General Information for Providers Manual
Printing the manual material found at this website for long-term use is not advisable. Department Policy material is updated periodically and it is the responsibility of the users to check that the policy they are researching or applying has the correct effective date for their circumstances.
If you experience any difficulty opening a section or link from this page, please email the webmaster.
How to Search this manual:
This edition has three search options.
- Search the whole manual. Open the Complete Manual pane. From your keyboard press the Ctrl and F keys at the same time. A search box will appear. Type in a descriptive or key word (for example "Denials"). The search box will show all locations where denials discussed in the manual.
- Search by Chapter. Open any Chapter tab (for example the "Billing Procedures" tab). From your keyboard press the Ctrl and F keys at the same time. A search box will appear. Type in a descriptive or key word (for example "Denials"). The search box will show where denials discussed in just that chapter.
- Site Search. Search the manual as well as other documents related to a particular search term on the Montana Healthcare Programs Site Specific Search page.
Prior manuals may be located through the provider website archives.
General Information for Providers Manual
Updated 02/20/2020
General Information for Providers Manual
To print this manual, right click your mouse and choose "print". Printing the manual material found at this website for long-term use is not advisable. Department Policy material is updated periodically and it is the responsibility of the users to check and make sure that the policy they are researching or applying has the correct effective date for their circumstances.
Update Log
Publication History
This publication supersedes all versions of previous general information provider handbooks. This publication is to be used in conjunction with provider type manuals. Published by the Montana Department of Public Health and Human Services, February 2002.
Updated September 2002, October 2003, September 2004, November 2004, April 2005, April 2008, February 2012, April 2012, June 2014, July 2014, September 2014, November 2014, August 2015, November 2015, January 2016, July 2016, August 2016, February 2017, September 2017, November 2017, April 2018, June 2018, May 2019, November 2019, January 2020, February 2020.
CPT codes, descriptions and other data only are copyright 1999 American Medical Association (or such other date of publication of CPT). All Rights Reserved. Applicable FARS/DFARS Apply.
Update Log
02/20/2020
SURS and Billing Procedures chapters updated to include acceptable minutes for billing a 15- minute unit of service.
01/01/2020
- Cost Share references removed from the Provider Requirements, Member Eligibility and Responsibility, and Billing Procedures Chapters.
- Term "Medicaid" replaced with "Montana Healthcare Programs" throughout the manual.
- Terms "client" and "patient" replaced with "member".
11/18/2019
The EPSDT Well-Child Chapter language was updated to included current age, rule, and service information.
05/03/2019
The Provider Requirements Chapter was revised to include rule language for usual and customary billing practices. The Billing Procedures Chapter was revised to included updated NDC information.
06/04/2018
Removed commercial resource references.
04/30/2018
The Outpatient Clinic Services section of the Billing Procedure Chapter was updated to include current provider-based clinic status.
11/24/2017
The Billings Procedure chapter was updated with current electronic submission information.
09/21/2017
General Information for Providers Manual converted to an HTML format and adapted to 508 Accessibility Standards. An additional paragraph was added under the EPSDT Well Child chapter regarding caregiver depression screening coverage. Language was changed regarding manual maintenance in the Introduction chapter.
02/06/2017
In summary, the Telemedicine Chapter was added as a new chapter and the Medically Needy section of the Member Responsibilities Chapter page 6.5 was updated.
08/02/2016
The Introduction contains updated links in the HELP section.
Cost Share was updated in the Billings Procedure.
A duplicate word was removed in the RA chapter.
The Cover Page was changed to reflect the current date of the new General Manual revision.
07/12/2016
General Information for Providers, July 2016
Table of Contents was amended by changing the title of “Basic Medicaid Waiver” to “Waiver for Additional Services and Populations (formerly Basic Medicaid Waiver)”.
Index was amended by changing the title of “Basic Medicaid Waiver” to “Waiver for Additional Services and Populations (formerly Basic Medicaid Waiver)”.
Page 1.3 changed the title “Basic Medicaid Waiver for Additional Services and Populations” to “Waiver for Additional Services and Populations (formerly Basic Medicaid Waiver)”.
01/19/2016
General Information for Providers, January 2016: Introduction Regarding HELP Plan Information
01/15/2016
General Information for Providers, January 2016: Introduction Regarding HELP Plan Information
12/31/2015
General Information for Providers, January 2016: HELP Plan-Related Updates and Others
11/17/2015
General Information for Providers, November 2015: Billing Procedures, Revenue Codes 25X and 27X
07/31/2015
General Information for Providers, August 2015: Entire Manual
11/19/2014
General Information for Providers, November 2014: Billing Procedures
10/08/2014
General Information for Providers, September 2014: Billing Procedures
07/22/2014
General Information for Providers, July 2014: Member Eligibility and Responsibilities
06/30/2014
General Information for Providers, June 2014: General Information for Providers
If information is found on the website, it has been removed from the manual, and a link to the source is provided.
04/13/2012
General Information for Providers, April 2012: Medicaid Covered Services and Member Eligibility
End of Update Log Chapter
Table of Contents
Key Contacts and Key Websites
Introduction
Administrative Rules of Montana (ARM) Rule References
Manual Organization
Manual Maintenance
Provider Training Opportunities
Contractor Services
Montana Healthcare Programs
Waiver for Additional Services and Populations
Medicaid Expansion
Other Programs
Provider Requirements
Provider Enrollment
Authorized Signature (ARM 37.85.406)
Provider Rights
EPSDT Well-Child
EPSDT Well-Child Check-Ups
EPSDT Provider Resources
Additional Services Under EPSDT
Who Can Provide EPSDT Screenings?
The Well-Child Screen
Initial/Interval History
Developmental Assessments
Appropriate Developmental Surveillance
Depression Screening
Alcohol and Drug Use Screen
Nutritional Screen
Unclothed Physical Inspection
Vision Screen
Hearing Screen
Autism Screen
Critical Congenital Heart Defect Screen
Laboratory Tests
Hematocrit and Hemoglobin
Blood Lead Level
Tuberculin Screening
Dyslipidemia Screening
STI/HIV Screening
Cervical Dysplasia Screening
Immunizations
Dental Screen
Discussion and Counseling/Anticipatory Guidance
Prior Authorization
What Is Prior Authorization?
