another insurance has been billed, and 90 days have passed with no response, attach a note to the claim explaining that the insurance company has been billed or attach a copy of the letter sent to the insurance company. Include the date the claim was submitted to the insurance company and certification that there has been no response.
- When the provider has billed the third party insurance and has received a non-specific denial (e.g., no member name, date of service, amount billed), submit the claim with a copy of the denial and a letter of explanation directly to Medicaid in order to avoid missing the timely filing deadline.
When the Third Party Pays or Denies a Service
When a third party payer is involved (excluding Medicare) and the other payer:
- Pays the claim, indicate the amount paid in the “amount paid” field of the claim when submitting to Medicaid for processing. These claims may be submitted either electronically or on paper.
- Allows the claim, and the allowed amount went toward member's deductible, include the insurance Explanation of Benefits (EOB) when billing Medicaid.
- Denies the claim, include a copy of the denial (including the reason explanation) with the claim, and submit to Medicaid.
- Denies a line on the claim, bill the denied lines together on a separate claim and submit to Medicaid. Include the explanation of benefits (EOB) from the other payer as well as an explanation of the reason for denial (e.g., definition of denial codes).
When the Third Party Does Not Respond
If another insurance has been billed, and 90 days have passed with no response, bill Medicaid as follows:
- Attach a note to the claim explaining that the insurance company has been billed, or attach a copy of the letter sent to the insurance company.
- Include the date the claim was submitted to the insurance company.
- Send this information to the Conduent Third Party Liability Unit.
Other Programs
The information covered in this chapter also applies to members enrolled in the Mental Health Services Plan (MHSP) and Healthy Montana Kids (HMK) dental and vision providers.
End of Coordination of Benefits
Billing Procedures
Claim Forms
Services provided by the healthcare professionals covered in this manual must be billed either electronically on a professional claim 837P or on a CMS-1500 paper claim form. CMS-1500 forms are available from various publishing companies; they are not available from the Department or Provider Relations.
Timely Filing Limits (ARM 37.85.406)
Providers must submit clean claims to Medicaid within:
- Twelve months from the latest of:
- the date of service;
- the date retroactive eligibility is determined; or
- the date disability was determined;
- Six months from the date on the Medicare explanation of benefits approving the service, if the Medicare claim was timely filed and the recipient was Medicare eligible at the time the Medicare claim was filed; or
- Six months from the date on an adjustment notice from a third party payor, where the third party payer has previously processed the claim for the same service and the adjustment notice is dated after the periods described above.
Clean claims are claims that can be processed without additional information or action from the provider. The submission date is defined as the date that the claim was received by the Department or the claims processing contractor. All problems with claims must be resolved within this 12-month period.
Tips to Avoid Timely Filing Denials
- Correct and resubmit denied claims promptly. (See the Remittance Advices and Adjustments chapter in the General Information for Providers manual.)
- If a claim submitted to Medicaid does not appear on the remittance advice within 30 days, contact Provider Relations for claim status.
- If another insurer has been billed and 90 days have passed with no response, you can bill Medicaid. (See the Coordination of Benefits chapter in this manual for more information.)
- To meet timely filing requirements for Medicare/Medicaid crossover claims, see the Coordination of Benefits chapter in this manual.
When to Bill Medicaid Members (ARM 37.85.406)
In most circumstances, providers may not bill Medicaid members for services covered under Medicaid. The main exception is that providers may collect cost sharing from members.
More specifically, providers cannot bill members directly:
- For the difference between charges and the amount Medicaid paid.
- For a covered service provided to a Medicaid-enrolled member who was accepted as a Medicaid member by the provider, even if the claim was denied.
- When the provider bills Medicaid for a covered service, and Medicaid denies the claim because of billing errors.
- When a third party payer does not respond.
- When a member fails to arrive for a scheduled appointment.
- When services are free to the member and free to non-Medicaid covered individuals, such as in a public health clinic.
Under certain circumstances, providers may need a signed agreement to bill a Medicaid member (see the following table).
Providers may bill a member when:
Patient is Medicaid enrolled and provider accepted them as a Medicaid member
- If the service is covered by Medicaid, the provider can bill the member only for cost sharing.
- If the service is not covered by Medicaid, the provider can bill the member only if a custom agreement was signed between the member and the provider before the service was performed.
Patient is Medicaid enrolled and provider did not accept them as a Medicaid member
- The provider can bill the member only if a custom agreement was signed between the member and the provider before the service was performed.
Patient is not Medicaid Enrolled
- The provider may bill the patient.
NOTE: If a provider bills Medicaid and the claim is denied because the member is not eligible, the provider may bill the member directly.
Private-Pay Agreement: This may be a private-pay agreement between the provider and member that states that the member is not accepted as a Medicaid member, and that he/she must pay for the services received.
Custom Agreement: This agreement lists the service the member is receiving and states that the service is not covered by Medicaid and that the member will pay for the service. See the Custom Agreement for Medicaid non-covered service agreement under the Forms button found on the home page of the provider website.
Member Cost Sharing (ARM 37.85.204 and ARM 37.85.402)
When Members Have Other Insurance
If a Medicaid member is also covered by Medicare, has other insurance, or some other third party is responsible for the cost of the member’s healthcare, see the Coordination of Benefits chapter in this manual.
Billing for Retroactively Eligible Members
When the provider accepts the member’s retroactive eligibility, the provider has 12 months from the date retroactive eligibility was determined to bill for those services. When submitting claims for retroactively eligible members in which the date of service is more than 12 months earlier than the date the claim is submitted, attach a copy of the Provider Notice of Eligibility (Form 160-M). The provider must request the form from the member’s local Office of Public Assistance. See https://dphhs.mt.gov/hcsd/OfficeofPublicAssistance.
For more information on retroactive eligibility, see the Member Eligibility and Responsibilities chapter in the General Information for Providers manual.
Place of Service
Place of service must be entered correctly on each line. Medicaid typically reduces payment for services provided in hospitals and ambulatory surgical centers since these facilities typically bill Medicaid separately for facility charges.
Physician clinics that are affiliated with hospitals should be particularly careful. If the Department has granted a clinic provider-based status then the hospital can bill for facility charges even if the clinic is not on the hospital campus. In these situations the clinic must show outpatient (22) as the place of service.
Multiple Visits (E/M Codes) on Same Date
Medicaid generally covers only one visit (or hospital admission) per member per day. When a member requires additional visits on the same day, use a modifier to describe the reason for multiple visits. When a modifier is not appropriate for the situation, attach documentation of medical necessity to the claim, and submit it to the appropriate Department program officer.
Coding
Standard use of medical coding conventions is required when billing Medicaid. Provider Relations or the Department cannot suggest specific codes to be used in billing for services. For coding resources, see the table of Coding Resources section below.
The following suggestions may help reduce coding errors and unnecessary claim denials:
- Use current CPT, HCPCS, and ICD diagnosis coding books.
- Always read the complete description and guidelines in the coding books. Relying on short descriptions can result in inappropriate billing.
- Attend classes on coding offered by certified coding specialists.
- Use specific codes rather than miscellaneous codes.
- Follow CPT guidelines on the difference between a new patient and an established patient.
- Bill for the appropriate level of service provided.
- Services covered within global periods for certain CPT procedures are not paid separately and must not be billed separately. Most surgical and obstetric procedures and some medical procedures include routine care before and after the procedure. Medicaid fee schedules show the global period for each CPT service.
- Use the correct units measurement on claims. In general, Medicaid follows the definitions in the CPT and HCPCS billing manuals. Unless otherwise specified, one unit equals one visit or one procedure. For specific codes, however, one unit may be 15 minutes, a percentage of body surface area, or another quantity. Always check the long text of the code description.
- CPT codes that are billed based on the amount of time spent with the member must be billed with the code that is closest to the time spent. For example, a provider spends 60 minutes with the member. The code choices are 45 to 50 minutes or 76 to 80 minutes. The provider must bill the code for 45 to 50 minutes.
Coding Resources
Please note that the Department does not endorse the products of any particular publisher.
CPT - https://commerce.ama-assn.org/store/
Description:
CPT codes and definitions.
Updated each January.
Contact:
American Medical Association
(800) 621-8335
CPT Assistant - https://commerce.ama-assn.org/store/
Description:
A newsletter on CPT coding issues.
Contacts:
American Medical Association
(800) 621-8335
HCPCS Level II - Available through various publishers and bookstores or from CMS at www.cms.gov.
Description:
HCPCS codes and definitions.
Updated each January and throughout the year.
Contact:
ICD
Description:
ICD diagnosis and procedure code definitions.
Updated each October.
Contact:
Available through various publishers and bookstores.
Miscellaneous - www. shopingenix. com
Description:
Various newsletters and other coding resources.
Contact:
Medicode (Ingenix)
NCCI Policy and Edits Manual - https://www.cms.gov/Medicare/Coding/NationalCorrectCodInitEd/index.html
Description:
This manual contains National Correct Coding Initiative (NCCI) policy and edits, which are pairs of CPT or HCPCS codes that are not separately payable except under certain circumstances. The edits are applied to services billed by the same provider for the same member on the same date of service.
Contact:National Technical Information Service
NOTE: Always refer to the long descriptions in coding books.
Using the Medicaid Fee Schedule
When billing Medicaid, it is important to use the Department’s fee schedule for your provider type in conjunction with the detailed coding descriptions listed in the current CPT and HCPCS diagnosis coding books. In addition to covered services and payment rates, fee schedules often contain helpful information such as appropriate modifiers, global periods, if multiple surgery guidelines apply, if the procedure can be done bilaterally, if an assistant, co-surgeon, or team is allowed for the procedure, if the code is separately billable, and more. Department fee schedules are updated each January and July. Fee schedules are available on the Provider Information website under the Resources by Provider Type button.
Using Modifiers
- Review the guidelines for using modifiers in the CPT, HCPCS, or other helpful resources. Remember to use the modifiers in effect for the date of service of the claim.
- Always read the complete description for each modifier; some modifiers are described in the CPT manual while others are in the HCPCS book.
- The Medicaid claims processing system recognizes three pricing modifiers and one informational modifier per claim line. Providers are asked to place any modifiers that affect pricing in the first three modifier fields.
- When billing with Modifier 50 for bilateral services, put all information on one line with one unit.
- Check the fee schedule to see if Medicaid allows the use of the following modifiers for a particular code: bilateral (50), multiple procedures (51), cosurgery (62), assistant at surgery (80, 81, 82, AS), and team surgery (66).
- Always bill your main surgical procedure code on line 1 of the claim with one unit only. All other subsequent procedures should be billed with the number of units done for each code per line.
- Do not separate out subsequent procedure codes on separate lines. This will cause exact duplicate line denials. Subsequent procedure modifiers should be used when appropriate except when billing add-on codes and Modifier 51 exempt codes.
Billing Tips for Specific Provider Types
Mid-Level Practitioner Billing
Mid-level practitioners must bill under their own NPI and taxonomy number rather than under a physician number.
Physician Billing
Medicaid-enrolled providers may bill for locum tenens physician services when the following criteria are met:
- The regular physician is absent due to illness, pregnancy, vacation or continuing medical education;
- The Medicaid member has arranged or seeks to receive services from the regular physician;
- The regular physician pays the locum tenens for his/her services on a per diem or similar fee-for-time basis;
- The substitute physician does not provide services to Medicaid members over a continuous period of longer than 60 days; and
- Medicaid-enrolled physician may bill locum tenens services using modifier Q6.
Podiatrist Billing
Podiatrists must use appropriate codes and modifiers from their specific fee schedule.
Independent Labs
Independent labs must use appropriate fee schedules, codes, and modifiers for their provider type.
- The provider’s current CLIA certification number must be on file with Provider Relations or all lab claims will be denied. See the Contact Us link on the website for CLIA certification information.