Telemedicine
Program Overview
When to Use Telemedicine
Telemedicine Confidentiality Requirements
General Billing Instructions
Originating Provider Requirements
Distance Provider Requirements
Member Eligibility and Responsibilities
Montana Healthcare Programs ID Cards
Verifying Member Eligibility
Inmates in Public Institutions (ARM 37.82.1321)
Presumptive Eligibility
Retroactive Eligibility
Coverage for the Medically Needy
Montana Breast and Cervical Cancer Treatment Program
When a Member Has Other Coverage
When a Member Has Medicare
When a Member Has TPL (ARM 37.85.407)
When Members Are Uninsured
Member Responsibilities
Other Programs
Money Follows the Person Demonstrated Grant
Surveillance and Utilization Review (SURS)
Claims Review (MCA 53-6-111, ARM 37.85.406)
Statewide Surveillance and Utilization Control Program (42 CFR 456.3)
Key Points
Billing Tips
Billing Procedures
Claim Forms
Timely Filing Limits (ARM 37.85.406)
When to Bill Montana Healthcare Programs Members (ARM 37.85.406)
Member Co-Payment (ARM 37.85.204)
Billing for Members with Other Insurance
Billing for Retroactively Eligible Members
Coding Tips
Medicaid National Correct Coding Initiative
Number of Lines on Claim
Multiple Services on Same Date
Span Bills
Reporting Service Dates
Using Modifiers
Billing Tips for Specific Services
Outpatient Clinic Services
Partial Hospitalization
Submitting a Claim
Claim Inquiries
The Most Common Billing Errors and How to Avoid Them
Other Programs
Remittance Advices and Adjustments
The Remittance Advice
Credit Balance Claims
Rebilling and Adjustments
Payment and the Remittance Advice
Other Programs
Appendix A: Forms
Appendix B: Place of Service Codes
Appendix C: Local Offices of Public Assistance
Definitions and Acronyms
Index
End of Table of Contents Chapter
Key Contacts and Key Websites
Additional information is available through the Provider Information Website.
Providers can stay informed with the latest Montana Healthcare Programs news and events, provider manuals, provider notices, fee schedules, newsletters, forms, and more.
The monthly Montana Healthcare Programs online newsletter, the Claim Jumper, Covers Montana Healthcare Programs program changes and include a list of documents posted to the Provider Information Website during that time frame.
For additional contacts see the Contact Us link in the left menu on the Montana Healthcare Programs Provider Information website, for a list of contacts and websites.
End of Key Contacts and Key Websites Chapter
Key Contacts and Key Websites
End of Key Contacts and Key Websites Chapter
Introduction
The Montana Healthcare Programs program plays an essential role in providing health insurance for Montanans. Before the enactment of Medicare and Montana Healthcare Programs, healthcare for the elderly and the indigent was provided through a patchwork of programs sponsored by governments, charities, and community hospitals.
Today, Medicare is a federal program that provides insurance for persons aged 65 and over and for people with severe disabilities, regardless of income. Montana Healthcare Programs provides healthcare coverage to specific populations, especially low-income families with children, pregnant women, disabled people, and the elderly. Montana Healthcare Programs is administered by state governments under broad federal guidelines. Recent healthcare laws have greatly increased the number of people who qualify for Montana Healthcare Programs. See the Montana Healthcare Programs Program: Report to the 2017 Legislature.
Rule References
Providers must be familiar with current rules and regulations governing the Montana Healthcare Programs program. The provider manuals are meant to assist providers in billing Montana Healthcare Programs; they do not contain all Montana Healthcare Programs rules and regulations.
Rule citations in the text are a reference tool; they are not a summary of the entire rule. In the event that a manual conflicts with a rule, the rule prevails. Links to rules are available online on the provider type pages on the Provider Information website or at http://www.sos.mt.gov/ARM/index.asp.
Providers can order the Administrative Rules of Montana, including individual titles, online or by mail, through the Secretary of State website. Select the How to Order option in the Additional Resources section.
Manual Organization
The General Information for Providers manual provides answers to general Montana Healthcare Programs questions about provider enrollment, member eligibility, and surveillance and utilization review.
This manual is designed to work with Montana Healthcare Programs provider type manuals, which contain program information on covered services, prior authorization, and billing for specific services.
It is divided by chapters, and a table of contents and index allow providers to find answers to most questions. The margins contain important information and space for writing notes. For eligibility and coordination of benefit information, see the Member Eligibility and Responsibilities chapter in this manual. Provider-specific information is in provider type manuals. Contact Provider Relations at 1-800-624-3958 with questions.
Manual Maintenance
Manuals must be kept current.
Notification of manual updates are provided through the weekly web postings under “Recent Website Posts” on the home page of the provider website and under Provider Notices on the provider type page of the provider website. Older versions of the manual may be found through the Archive page on the Provider website. Printing the manual material found at this website for long-term use is not advisable. Department Policy material is updated periodically and it is the responsibility of the users to check and make sure that the policy they are researching or applying has the correct effective date for their circumstances.
Website Information
Additional information is available through the Provider Information website.
Providers can stay informed with the latest Montana Healthcare Programs news and events, download provider manuals/replacement pages, provider notices, fee schedules, newsletters, and forms. Other resources are also available. See the menu for links.
Provider Training Opportunities
Montana Healthcare Programs offers a variety of training opportunities that are announced on the Provider Information website and in the Claim Jumper newsletter. Recorded training sessions are available on the Training page of the website.
Contract Services
Montana Healthcare Programs works with various contractors who represent Montana Healthcare Programs through the services they provide. While it is not necessary for providers to know contractor duties, the information below is provided as informational.
- Conduent State Healthcare, LLC. Answers provider inquiries and enrolls providers in Montana Healthcare Programs and Passport to Health; processes claims for Montana Healthcare Programs, MHSP, HMK, pharmacy, dental, and eyeglasses, and HELP claims listed in the HELP Plan section.
- Mountain-Pacific Quality Health. Provides prior authorization for many Montana Healthcare Programs services.
- Magellan Montana Healthcare Programs Administration (dba First Health Services). Provides prior authorization, utilization review, and continued stay review for some mental health services.
Standard Montana Healthcare Programs
Standard Montana Healthcare Programs Benefits
All Montana Healthcare Programs members are eligible for Standard Montana Healthcare Programs services if medically necessary. Covered services include, but are not limited to, audiology services, clinic services, community health centers services, dental services, doctor visits, hospital services, immunizations, Indian Health Services, laboratory services, mental health services, Nurse First services, nursing facility, occupational therapy, pharmacy, public health clinic services, substance dependency services, tobacco cessation, transportation, vision services, well-child checkups, and x-rays.