- This requirement also applies to public health labs. Questions regarding public health labs may be directed to the Public Health Lab Assistance hotline. See the Contact Us link on the website.
Independent Diagnostic Testing Facilities (IDTF)
IDTF providers must use appropriate fee schedules, codes and modifiers for their provider type. If an IDTF performs laboratory services, they must enroll as an independent lab in addition to IDTF.
- Repeat modifiers should be used to indicate multiple radiology services of the same radiology code performed on the same day for the same member by the same or different providers. Repeat modifiers are specific modifiers used to indicate that a service is a repeat rather than a duplicate. Examples are Modifiers 76 and 77.
- For multiple radiology services of the same code provided by the same provider on the same date of service, bill the first unit as one unit on one line, followed by additional units of the same code on an additional line with Modifier 76.
- For radiology services of the same code provided by a different provider on the same date of service as another provider, bill all units on one line with Modifier 77.
- If a claim is denied as a duplicate, send copies of the radiology report, the denial statement, and the claim to the appropriate Department program officer for review. (See the Contact Us link on the website site index , then choose the Lab and Imaging pane.)
- For bilateral x-rays, bill on separate lines, one line with Modifier RT and one line with Modifier LT. The exception would be codes that are described as bilateral in their code description. These are to be billed on one line with one unit.
- Imaging providers must take particular care in the use of modifiers. Modifier TC is used when only the technical portion of the service is provided. The provider who interprets the results uses Modifier 26. When both technical and professional services are performed by the same provider, no modifier is required.
Mobile Imaging/Portable X-ray Supplier
- Mobile imaging providers must utilize modifiers appropriately. Modifier TC is used when only the technical portion of the service is provided. The provider who interprets the results uses Modifier 26. When both technical and professional services are performed by the same provider, no modifier is required.
- R0070 and R0075 must be billed based on the number of members served at one location.
- Modifiers UN, UP, UQ, UR OR US must be billed with R0075, depending on the number of members served at the location.
- Q0092 may be billed for the set-up fee for each imaging procedure furnished to a member as long as X-rays taken at different areas of the member’s body.
RHC/FQHC – Professional Services in Hospitals
RHC and FQHC practitioners (e.g., physicians, mid-level practitioners) performing services in a hospital setting should bill those services using the appropriate manual/rules that apply for that practitioner.
Billing Tips for Specific Services
Abortions
A completed Montana Healthcare Programs Physician Certification for Abortion Services (MA-37) form must be attached to every abortion claim or payment will be denied. This is the only form Medicaid accepts for abortions.
Anesthesia
With the exception of moderate conscious sedation, Montana Medicaid does not allow separate reporting of anesthesia for a medical or surgical procedure when it is provided by the practitioner performing the procedure.
When billing for anesthesia services, the date of service on the claim form must match the date of service that anesthesia was administered. If the surgery overlaps days, then bill the anesthesia only with the start date.
CPT states: For continuous services that last beyond midnight, use the date in which the service began and report the total units of time provided continuously.
The following payment method is used for anesthesia services, regardless of whether the service is billed by an anesthesiologist or another professional. Though the method differs from the RBRVS payment method, the two methods are linked and contain similar provisions.
- Use appropriate CPT anesthesia codes.
- Do not use surgery codes with an anesthesia modifier.
- For services where codes or definitions differ between the CPT and the American Society of Anesthesiologists Relative Value Guide, Medicaid adopts the CPT version.
- Include the total number of minutes on the claim. Medicaid will convert the number of minutes to the number of time units. Do not include the base units on the claim as the claims processing system determines the number of base units. (See the Submitting a Claim chapter in this manual.)
Bundled Services
Certain services with CPT codes (e.g., telephone advice, some pulse oximetry services) are covered by Medicaid but have a fee of zero. This means that the service is typically bundled with an office visit or other service. Since the bundled service is covered by Medicaid, providers may not bill the member separately for it.
Cosmetic Services
Include the prior authorization number on the claim. (See the Submitting a Claim chapter in this manual.)
EPSDT Well-Child Screens
- Bill for a complete screen using the appropriate evaluation and management (E/M) code for preventive medicine services.
- When billing for partial screens, use the appropriate preventive medicine code with Modifier 52 (reduced services).
- See also the EPSDT Well-Child chapter in the General Information for Providers manual.
- For well-child EPSDT indicators, see the Submitting a Claim chapter in this manual.
Family Planning Services
Contraceptive supplies and reproductive health items provided free to family planning clinics cannot be billed to Medicaid. When these supplies are not free to the clinic, providers associated with a family planning clinic can bill Medicaid for the following items:
Code - Item
A4266 - Diaphragm
A4267 - Male Condoms
A4268 - Female Condoms
A4269 - Spermicide
S4993 - Oral Contraceptives
340B drugs may be billed for acquisition costs only. For family planning indicators, see the Submitting a Claim chapter in this manual.
Immunizations
Per CPT, Codes 90460 and 90461 replace deleted Code 90465– Code 90468 for Vaccines for Children (VCF), a program for members ages 0–18.
Code 90460 (non-VFC) is billed for the first component of a vaccine. Code 90461 SL is not allowed by the VFC Program.
VFC codes are reviewed quarterly and updates may be implemented; please consult current provider notices to see if there are any changes.
Follow the CPT coding instructions as outlined in the CPT coding book for the proper use of these codes (i.e., face-to-face physician or qualified healthcare counseling time) member age, and add-on coding rules. Also, a combination of these two sets for the same date of service, member, and provider will result in an NCCI denial, with or without an NCCI modifier, because Codes 90471, 90472, 90473, and 90474 are component codes to Codes 90460 and 90461.
You may only bill for administrative services if performed by or under the direct supervision of a reimbursable professional (i.e., physician, mid-level). All administration of VFC vaccines must be billed on a CMS-1500.
The administration codes should have the appropriate modifier (SL) to be reimbursed for the federally mandated administration rate. Codes for the VFC supplied vaccines must be billed on the same claim with no charge ($0.00). See the fee schedule on the Physician page on the Provider Information website.
Note: If a significant separately identifiable Evaluation and Management (E/M) service (e.g., office or other outpatient services, preventive medicine services) is performed, the appropriate E/M service code with the appropriate modifier should be reported in addition to the vaccine and toxoid administrative codes.
Note: Administrative Code 90460 (VFC) may have multiple units per line because the code can be used for all VFCs. Codes 90471, 90473, and 90474 define route of administration.
Note: If a significant separately identifiable E/M service (e.g., office or other outpatient services, preventive medicine services) is performed, the appropriate E/M service code with the appropriate modifier should be reported in addition to the vaccine and toxoid administration codes.
Obstetrical Services
If the provider’s care includes prenatal (antepartum) and/or postnatal (postpartum) care in addition to the delivery, the appropriate global OB code must be billed. Antepartum care includes all visits until delivery, and there are different codes for specified numbers of visits. There are also different codes for antepartum and postpartum care when only one or the other is provided. Please review your CPT coding book carefully.
When billing a medical or surgical procedure, the date of service on the claim form must match the date of service that the procedure was performed. If the procedure has a global component and the provider saw the patient before and after the procedure, then the provider must bill the global procedure code on the claim form with the date associated for services rendered. For instance, if a vaginal delivery with antepartum and postpartum care (CPT 59400) is performed, it must be billed using the date of delivery as the from and to dates of service.
Reference Lab Billing
Under federal regulations, all lab services must be billed to Medicaid by the lab that performed the service. Modifier 90, used to indicate reference lab services, is not covered by Medicaid.
Sterilization
For elective sterilizations, a completed Informed Consent to Sterilization (MA-38) form must be attached to the claim for each provider involved or payment will be denied. No fields may be left blank, except for the Interpreter’s Statement. This form must be legible and accurate. If revisions are made, they must be made with a single line through the incorrect information and initialed by the party making the change. patient information may only be changed by the patient and must be initialed by the patient. Documentation must be included explaining why revisions were made. It is the provider’s responsibility to obtain a copy of the form from the primary or attending physician.
For medically necessary sterilizations (including hysterectomies, oophorectomies, salpingectomies, and orchiectomies), one of the following must be attached to the claim, or payment will be denied:
- A completed Medicaid Hysterectomy Acknowledgement form (MA-39) for each provider submitting a claim. It is the provider’s responsibility to obtain a copy of the form from the primary or attending physician. Complete only one section of this form. When no prior sterility (Section B) or life-threatening emergency (Section C) exists, the member (or representative, if any) and physician must sign and date Section A of this form prior to the procedure (see 42 CFR 441.250 for the federal policy on hysterectomies and sterilizations). Also, for Section A, signatures dated after the surgery date require manual review of medical records by the Department. The Department must verify that the member (and representative, if any) was informed orally and in writing, prior to the surgery, that the procedure would render the member permanently incapable of reproducing. The member does not need to sign this form when Sections B or C are used. Refer to the Forms page on the website for instructions on completing the form.
- For members who have become retroactively eligible for Medicaid, the physician must certify in writing that the surgery was performed for medical reasons and must document one of the following:
- The individual was informed prior to the hysterectomy that the operation would render the member permanently incapable of reproducing.
- The reason for the hysterectomy was a life-threatening emergency.
- The member was already sterile at the time of the hysterectomy and the reason for prior sterility.
When submitting claims for retroactively eligible members, attach a copy of the MA-160 (eligibility determination letter) to the claim if the date of service is more than 12 months earlier than the date the claim is submitted. For more information on sterilizations, see the Covered Services chapter in this manual.Surgical Services Medicaid does not provide additional payment for the operating room in a physician’s office. Medicaid pays facility expenses only to licensed hospitals and ambulatory surgical centers.
Reporting surgical services
Certain surgical procedures must not be reported together, such as:
- Procedures that are mutually exclusive based on the CPT code description or standard medical practice.
- When both comprehensive and component procedures are performed, only the comprehensive procedure should be billed.
- When the CPT manual describes several procedures of increasing complexity, only the code describing the most extensive procedure performed should be reported.
Medicaid edits for some surgical services using Medicaid’s National Correct Coding Initiative (NCCI) edits and performs post-payment review on others. See Coding Resources earlier in this chapter for more information on NCCI.
Assistant at Surgery
When billing for an assistant at surgery, refer to the current Medicaid fee schedule to see if an assist is allowed for that procedure.
If an assistant at surgery does not use the appropriate modifier, then either the assistant’s claim or the surgeon’s claim (whichever is received later) will be denied as a duplicate service.
Physicians must bill assistant at surgery services using the appropriate surgical procedure code and Modifier 80, 81, or 82.
Mid-level practitioners must bill assistant at surgery services under their own NPI and taxonomy using the appropriate surgical procedure code and Modifier AS, 80, 81, or 82.
Global surgery periods: Global surgery periods are time spans assigned to surgery codes. During these time spans, services related to the surgery may not be billed. Group practice members that are of the same specialty must bill Medicaid as if a single practitioner provided all related follow-up services for a member. For example, Dr. Armstrong performs orthopedic surgery on a member. The member comes in for a follow-up exam, and Dr. Armstrong is on vacation. Dr. Armstrong’s partner, Dr. Black, performs the follow-up. Dr. Black cannot bill this service to Medicaid because the service was covered in the global period when Dr. Armstrong billed for the surgery.
For major surgeries, this span is 90 days and includes the day prior to the surgery and the following services: post-operative surgery related care and pain management and surgically-related supplies and miscellaneous services.
For minor surgeries and some endoscopies, the spans are either 1 day or 10 days. They include any surgically related follow-up care and supplies on the day of surgery, and for a 10-day period after the surgery.
For a list of global surgery periods by procedure code, see the current Department fee schedule for your provider type.
If the CPT manual lists a procedure as including the surgical procedure only (i.e., a “starred” procedure) but Medicaid lists the code with a global period, the Medicaid global period applies. Almost all Medicaid fees are based on Medicare relative value units (RVUs), and the Medicare relative value units were set using global periods even for starred procedures. Montana Medicaid has accepted these RVUs as the basis for its fee schedule.