Waiver for Additional Services and Populations (formerly Basic Montana Healthcare Programs Waiver)
This waiver includes individuals age 18 or older, with Severe Disabling Mental Illnesses (SDMI) who qualify for or are enrolled in the state-financed Mental Health Services Plan (MHSP), but are otherwise ineligible for Montana Healthcare Programs benefits and either have:
- Income 0–138% of the federal poverty level (FPL) and are eligible for or enrolled in Medicare; or
- Income 139–150% of the FPL regardless of Medicare status (they can be covered or not covered by Medicare and be eligible).
Members covered under this waiver receive Standard Montana Healthcare Programs benefits. To apply or for more information, contact the Addictive and Mental Disorders Division at 1-406-444-2878 or visit the BHDD website.
HELP Plan Benefits
The Montana Health and Economic Livelihood Partnership (HELP) Plan provides health coverage to adults ages 19–64 with incomes up to 138% of the FPL; who are not enrolled or eligible for Medicare; who are not incarcerated; and who are U.S. citizens or documented, qualified aliens who are Montana residents.
Most services will be administered through Blue Cross and Blue Shield of Montana (BCBSMT), a third party administrator, and some services will be administered through Conduent.
Services for the HELP Plan Processed by BCBSMT Most medical and behavior health services will be processed by BCBSMT, including:
- Behavioral Health (Mental Health and Substance Use Disorder)
- Convalescent Home (excludes Custodial Care)
- Durable Medical Equipment/Supplies
- Early and Periodic Screening, Diagnostic, and Treatment (EPSDT)
- Emergency
- Hospital
- Lab and X-Ray (Medical)
- Medical Vision and Exams
- Mid-Level
- Physician
- Preventive
- Rehabilitative and Habilitative
- Surgical
Services for the HELP Plan Processed by Conduent
- Audiology
- Dental
- Diabetes Prevention Program
- Eyeglasses
- Federally Qualified Health Center
- Hearing Aids
- Home Infusion
- Indian Health Services/Tribal Health
- Pharmacy
- Rural Health Clinic
- Transportation
Contact Information
• HELP Plan Provider Services 1 (877) 296-8206 (BCBSMT)
• BCBSMT website http://www.bcbsmt.com/mthelpplan
• HELP Plan Provider Services 1 (800) 624-3958 (Conduent)
• Provider Information website https://medicaidprovider.mt.gov
• HELP Plan Information website https://dphhs.mt.gov/healthcare
Other Programs
In addition to Montana Healthcare Programs, the Department of Public Health and Human Services (DPHHS, the Department) offers other programs. In addition to those listed below, other subsidized health insurance plans may be available from programs funded by the federal government or private organizations.
Chemical Dependency Bureau State Paid Substance Dependency/Abuse Treatment Programs
For individuals who are ineligible for Montana Healthcare Programs and whose family income is within program standards. For more information on these programs, call 406-444-3964 or visit https://dphhs.mt.gov/BHDD/SubstanceAbuse/index.
Children’s Mental Health Bureau Non-Montana Healthcare Programs Services
Funding sources for short-term use, not entitlement programs. Planning efforts toward family reunification are the primary objective, with transition planning essential for youth in out-of-home care. For information, call 406-444-4545, or refer to the Non-Montana Healthcare Programs Services Provider Manual at https://dphhs.mt.gov/BHDD/cmb/Manuals.
Children’s Special Health Services (CSHS)
A program that assists children with special healthcare needs who are not eligible for Montana Healthcare Programs by paying medical costs, finding resources, and conducting clinics. For more information, call 406-444-3622 (local) or 800-762-9891 (toll-free in Montana) or visit https://dphhs.mt.gov/ecfsd/cshs/index.
Health Insurance Premium Payment (HIPP)
A program that allows Montana Healthcare Programs funds to be used to pay for private health insurance coverage when it is cost effective to do so. Visit https://dphhs.mt.gov/MontanaHealthcarePrograms/HIPP.
Healthy Montana Kids (HMK)
HMK offers low-cost or free health insurance for low-income children younger than 19. Children must be uninsured U.S. citizens or qualified aliens, Montana residents who are not eligible for Montana Healthcare Programs. Visit https://dphhs.mt.gov/HMK.
Mental Health Services Plan (MHSP)
A program for adults who are ineligible for Montana Healthcare Programs and whose family income is within program standards. Visit https://dphhs.mt.gov/BHDD/mentalhealthservices/index.
Plan First
If a member loses Montana Healthcare Programs, family planning services may be paid by Plan First, which is a separate Montana Healthcare Programs program that covers family planning services for eligible women. Some of the services covered include office visits, contraceptive supplies, laboratory services, and testing and treatment of sexually transmitted diseases (STDs). Visit https://dphhs.mt.gov/MontanaHealthcarePrograms/PlanFirst.aspx.
End of Introduction Chapter
Provider Requirements
Provider Enrollment
To be eligible for enrollment, a provider must:
- Provide proof of licensure, certification, accreditation, or registration according to Montana state laws and regulations.
- Provide a completed W-9.
- Meet the conditions in this chapter and in program instructions regulating the specific type of provider, program, and/or service.
Providers must complete a Montana Healthcare Programs Provider Enrollment Form, which is a contract between the provider and the Department. Healthcare providers must have a National Provider Identifier (NPI) or atypical provider identifier (API), which should be used in all correspondence with Montana Healthcare Programs. Providers must enroll for each type of service they provide. For example, a pharmacy that also sells durable medical equipment (DME) must enroll for the pharmacy and again for DME.
Montana Healthcare Programs payment is made only to enrolled providers.
Enrollment Materials
Each newly enrolled provider is sent an enrollment letter confirming enrollment. The letter includes instructions for obtaining additional information from the Provider Information website.
Letters to atypical providers include their API.
Montana Healthcare Programs-related forms are available on the Provider Information website. However, providers must order CMS-1500, UB-04, and dental claim forms from an authorized vendor.
Out-of-state providers can avoid denials and late payments by renewing Montana Healthcare Programs enrollment early.
Montana Healthcare Programs Renewal
For continued Montana Healthcare Programs participation, providers must maintain a valid license or certificate. For Montana providers, licensure or certification is automatically verified and enrollment renewed each year. If licensure or certification cannot be confirmed, the provider is contacted. Out-of-state providers are notified when Montana Healthcare Programs enrollment is about to expire. To renew enrollment, providers should mail or fax a copy of their license or certificate to Provider Relations. See the Contact Us link on the Provider Information website.
Changes in Enrollment
Changes in address, telephone/fax, name, ownership, legal status, tax ID, or licensure must be submitted in writing to Provider Relations. Faxes are not accepted because the provider’s original signature and NPI (healthcare providers) or API (atypical providers) are required. For change of address, providers can use the form on the website; for a physical address change, providers must include a completed W-9 form.
To avoid payment delays, notify Provider Relations of an address change in advance.
Change of Ownership
When ownership changes, the new owner must re-enroll in Montana Healthcare Programs. For income tax reporting purposes, the provider must notify Provider Relations at least 30 days in advance about any changes to a tax identification number. Early notification helps avoid payment delays and claim denials.
Electronic Claims
Providers who submit claims electronically experience fewer errors and quicker payment. For more information on electronic claims submission options, see the Electronic Claims section in the Billing Procedures chapter in this manual.
Terminating Montana Healthcare Programs Enrollment
Montana Healthcare Programs enrollment may be terminated by writing to Provider Relations; however, some provider types have additional requirements. Providers should include their NPI (healthcare providers) or API (atypical providers) and the termination date in the letter. The Department may also terminate a provider’s enrollment under the following circumstances:
- Breaches of the provider agreement.
- Demonstrated inability to perform under the terms of the provider agreement.
- Failure to abide by applicable Montana and U.S. laws.
- Failure to abide by the regulations and policies of the U.S. Department of Health and Human Services or the Montana Healthcare Programs program.
Authorized Signature (ARM 37.85.406)
All correspondence and claim forms submitted to Montana Healthcare Programs must have an NPI (healthcare providers) or API (atypical providers) and an authorized signature. The signature may belong to the provider, billing clerk, or office personnel, and may be handwritten, typed, stamped, or computer-generated. When a signature is from someone other than the provider, that person must have written authority to bind and represent the provider for this purpose. Changes in enrollment information require the provider’s original signature.
Provider Rights
- Providers have the right to end participation in Montana Healthcare Programs in writing at any time; however, some provider types have additional requirements.
- Providers may bill Montana Healthcare Programs members when the conditions are met outlined in ARM 37.85.204.
- Providers may bill Montana Healthcare Programs members for services not covered by Montana Healthcare Programs if the provider and member have agreed in writing prior to providing services.
- When the provider does not accept the member as a Montana Healthcare Programs member, a specific custom agreement is required stating that the member agrees to be financially responsible for the services received.
- A provider may bill a member for non-covered services if the provider has informed the member in advance of providing the services that Montana Healthcare Programs will not cover the services and that the member will be required to pay privately for the services, and if the member has agreed to pay privately for the services. Non-covered services are services that may not be reimbursed for the particular member by the Montana Healthcare Programs program under any circumstances and covered services are services that may be reimbursed by the Montana Healthcare Programs program for the particular member if all applicable requirements, including medical necessity, are met (ARM 37.85.406).
- Providers have the right to choose Montana Healthcare Programs members, subject to the conditions in Accepting Montana Healthcare Programs Members later in this chapter.
- Providers have the right to request administrative reviews and fair hearings for a Department action that adversely affects the provider’s rights or the member’s eligibility (ARM 37.85.411).
Administrative Reviews and Fair Hearings (ARM 37.5.310)
A provider may request an administrative review if he/she believes the Department has made a decision that fails to comply with applicable laws, regulations, rules, or policies.
To request an administrative review, state in writing the objections to the Department’s decision and include substantiating documentation for consideration in the review. The request must be addressed to the division that issued the decision and delivered (or mailed) to the Department. The Department must receive the request within 30 days from the date the Department’s contested determination was mailed. Providers may request extensions in writing within this 30 days. See the Contact Us link on the Provider Information website.
If the provider is not satisfied with the administrative review results, a fair hearing may be requested. Fair hearing requests must contain concise reasons the provider believes the Department’s administrative review determination fails to comply with applicable laws, regulations, rules, or policies. This document must be signed and received by the Fair Hearings Office within 30 days from the date the Department mailed the administrative review determination. A copy must be delivered or mailed to the division that issued the determination within 3 working days of filing the request.
Provider Participation (ARM 37.85.401)
By enrolling in the Montana Healthcare Programs program, providers must comply with all applicable state and federal statutes, rules, and regulations, including but not limited to, federal regulations and statutes found in Title 42 of the Code of Federal Regulations and the United States Code governing the Montana Healthcare Programs program and all applicable Montana statutes and rules governing licensure and certification.
Accepting Montana Healthcare Programs Members (ARM 37.85.406)
Institutional providers, eyeglass providers, and non-emergency transportation providers may not limit the number of Montana Healthcare Programs members they will serve. Institutional providers include nursing facilities, skilled care nursing facilities, intermediate care facilities, hospitals, institutions for mental disease, inpatient psychiatric hospitals, and residential treatment facilities.
Other providers may limit the number of Montana Healthcare Programs members. They may also stop serving private-pay members who become eligible for Montana Healthcare Programs. Any such decisions must follow these principles:
- No member should be abandoned in a way that would violate professional ethics.
- Members may not be refused service because of race, color, national origin, age, or disability.
- Members enrolled in Montana Healthcare Programs must be advised in advance if they are being accepted only on a private-pay basis.
- In service settings where the member is admitted or accepted as a Montana Healthcare Programs member by a provider, facility, institution, or other entity that arranges provision of services by other or ancillary providers, all other or ancillary providers will be deemed to have accepted the individual as a Montana Healthcare Programs member and may not bill the member for the services unless, prior to provision of services, the particular provider informed the member of their refusal to accept Montana Healthcare Programs and the member agreed to pay privately for the services. See ARM 37.85.406(11)(d) for details.
- Most providers may begin Montana Healthcare Programs coverage for retroactively eligible members at the current date or from the date retroactive eligibility was effective. See the Retroactive Eligibility section in the Member Eligibility and Responsibilities chapter of this manual for details.
- When a provider bills Montana Healthcare Programs for services rendered to a member, the provider has accepted the member as a Montana Healthcare Programs member.
- Once a member has been accepted as a Montana Healthcare Programs member, the provider may not accept Montana Healthcare Programs payment for some covered services but refuse to accept Montana Healthcare Programs payment for other covered services.