In some cases, a physician (or the physician’s partner of the same specialty in the same group practice) provides care within a global period that is unrelated to the surgical procedure. In these circumstances, the unrelated service must be billed with the appropriate modifier to indicate it was not related to the surgery.
Telemedicine Services
When performing a telemedicine consult, use the appropriate CPT E/M consult code. The place of service is the location of the provider providing the telemedicine service. Medicaid does not pay for network use or other infrastructure charges.
Please refer to the Telemedicine section of the General Information for Providers Manual.
Transplants
Include the prior authorization number on the claim. See the Submitting a Claim chapter in this manual. All providers must have their own prior authorization number for the services. For details on obtaining prior authorization, see the Prior Authorization chapter in this manual.
Weight Reduction
Providers who counsel and monitor members on weight reduction programs must bill Medicaid using appropriate E/M codes.
Unlisted Procedures
Unlisted CPT or HCPCS codes and supporting documentation are to be sent to the Department at the address below for review. If the claim is submitted electronically, the documentation must be sent as a paperwork attachment. (See Paperwork Attachment instruction section below.)
Claim Review
Physician-Related Services
P.O. Box 202951
Helena, MT 59624
Submitting Electronic Claims
Providers who submit claims electronically experience fewer errors and quicker payment. Claims may be submitted using the methods below. For detailed submission methods, see the electronic submissions manual on the Electronic Billing page of the website.
- WINASAP 5010. This free software provided by Conduent allows for the creation of basic claim submissions. Please note that this software is not compatible with Windows 10 and has limited support as it is free software.
o Utilizes either a dial-up modem or submissions through the Montana Access to Health (MATH) Web Portal.
o Requires completion of the X12N Transaction Packet to allow for claim submissions.
- Clearinghouses/Contracted Claim Submitter. Providers can make arrangements with a clearinghouse/contracted claim submitter for claim submission. Please note that the clearinghouse must be enrolled to submit claims to Montana Medicaid.
- Montana Access to Health (MATH) Web Portal. A secure website that allows providers to verify eligibility, check claim status, and view medical claims history. Valid X12N files can be uploaded through this website.
o Requires completion of the X12N Transactions Packet to allow for claim submissions.
- MoveIt DMZ. This secure transfer protocol is for providers and clearinghouses that submit large volumes of files (in excess of 20 per day) or are regularly submitting files larger than 2 MB. This utilizes SFTP and an intermediate storage area for the exchange of files.
o A request for this must be made through Conduent Provider Relations for established trading partners.
Providers should be familiar with federal rules and regulations related to electronic claims submission.
Billing Electronically with Paper Attachments
When submitting claims that require additional supporting documentation, the Attachment Control Number field must be populated with an identifier. Identifier formats can be designed by software vendors or clearinghouses, but the preferred method is the provider’s NPI followed by the member’s ID number and the date of service, each separated by a dash:
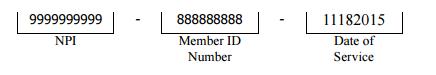
The supporting documentation must be submitted with a Paperwork Attachment Cover Sheet under the forms button on the provider website home page. The number in the paper Attachment Control Number field must match the number on the cover sheet.
Electronic claims that have the PWK indicator will pend for 30 days awaiting the appropriate paperwork to be submitted using the above procedure. If the claim has no PWK indicator, claims will proceed through the normal adjudication process.
Submitting Paper Claims
For instructions on completing a paper claim, see the Submitting a Claim chapter in this manual. Unless otherwise stated, all paper claims must be mailed to:
Claims Processing
P.O. Box 8000
Helena, MT 59604
Claim Inquiries
Contact Provider Relations for general claim questions and questions regarding member eligibility, payments, and denials.
Paper claims are often returned to the provider before they can be processed, and many other claims (both paper and electronic) are denied. To avoid unnecessary returns and denials, double-check each claim to confirm the following items are included and accurate.
How to Avoid the Most Common Billing Errors
Reasons for Return or Denial:
Provider’s NPI and/or taxonomy missing or invalid
Preventing Returned or Denied Claims:
Verify the correct NPI and taxonomy are on the claim.
Reasons for Return or Denial:
Authorized signature missing.
Preventing Returned or Denied Claims:
Each claim must have an authorized signature belonging to the provider, billing clerk, or office personnel. The signature may be typed, stamped, or handwritten.
Reasons for Return or Denial:
Signature date missing.
Preventing Returned or Denied Claims:
Each claim must have a signature date.
Reasons for Return or Denial:
Incorrect claim form used.
Preventing Returned or Denied Claims:
The claim must be the correct form for the provider type. Services covered in this manual require a CMS-1500 claim form (or electronic professional claim).
Reasons for Return or Denial:
Information on claim form not legible.
Preventing Returned or Denied Claims:
Information on the claim form must be legible. Use dark ink and center the information in the field. Information must not be obscured by lines.
Reasons for Return or Denial:
Recipient number not on file, or recipient was not eligible on date of service.
Preventing Returned or Denied Claims:
Before providing services to the member:
View the member’s eligibility information at each visit. Medicaid eligibility may change monthly.
Verify member eligibility by using one of the methods described in the Member Eligibility and Responsibilities chapter of the General Information for Providers manual.
Reasons for Return or Denial:
Duplicate claim.
Preventing Returned or Denied Claims:
Please check all remittance advices for previously submitted claims before resubmitting.
When making changes to previously paid claims, submit an adjustment form rather than a new claim. (See Remittance Advices and Adjustments in this manual.)
Please allow 45 days for the Medicare/Medicaid Part B crossover claim to appear on the remittance advice before submitting the claim directly to Medicaid.
Reasons for Return or Denial:
Procedure requires Passport provider referral – No Passport provider number on claim.
Preventing Returned or Denied Claims:
A Passport provider number must be on the claim when such a referral is required. See the Passport to Health manual.