Non-Discrimination (ARM 37.85.402)
Providers may not discriminate illegally in the provision of service to eligible Montana Healthcare Programs members or in employment of persons on the grounds of race, creed, religion, color, sex, national origin, political ideas, marital status, age, or disability. Providers shall comply with the Civil Rights Act of 1964 (42 USC 2000d, et seq.), the Age Discrimination Act of 1975 (42 USC 6101, et seq.), the Americans With Disabilities Act of 1990 (42 USC 12101, et seq.), section 504 of the Rehabilitation Act of 1973 (29 USC 794), and the applicable provisions of Title 49, MCA, as amended and all regulations and rules implementing the statutes.
Providers are entitled to Montana Healthcare Programs payment for diagnostic, therapeutic, rehabilitative or palliative services when the following conditions are met:
- Provider must be enrolled in Montana Healthcare Programs. (ARM 37.85.402)
- Services must be performed by practitioners licensed and operating within the scope of their practice as defined by law. (ARM 37.85.401)
- Member must be enrolled in Montana Healthcare Programs and be nonrestricted. See Member Eligibility and Responsibilities for restrictions. (ARM 37.85.415 and ARM 37.85.205)
- Service must be medically necessary. The Department may review medical necessity at any time before or after payment. (ARM 37.85.410)
- Service must be covered by Montana Healthcare Programs and not be considered cosmetic, experimental, or investigational. (ARM 37.82.102, ARM 37.85.207, and ARM 37.86.104)
- Montana Healthcare Programs and/or third party payers must be billed according to rules and instructions as described in the Billing Procedures chapter, current provider notices and manual replacement pages, and according to ARM 37.85.406 (Billing, reimbursement, claims processing and payment) and ARM 37.85.407 (third party liability).
- Charges must be usual and customary. (ARM 37.85.212 and ARM 37.85.406)
For all purposes of this rule, the amount of the provider's usual and customary charge may not exceed the reasonable charge usually and customarily charged to all payers. - ARM 37.85.406(19)
- Reimbursement to providers from Montana Healthcare Programs and all other payers may not exceed the total Montana Healthcare Programs fee. For example, if payment to the provider from all responsible parties ($75.00) is greater than the Montana Healthcare Programs fee ($70.00), Montana Healthcare Programs will pay at $0. (ARM 37.85.406)
- Claims must meet timely filing requirements. See the Billing Procedures chapter in this manual for timely filing requirements. (ARM 37.85.406)
Montana Healthcare Programs Payment Is Payment in Full (ARM 37.85.406)
Providers must accept Montana Healthcare Programs payment as payment in full for any covered service. Zero paid claims are considered paid.
Payment Return (ARM 37.85.406)
If Montana Healthcare Programs pays a claim, and then discovers that the provider was not entitled to the payment for any reason, the provider must return the payment.
Disclosure
- Providers are required to fully disclose ownership and control information when requested by the Department. (ARM 37.85.402)
- Providers are required to make all medical records available to the Department. (ARM 37.85.410 and ARM 37.85.414)
Member Services
- All services must be made a part of the medical record. (ARM 37.85.414)
- Providers must treat Montana Healthcare Programs members and private-pay members equally in terms of scope, quality, duration, and method of delivery of services unless specifically limited by regulations. (ARM 37.85.402)
Confidentiality (ARM 37.85.414)
All Montana Healthcare Programs member and applicant information and related medical records are confidential. Providers are responsible for maintaining confidentiality of healthcare information subject to applicable laws.
Record Keeping (ARM 37.85.414)
Providers must maintain all Montana Healthcare Programs-related medical and financial records for 6 years and 3 months following the date of service. The provider must furnish these records to the Department or its designee upon request. The Department or its designee may audit any Montana Healthcare Programs-related records and services at any time. Such records may include but are not limited to:
- Original prescriptions
- Certification of medical necessity
- Treatment plans
- Medical records and service reports including but not limited to:
- Member’s name and date of birth
- Date and time of service
- Name/title of person providing service (other than billing practitioner)
- Chief complaint or reason for each visit
- Pertinent medical history
- Pertinent findings on examination
- Medication, equipment, and/or supplies prescribed or provided
- Description and length of treatment
- Recommendations for additional treatments, procedures, or consultations
- X-rays, tests, and results
- Dental photographs/teeth models
- Plan of treatment and/or care, and outcome
- Specific claims and payments received for services
- Each medical record entry must be signed and dated by the person ordering or providing the service.
- Prior authorization information
- Claims, billings, and records of Montana Healthcare Programs payments and amounts received from other payers for services provided to Montana Healthcare Programs members
- Records/original invoices for items prescribed, ordered, or furnished
- Any other related medical or financial data
Compliance with Applicable Laws, Regulations, and Policies
All providers must follow all applicable rules of the Department and all applicable state and federal laws, regulations, and policies. Provider manuals are to assist providers in billing Montana Healthcare Programs; they do not contain all Montana Healthcare Programs rules and regulations. Rule citations in the text are a reference tool; they are not a summary of the entire rule. In the event that a manual conflicts with a rule, the rule prevails.
The following are references for some of the rules that apply to Montana Healthcare Programs. The provider manual for each individual program contains rule references specific to that program.
- Title XIX Social Security Act 1901 et seq.
- 42 U.S.C. 1396 et seq.
- Code of Federal Regulations (CFR)
- CFR Title 42 – Public Health
- Montana Codes Annotated (MCA)
- MCA Title 53 – Social Services and Institutions
- Administrative Rules of Montana (ARM)
- ARM Title 37 – Public Health and Human Services
Links to rules are available on the provider type pages of the Provider Information website. Paper copies of rules are available through the Secretary of State’s office.
Provider Sanctions (ARM 37.85.501–507 and ARM 37.85.513)
The Department may withhold a provider’s payment or suspend or terminate Montana Healthcare Programs enrollment if the provider has failed to abide by terms of the Montana Healthcare Programs contract, federal and state laws, regulations, and policies.
Providers are responsible for keeping informed about applicable laws, regulations, and policies.
Other Programs
Below is a list of non-Montana Healthcare Programs Department of Public Health and Human Services (DPHHS) programs.