Reasons for Return or Denial:
TPL on file and no credit amount on claim.
Preventing Returned or Denied Claims:
If the member has other insurance (or Medicare), bill the other carrier before Medicaid. See Coordination of Benefits in this manual.
If the member’s TPL coverage has changed, providers must notify Conduent TPL unit before submitting a claim.
End of Billing Procedures Chapter
Submitting a Claim
The services described in this manual are billed either electronically on a professional claim or on a CMS-1500 paper claim form. Claims submitted with all of the necessary information are referred to as clean and are usually paid in a timely manner. (See the Billing Procedures chapter in this manual.)
Claims are completed differently for the different types of coverage a member has. The following are accepted codes for completing box 24h:
| Code | Member/Servide | Purpose |
|---|---|---|
| 1 | EPSDT | Used when the member is under age 21. |
| 2 | Family Planning | Used when providing family planning services. |
| 3 | EPSDT and family planning | Used when the member is under age 21 and is receiving family planning services. |
| 4 | Pregnancy (any service provided to a pregnant woman) | Used when providing services to to pregnant women. |
| 6 | Nursing facility member | Used when providing services to nursing facility residents. |
Unless otherwise stated, all paper claims must be mailed to the following address:
Claims Processing
P.O. Box 8000
Helena, MT 59604
CMS-1500 Agreement
Your signature on the CMS-1500 constitutes your agreement to the terms presented on the back of the form. This form is subject to change by the Centers for Medicare and Medicaid Services (CMS).
Avoiding Claim Errors
Claims are often denied or even returned to the provider before they can be processed. To avoid denials and returns, double-check each claim to confirm the following items are accurate. For more information on returned and denied claims, see the Billing Procedures chapter in this manual.
Common Claim Errors
Claim Errors:
Required field is blank.
Prevention:
If a required field is blank, the claim may either be returned or denied.
Claim Errors:
Member ID number missing or invalid.
Prevention:
This is a required field; verify that the member’s Medicaid ID number is listed as it appears on the member’s eligibility information.
Claim Errors:
Patient name missing.
Prevention:
This is a required field; check that it is correct.
Claim Errors:
Provider NPI and taxonomy missing or invalid.
Prevention:
Verify the correct NPI and taxonomy are on the claim.
Claim Errors:
Referring or Passport provider name and ID number missing.
Prevention:
When a provider refers a member to another provider, include the referring provider’s name and ID number or Passport number. See the Passport to Health manual.
Claim Errors:
Prior authorization number missing.
Prevention:
When prior authorization is required for a service, the prior authorization number must be listed on the claim. See the Prior Authorization chapter in this manual.
Claim Errors:
Not enough information regarding other coverage.
Prevention:
When a member has other coverage, related fields become required.
Claim Errors:
Authorized signature missing.
Prevention:
Each claim must have an authorized signature belonging to the provider, billing clerk, or office personnel. The signature may be typed, stamped, or hand-written.
Claim Errors:
Signature date missing.
Prevention:
Each claim must have a signature date.
Claim Errors:
Incorrect claim form used.
Prevention:
Services covered in this manual require a CMS-1500 claim form or an electronic professional claim.
Claim Errors:
Information on claim form not legible.
Prevention:
Information on the claim form must be legible. Use dark ink and center the information in the field. Information must not be obscured by lines.
Claim Errors:
Medicare EOMB not attached.
Prevention:
When Medicare is involved in payment on a claim, the Medicare EOMB must be attached to the claim or it will be denied.
Other Programs
This chapter also applies to claims forms completed for Mental Health Services Plan (MHSP) services and Healthy Montana Kids (HMK)/CHIP eyeglass services.
End of Submitting a Claim Chapter
How Payment Is Calculated
Overview
Though providers do not need the information in this chapter in order to submit claims to the Department, the information allows providers to understand how payment is calculated and to predict approximate payment for particular claims.
The RBRVS Fee Schedule
Most services by provider types covered in this manual are reimbursed for using he Department’s RBRVS fee schedule. RBRVS stands for Resource-Based Relative Value Scale. The fee schedule includes CPT codes and HCPCS codes. Within the CPT coding structure, only anesthesia services and clinical lab services are not reimbursed for using the RBRVS fee schedule.
NOTE: Many Medicaid payment methods are based on Medicare, but there are differences. In these cases, the Medicaid method prevails.
RBRVS was developed for the Medicare program. Medicare does a major update annually, with smaller updates performed quarterly. Montana Medicaid’s RBRVS-based fee schedule is based largely on the Medicare model, with a few differences as described below. By adapting the Medicare model to the needs of the Montana Medicaid program, the Department was able to take advantage of the research performed by the federal government and national associations of physicians and other healthcare professionals. RBRVS-based payment methods are widely used across the U.S. by Medicaid programs, workers’ compensation plans and commercial insurers.
Fee Calculation
Each fee is the product of a relative value times a conversion factor.
Basis of Relative Values
For almost all services, Medicaid uses the same relative values as Medicare in Montana. Nationally, Medicare adjusts the relative values for differences in practice costs between localities, but Montana is considered a single locality. For fewer than 1% of codes, relative values are not available from Medicare. For these codes, the Department has set the fee.
When Medicaid payment differs from the fee schedule, consider the following:
- The Department pays the lower of the established Medicaid fee or the provider’s charge
- Modifiers. (See Other Modifiers in this chapter.)
- Provider type (See Professional Differentials in this chapter.)
- Place of service (See Site of Service Differential in this chapter.)
- Date of service (Fees for services may change over time.)
- Also check for cost sharing and Medicare or TPL payments shown on the remittance advice.
Composition of Relative Values
For each code, the relative value is the sum of a relative value for the work effort (including time, stress, and difficulty), the associated transitional practice expense, and the associated malpractice expense.
Site of Service Differential
The Medicare program has calculated two sets of relative values for each code: one reflects the practitioner’s practice cost of performing the service in an office and one reflects the practitioner’s practice cost of performing the service in a facility.
Medicaid typically pays a lower fee if the service is provided in a facility because Medicaid typically also pays the facility.