- Chemical Dependency Bureau Substance Dependency/Abuse Treatment https://dphhs.mt.gov/BHDD/SubstanceAbuse/index
- Children’s Mental Health Bureau Non-Montana Healthcare Programs Services https://dphhs.mt.gov/dsd/https://dphhs.mt.gov/BHDD/cmb/Manuals/Manuals
- Health Insurance Premium Payment (HIPP) https://dphhs.mt.gov/MontanaHealthcarePrograms/HIPP
- Healthy Montana Kids (HMK) https://dphhs.mt.gov/HMK
- Mental Health Services Plan (MHSP) https://dphhs.mt.gov/BHDD/mentalhealthservices/index
- Plan First https://dphhs.mt.gov/MontanaHealthcarePrograms/PlanFirst
End of Provider Requirements Chapter
EPSDT Well-Child
The Early and Periodic Screening, Diagnostic, and Treatment (EPSDT) Services program is the federally sponsored, comprehensive healthcare benefits package for Montana Healthcare Programs-enrolled children through age 20. It helps families get early identification and treatment of medical, dental, vision, mental health, and developmental problems for their children. All Montana Healthcare Programs families are encouraged to use these services. See ARM 37.86.2201–2235.
EPSDT Well-Child Check-Ups
At the core of EPSDT is the well child visit. These regularly scheduled check-ups help your child’s primary care provider identify problems and assist with a treatment plan for your child. . By following the Bright Futures schedule of well child visits, parents can ensure their children receive the full benefit of their comprehensive health care coverage.
EPSDT Well-Child visits include:
- Comprehensive health & developmental history
- Comprehensive unclothed physical examination
- Assessment of physical, emotional & developmental health
- Immunizations appropriate to age & health history
- Laboratory tests (including blood lead levels)
- Assessment of mental/behavioral health
- Assessment of mouth, oral cavity & teeth, including referral to a dentist
- Assessment of nutritional status
- Assessment of vision, including referrals
- Assessment of overall health, including referrals
- Health education (also called anticipatory guidance)
- Family planning services and adolescent maternity care
In addition to well child visits, EPSDT includes inter-periodic sick visits, or other visits as needed by the individual child.
EPSDT Provider Resources:
Immunization Schedule - The American Academy of Pediatrics Bright Futures recommended immunization schedule for children through the age of 18.
Montana Healthcare Programs Member Guide - Learn more about Montana Healthcare Programs coverage through the Early and Periodic Screening, Diagnosis and Treatment Program at pages 30-31 in the handbook.
Bright Futures - A link to the American Academy of Pediatrics Bright Futures website.
Additional Services Under EPSDT
If a child (up to the age of 21), needs medically necessary services, outside the normal realm of covered services (non-covered, over the limit, does not meet criteria, etc), these can be approved on a case by case basis. EPSDT prior authorization requests must be submitted by a child’s primary care provider or medical specialist, within their scope of practice, who determines the child needs additional treatment, services, or supplies for a primary health condition.
These requests are reviewed and decision determinations completed within 2 weeks of receipt of all required documentation.
EPSDT Prior Authorization & Medical Necessity Form is found on the Forms Page of the provider website.
For more information regarding EPSDT services contact the DPHHS Health Resources Division, Maternal and Child Health Nurse .
Who Can Provide EPSDT Screenings?
- Physicians
- Advanced Registered Nurse Practitioners (ARNP)
- Physician assistants
- Registered nurse under guidance of a physician or ARNP may perform the screenings but not diagnose or treat.
- Providers must be Montana Healthcare Programs-enrolled to receive payment from Montana Healthcare Programs.
The Well-Child Screen
The foundation of EPSDT is the well-child screen. These screens should begin as early as possible in a child’s life or as soon as the child is enrolled in Montana Healthcare Programs. The well-child screens are based on a periodicity schedule established by medical, dental, and other healthcare experts, including the American Academy of Pediatrics. The Well-Child Screen Recommendations are found on the Bright Futures website, https:/brightfutures.aap.org.
Every infant should have a newborn evaluation after birth. If a child comes under care for the first time at any point on the schedule, or if any items are not accomplished at the suggested age, the schedule should be brought up-to-date at the earliest possible time. If a well-child screen shows that a child is at risk based on the child’s environment, history, or test results, the provider should perform required or recommended tests even though they may not be indicated for the child’s age. Developmental, psychosocial, and chronic disease issues for children and adolescents may require frequent counseling and treatment visits separate from preventive care visits.
Using an evidence-based screening tool, a caregiver depression screening is covered under an enrolled child's Montana Healthcare Programs benefit, during their first year of life. This includes anyone that is considered a child's primary care provider. Positive screenings must be appropriately referred. Screenings are covered under the child’s Montana Healthcare Programs benefit due to the dyadic relationship of a caregiver and child. The service is directed at treating the health and well-being of the child, with a goal of providing a healthy start to their life.
Initial/Interval History
A comprehensive history, obtained from the parent or other responsible adult who is familiar with the child’s history should be done during the initial visit. Once it is done, it only needs to be updated at subsequent visits. The history should include the following:
- Developmental history to determine whether the child’s individual developmental processes fall within a normal range of achievement compared to other children of his/her age and cultural background.
- Discussion of the child’s development, as well as techniques to enhance the child’s development, with the parents.
- Nutritional history and status. Questions about dietary practices identify unusual eating habits, such as pica, or extended use of bottle feedings, or diets that are deficient or excessive in one or more nutrients.
- Complete dental history.
Developmental Assessments
Appropriate Developmental Surveillance. Providers should administer an age-appropriate developmental screen at each well-child visit. Any concerns raised during the surveillance should be promptly addressed with standardized developmental screening tests. See the recommended algorithm provided by Bright Futures at http://pediatrics.aappublications.org/content/118/1/405.full.
Appropriate Developmental Screening. Providers should administer an age appropriate developmental screen at age 9, 18, and 30 months. Results should be considered in combination with other information gained through the history, physical examination, observation, and reports of behavior. If developmental problems are identified, appropriate follow-up and/or referral to proper resources should be made.
Speech and language screens identify delays in development. The most important readiness period for speech is 9 to 24 months. Parents should be urged to talk to their children early and frequently. Refer the child for speech and language evaluation as indicated.
Parents of children with developmental disabilities should be encouraged to contact Parents Let’s Unite for Kids (PLUK).
PLUK is an organization designed to provide support, training, and assistance to children with disabilities and their parents. Call, write, or visit the PLUK website, http://www. pluk.org/.
PLUK
516 North 32nd Street
Billings, MT 59101-6003
(406) 255-0540 Phone
(800) 222-7585 Toll Free
(406) 255-0523 Fax
E-Mail info@pluk.org
Depression Screening. Signs and symptoms of emotional disturbances represent deviations from or limitations in healthy development. These problems usually will not warrant a psychiatric referral but can be handled by the provider. He/she should discuss problems with parents and give advice. If a psychiatric referral is warranted, the provider should refer the child to an appropriate provider. Recommended screening using the Member Health Questionnaire (PHQ-2) or other tools found on the Bright Futures website.
Alcohol and Drug Use Screen. The provider should screen for risky behaviors (e.g., substance abuse, unprotected sexual activity, tobacco use, firearm possession). In most instances, indications of such behavior will not warrant a referral but can be handled by the provider, who should discuss the problems with the member and the parents and give advice. If a referral is warranted, the provider should refer to an appropriate provider. Recommended screening tool can be found on the Bright Futures website.
Nutritional Screen
Providers should assess the nutritional status at each well-child screen. Children with nutritional problems may be referred to a licensed nutritionist or dietician for further assessment or counseling.
Unclothed Physical Inspection
At each visit, a complete physical examination is essential. Infants should be totally unclothed and older children undressed and suitably draped.
Vision Screen
A vision screen appropriate to the age of the child should be conducted at each well-child screen. If the child is uncooperative, rescreen within six months.
Hearing Screen
A hearing screen appropriate to the age of the child should be conducted at each well-child screen. All newborns should be screened.
Autism Screen
Autism screenings are recommended at age 18 and 24 months, and a recommended tool is provided on the Bright Futures website.
Critical Congenital Heart Defect Screen
Screening using pulse oximetry should be performed in newborns, after 24 hours old and before discharge.
Laboratory Tests
Providers who conduct well-child screens must use their medical judgment in determining applicability of performing specific laboratory tests. Appropriate tests should be performed on children determined at risk through screening and assessment.
Hematocrit and Hemoglobin. Hematocrit or hemoglobin tests should be done for at-risk (premature and low birth weight) infants at ages newborn and 2 months. For children who are not at risk, follow the recommended schedule.
Blood Lead Level. All children in Montana Healthcare Programs are at risk of lead poisoning. To ensure their good health, the federal government requires that all Montana Healthcare Programs-enrolled children be tested for lead poisoning. Testing is recommended at 12 and 24 months of age. Children up to age 6 years who have not been checked for lead poisoning before should also be tested.
A blood lead level test should be performed on all children at 12 and 24 months of age.
All Montana Healthcare Programs children at other ages should be screened. Complete a verbal risk assessment for all Montana Healthcare Programs children up to age 6 years at each EPSDT screening:
- Does your child live in Butte, Walkerville, or East Helena, which are designated high-risk areas?
- Does your child live near a lead smelter, battery recycling plant, or other industry (operating or closed) likely to release lead?
- Does your child live in or regularly visit a house built before 1960, which contains lead paint?
- Does your child live near a heavily traveled major highway where soil and dust may be contaminated with lead?
- Does your child live in a home where the plumbing consists of lead pipes or copper with lead solder joints?
- Does your child frequently come in contact with an adult who works with lead, such as construction, welding, pottery, reloading ammunition (making own bullets), etc.?
- Is the child given any home or folk remedies? If yes, discuss.
If the answer to all questions is no, a child is considered at low risk for high doses of lead exposure. Children at low risk for lead exposure should receive a blood test at 12 and 24 months.
If the answer to any question is yes, a child is considered at high risk for high doses of lead exposure and a blood lead level test must be obtained immediately regardless of the child’s age.
Tuberculin Screening. Tuberculin testing should be done on individuals in high-risk populations or if historical findings, physical examination, or other risk factors so indicate.
Dyslipidemia Screening. Screening should be considered based on risk factors and family history at 24 months, 4, 6, 8, 12, 13, 14, 15, 16, and 17 years, and is indicated at or around 10 and 20 years of age.
STI/HIV Screening. All adolescent members should be screened for sexually transmitted infections (STIs) and HIV based on risk assessment starting at age 11 and reassessed annually with at least one assessment occurring between the ages of 16–18 years old.
Cervical Dysplasia Screening. Adolescents are not routinely screened for cervical dysplasia until age 21. See the 2010 AAP statement for indications at https:/www.aap.org/en-us/Pages/Default.aspx.
Immunizations
The immunization status of each child should be reviewed at each well-child screen. This includes interviewing parents or caretakers, reviewing immunization records, and reviewing risk factors.
The Recommended Childhood Immunization schedule is available on the AMA website and the Centers for Disease Control and Prevention website.
Dental Screen
The child’s provider should perform annual dental screens, and results should be included in the child’s initial/interval history. Annual dental screens include an oral inspection, fluoride varnish (as available) and making a referral to a dentist for any of the following reasons:
- When the first tooth erupts, and every six months thereafter.
- If a child with a first tooth has not obtained a complete dental examination by a dentist in the past 12 months.
- If an oral inspection reveals cavities or infection, or if the child is developing a handicapping malocclusion or significant abnormality.
Discussion and Counseling/Anticipatory Guidance
Providers should discuss examination results, address assessed risks, and answer any questions in accordance with parents’ level of understanding. Age-appropriate discussion and counseling should be an integral part of each visit. Allow sufficient time for unhurried discussions.
At each screening visit, provide age-appropriate anticipatory guidance concerning such topics as the following:
- Auto safety: Car seats, seat belts, air bags, positioning young or lightweight children in the backseat.
- Recreational safety: Helmets and protective padding, playground equipment.
- Home hazards: Poisons, accidents, weapons, matches/lighters, staying at home alone, use of detectors for smoke, radon gas, and carbon monoxide.
- Exposure to sun and secondhand smoke.
- Adequate sleep, exercise, and nutrition, including eating habits and eating disorders.
- Peer pressure.
- General health: Immunizations, patterns of respiratory infections, skin eruptions, care of teeth.
- Problems such as whining, stealing, setting fires, etc. as indicated by parental concern.
- Behavior and development: Sleep patterns, temper, attempts at independence (normal and unpleasant behavior), curiosity, speech and language, sex education and development, sexual activities, attention span, toilet training, alcohol and tobacco use, substance abuse.