Conversion Factor
The Department sets the conversion factor for the state fiscal year (July through June) and it is listed on the fee schedule.
Policy Adjuster
To encourage access to maternity services and family planning services, the Department increases fees for these codes using a policy adjuster that increases the fee. The fee listed on the fee schedule includes the policy adjuster.
Global Periods
For many surgical services and maternity services, the fee covers both the service and all related care within a specified global period. For almost all such codes, the global periods used by Medicaid are identical to those used by Medicare, but in cases of differences the Medicaid policy applies. See the Billing Procedures chapter in this manual for information on global periods.
Professional and Technical Components
Many imaging services and some diagnostic services are divided into the technical component (performing the test) and the professional component (interpreting the test). A practitioner who only performs the test would bill the service with modifier TC; a practitioner who only interprets the test would bill Modifier 26; and a practitioner who performs both components would bill the code without a modifier. Performance of both components is called the global service. The fee schedule has separate fees for each component and for the global service.
Other Modifiers
Under the RBRVS fee schedule, certain other modifiers also affect payment. Modifiers affecting reimbursement are listed in the table on the next page.
How Modifiers Change Pricing
- Modifiers may not be applicable for all services.
- For services paid via the RBRVS fee schedule, the fee schedule shows the list of services for which Modifiers 26, TC, 50, 51, 62, 66, and 80 apply.
- If a modifier does not appear in the list below, then it does not affect pricing.
- Use of Modifier 22 is prohibited for mental health services. In 2013, the CPT manual added two codes specifically for crisis with instructions and guidance for providers.
- The list shows summary modifier descriptions. See the CPT and HCPCS coding books for the full text.
Modifiers That Affect Pricing
Modifier: 22 Definition: Increased procedural service
How Payment is Affected: The services is paid at 110% of the fee.
Modifier: 26 Definition: Professional component
How Payment is Affected: For services paid via the RBRVS fee schedule, see the specific service. For other services, payment equals 40% of the fee.
Modifier: 47 Definition: Anesthesia by surgeon
How Payment is Affected: Modifier not allowed.
Modifier: 50 Definition: Bilateral procedure
How Payment is Affected: The procedure is paid at 150% of the fee.
Modifier: 51 Definition: Multiple procedures
How Payment is Affected: Each procedure is paid at 50% of the fee.
Modifier: 52 Definition: Reduced service
How Payment is Affected: The service is paid at 50% of the fee.
Modifier: 53 Definition: Discontinued procedure
How Payment is Affected: The service is paid at 50% of the fee.
Modifier: 54 Definition: Surgical care only
How Payment is Affected: The service is paid at 75% of the fee.
Modifier: 55 Definition: Postoperative management only
How Payment is Affected: The service is paid at 25% of the fee.
Modifier: 56 Definition: Preoperative management only
How Payment is Affected: The service is paid at 25% of the fee.
Modifier: 59 Definition: Distinct procedural service
How Payment is Affected: The service is paid at 50% of the fee unless the procedure is identified as ‘modifier 51 exempt’ or ‘add-on’.
Modifier: 62 Definition: Two surgeons
How Payment is Affected: Each surgeon is paid at 62.5% of the fee.
Modifier: 80 Definition: Assistant surgeon
How Payment is Affected: The service is paid at 16% of the fee.
Modifier: 81 Definition: Minimum assistant surgeon
How Payment is Affected: The service is paid at 16% of the fee.
Modifier: 82 Definition: Assistant surgeon; qualified resident surgeon not available
How Payment is Affected: The service is paid at 16% of the fee.
Modifier: 90 Definition: Reference laboratory
How Payment is Affected: Modifier not allowed
Modifier: AD Definition: Medical supervision of more than four concurrent anesthesia procedures
How Payment is Affected: Each service is paid at 52.5% of the fee.
Modifier: AS Definition: Physician assistant, nurse practitioner or clinical nurse specialist as assistant at surgery
How Payment is Affected: The service is paid at 16% of the fee.
Modifier: QK Definition: Medical supervision of 2–4 concurrent anesthesia procedures
How Payment is Affected: Each service is paid at 52.5% of the fee.
Modifier: QX Definition: Certified registered nurse anesthetist service: medically directed by MD
How Payment is Affected: Each service is paid at 52.5% of the fee.
Modifier: QZ Definition: Certified registered nurse anesthetist service without medical direction
How Payment is Affected: The modifier does not reduce the fee, but a professional differential of 90% is applied due to provider type. See Professional Differentials in this chapter.
Modifier: TC Definition: Technical component
How Payment is Affected: For services paid via the RBRVS fee schedule, see the specific service. For other services, payment equals 60% of the fee.
Professional Differentials
Mid-level practitioners generally receive 90% of the fee that a physician would receive for the same service. The exception is that mid-level practitioners receive 100% of the fee for immunizations, family planning, injectables, lab and pathology services, radiology, cardiography and echocardiography, and services to members under age 21 (i.e., well-child EPSDT services).
Charge Cap
For the services covered in this manual, Medicaid pays the lower of the established Medicaid fee or the provider’s charge.
Bundled Codes
A few services are covered by Medicaid but have a fee of zero, meaning that payment for the service is considered bundled into the payment for services that are usually provided with it. Because these services are covered by Medicaid, providers may not bill members for them on a private-pay basis.
Status Codes
The Medicare physician fee schedule includes status codes that show how each services is reimbursed. Medicaid also uses status codes.
Anesthesia Services
With the exception of moderate conscious sedation, Montana Medicaid does not allow separate reporting of anesthesia for a medical or surgical procedure when it is provided by the practitioner performing the procedure.
When billing for anesthesia services, the date of service on the claim form must match the date of service that anesthesia was administered. If the surgery overlaps days, then bill the anesthesia only with the start date.
NOTE: When billing Medicaid for anesthesia services, enter the number of minutes in the Units field of the CMS-1500 claim form.
CPT states: For continuous services that last beyond midnight, use the date in which the service began and report the total units of time provided continuously.
The following payment method is used for anesthesia services, regardless of whether the service is billed by an anesthesiologist or another professional. Though the method differs from the RBRVS payment method, the two methods are linked and contain similar provisions.
Time Units
A unit of time for anesthesia is 15 minutes, though Medicaid does pay for partial units. Providers enter the number of minutes on the claim; the claims processing contractor then converts the minutes to time units.
Base Units
Base units are adopted by Medicaid from the schedule of base units used by Medicare. Base units are calculated by the American Society of Anesthesiologists. Providers do not enter the number of base units on the claim.
Fee Calculation
For a particular service, Medicaid payment is calculated as follows: (Time units + base units) x anesthesia conversion factor = payment
Modifiers
Payment for anesthesia services is affected by the modifier pricing rules shown in this chapter; take note of the modifiers for anesthesia care provided under medical supervision. Medicaid follows Medicare in not paying extra for the patient status Modifiers P1 to P6.
Clinical Lab Services (ARM 37.85.212)
In general, Medicaid pays the same fees for clinical lab services as Medicare pays in Montana. If a Medicare fee is not available for a lab test covered by Medicaid, then payment is calculated by looking at the average charge and the amounts paid by other payers.
Vaccines and Drugs Provided within the Office
Many vaccines are available for free to physician offices through the Vaccines for Children (VFC) program. For information on obtaining these vaccines, call (406) 444-5580. For these vaccines, Medicaid does not pay separately. Medicaid does pay for the administration of the vaccine, however. Medicaid pays for most vaccines not available through the VFC program. (See the Immunizations section of the Billing Procedures chapter in this manual.)
Reimbursement for physician administered drugs (PAD), which are billed using HCPCS codes is made according to the Department’s fee schedule. The Department’s fee schedule is based on the Medicare Average Sale Price (ASP) Fee Schedule if there is an ASP fee, or the RBRVS fee if there is an RBRVS fee. If there is no ASP or RBRVS fee then the fee is calculated by National Drug Code (NDC) using the estimated acquisition cost to set reimbursement. Most must be billed with a HCPCS code and include the NDC, unit type, and number of units.
How Cost Sharing Is Calculated on Medicaid Claims
Member cost sharing fees are a set dollar amount per visit. (See the Cost Sharing section in the Billing Procedures chapter in the General Information for Providers Manual) The member’s cost sharing amount is shown on the remittance advice and deducted from the Medicaid allowed amount.
How Payment Is Calculated on TPL Claims
When a member has coverage from both Medicaid and Medicare, Medicare is the primary payer as described in the Coordination of Benefits chapter of this manual. Medicaid then makes a payment as the secondary payer. For the provider types covered in this manual, Medicaid’s payment is calculated so that the total payment to the provider is either the Medicaid allowed amount less the Medicare paid amount or the sum of the Medicare coinsurance and deductible, whichever is lower. This method is sometimes called “lower of” pricing.
Other Department Programs
The payment method described in this chapter also applies to services provided under the Mental Health Services Plan (MHSP).
End of How Payment Is Calculated Chapter
Appendix A: Forms
- Individual Adjustment Request
- Physician Certification for Abortion Services (MA-37)
- Informed Consent to Sterilization (MA-38)
- Medicaid Hysterectomy Acknowledgement (MA-39)
- Paperwork Attachment Cover Sheet
End of Appendix A: Forms Chapter
Appendix B: Place of Service Codes
End of Appendix B: Place of Service Codes Chapter
Definitions and Acronyms
HCPCS/CPT Codes
Montana Medicaid adds many codes from the yearly edition of the Current Procedural Terminology and HCPCS manuals. Refer to the fee schedules posted on the Provider Information website. If you are billing unlisted J codes (e.g., J3490), verify that a new J code does not exist before you bill. If one does not exist send the claim with a copy of the invoice directly to the State office.
Nondiscrimination (ARM 37.85.402)
The Department does not exclude, deny benefits to, or otherwise discriminate against any person on the basis of race, color, national origin, age, sex, handicap, political beliefs, religion or disability. This includes the admission to, participation in, or receipt of services or benefits of any of its programs, activities or employment, whether carried out by the Department or through a contractor or other entity.
For questions or to file a complaint alleging violations, contact the Montana Human Rights Bureau (800) 542-0807 or (406) 444-2884.
To file a complaint with the Office of Civil Rights, visit: http://www.hhs.gov/ocr/civilrights/complaints/index.html.
Sports Physicals
A sports physical is typically a non problem-oriented encounter in which the provider evaluate and certifies a patient’s involvement in organized sports, such as high school football. If a comprehensive history and physical examination are performed, report the age-appropriate code from the preventive medicine series. If less than a comprehensive history and exam, are performed, report the appropriate level office or other outpatient evaluation and management visit code.
Tamper-Resistant Prescription Pads
Federal law requires written Medicaid prescriptions to be on tamper-resistant pads. The Department, in accordance with CMS guidance, requires that a Medicaid prescription pad contain all of the following.
- One or more industry-recognized features designed to prevent unauthorized copying of a completed or blank prescription form,
- One or more industry-recognized features designed to prevent the erasure or modification of information written on the prescription by the prescriber; and
- One or more industry-recognized features designed to prevent the use of counterfeit prescription forms.
End of Definitions and Acronyms Chapter
Index
Previous editions of this manual contained an index.
This edition has three search options.
- Search the whole manual. Open the Complete Manual pane. From your keyboard press the Ctrl and F keys at the same time. A search box will appear. Type in a descriptive or key word (for example "Denials". The search box will show all locations where denials discussed in the manual.
- Search by Chapter. Open any Chapter tab (for example the "Billing Procedures" tab). From your keyboard press the Ctrl and F keys at the same time. A search box will appear. Type in a descriptive or key word (for example "Denials". The search box will show where denials discussed in just that chapter.
- Site Search. Search the manual as well as other documents related to a particular search term on the Montana Healthcare Programs Site Specific Search page.
End of Index Chapter
End of Physician-Related Services Manual