- Interpersonal relations: Attitude of father; attitude of mother; place of child in family; jealousy; selfishness, sharing, taking turns; fear of strangers; discipline, obedience; manners, courtesy; peer companionship/relations; attention getting; preschool, kindergarten and school readiness and performance; use of money; assumption of responsibility; need for affection and praise; competitive athletics.
End of EPSDT Well-Child Chapter
Prior Authorization
What Is Prior Authorization?
Prior authorization refers to a list of services that require Department authorization before they are performed. Some services may require both Passport referral and prior authorization.
Montana Healthcare Programs does not pay for services when prior authorization, Passport, or Team Care requirements are not met.
In practice, providers will often encounter members who are enrolled in Passport. Whether the member is enrolled in Passport or Team Care, the eligibility information denotes the member’s primary care provider. Services are only covered when they are provided or approved by the designated Passport provider or Team Care pharmacy shown in the eligibility information.
If a service requires prior authorization, the requirement exists for all Montana Healthcare Programs members. Prior authorization is usually obtained through the Department or a prior authorization contractor.
When both Passport and prior authorization are required, they must be recorded in different places on the claim.
If both Passport referral and prior authorization are required for a service, then both numbers must be recorded in different fields on the Montana Healthcare Programs claim form. (See the Submitting a Claim section in this manual.)
Most Montana Healthcare Programs fee schedules indicate when prior authorization is required for a service. For more information, see your provider type fee schedule and/or the Prior Authorization page of the Provider Information website.
End of Prior Authorization Chapter
Telemedicine
Program Overview
Telemedicine is the use of interactive audio-video equipment to link practitioners and members located at different sites. The Montana Healthcare Programs Program reimburses providers for medically necessary telemedicine services furnished to eligible members.
Telemedicine is not itself a unique service but a means of providing selected services approved by Montana Healthcare Programs. Telemedicine involves two collaborating providers, an originating provider and a distance provider. The provider where the member is located is the originating provider or originating site. In most cases, the distant provider is a clinician who acts as a consultant to the originating provider. However, in some cases the distant provider may be the only provider involved in the service.
Providers must be enrolled as Montana Healthcare Programs providers and be licensed in the State of Montana in order to:
- Treat a Montana Healthcare Programs member; and
- Submit claims for payment to Montana Healthcare Programs
When to Use Telemedicine
Montana Healthcare Programs considers the primary purposes of telemedicine are to bring providers to people living in rural areas, and to allow members access to care that is not available within their community. Providers should weigh these advantages against quality of care and member safety considerations. Members may choose which is more convenient for them when providers make telemedicine available.
Telemedicine should not be selected when face-to-face services are medically necessary. Members should establish relationships with primary care providers who are available on a face-to-face basis.
Telemedicine can be provided in member’s residence; the distance provider is responsible for the confidentiality requirements. Member’s residences do not qualify for originating provider reimbursement.
Telemedicine Confidentiality Requirements
All Montana Healthcare Programs providers using telemedicine to deliver Montana Healthcare Programs services must employ existing quality-of-care protocols and member confidentiality guidelines when providing telemedicine services. Health benefits provided through telemedicine must meet the same standard of care as in-person care. Record keeping should comply with Montana Healthcare Programs requirements in Administrative Rules of Montana (ARM) 37.85.414.
Transmissions must be performed on dedicated secure lines or must utilize an acceptable method of encryption adequate to protect the confidentiality and integrity of the transmission. Transmissions must employ acceptable authentication and identification procedures by both the sender and receiver.
General Billing Instructions
Providers may only bill procedure codes for which they are already eligible to bill. Services not otherwise covered by Montana Healthcare Programs are not covered when delivered via telemedicine. The use of telecommunication equipment does not change prior authorization or any other Montana Healthcare Programs requirements established for the services being provided.
The availability of services through telemedicine in no way alters the scope of practice of any health care provider; or authorizes the delivery of health care services in a setting or manner not otherwise authorized by law.
Telemedicine reimbursement does not include:
- Consultations provided by telephone (interactive audio); or
- Facsimile machine transmissions.
- Crisis hotlines
The originating and distant providers may not be within the same facility or community. The same provider may not be the pay to for both the originating and distance provider.
If a rendering provider’s number is required on the claim for a face-to-face visit, it is required on a telemedicine claim.
Originating Provider Requirements
The originating site provider must have secure and appropriate equipment to ensure confidentiality, including camera(s), lighting, transmission and other needed electronics.
Originating providers bill using procedure code Q3014 (telemedicine originating site fee) for the use of a room and telecommunication equipment. The telehealth place of service code 02 does not apply to originating site facilities billing a facility fee.
The following provider types may bill procedure code Q3014:
- Outpatient Hospital;
- Critical Access Hospital*;
- Federally Qualified Health Center*;
- Rural Health Center*;
- Indian Health Service*;
- Physician;
- Psychiatrist;
- Mid-Levels;
- Dieticians;
- Psychologists;
- Licensed Clinical Social Worker;
- Licensed Professional Counselor;
- Mental Health Center:
- Chemical Dependency Clinic;
- Group/Clinic;
- Public Health Clinic; or
- Family Planning Clinic.
*Reimbursement for Q3014 is a set fee and is paid outside of both the cost to charge ratio and the all-inclusive rate.
Originating provider claims must include a specific diagnosis code to indicate why a member is being seen by the distance provider. The originating site must request the diagnosis code(s) from the distance site prior to billing the telemedicine appointment.
The originating provider may also, as appropriate; bill for clinical services provided on-site the same day that a telemedicine originating site service is provided. This originating site may not bill for assisting the distant provider with an examination, this includes any services that would be normally included in a face-to-face visit.
Distance Provider Requirements
Distance providers should submit claims for telehealth services using the appropriate CPT or HCPCS code for the professional service along with the GT modifier (interactive communication). Effective January 1, 2017, providers must also use the telehealth place of service of 02 for claims submitted on a CMS-1500 claim. By coding with the GT modifier and the 02 place of service, the provider is certifying that the service was a face-to-face visit provided via interactive audio-video telemedicine.
Any out of state distance providers must be licensed in the State of Montana and enrolled in Montana Healthcare Programs in order to provide telemedicine services to Montana Healthcare Programs members. Providers must contact the Montana Department of Labor and Industry to find out details on licensing requirements for their applicable professional licensure.
End of Telemedicine Chapter
Member Eligibility and Responsibilities
Montana Healthcare Programs ID Cards
Each Montana Healthcare Programs member is issued his/her own permanent Montana Access to Health Montana Healthcare Programs ID card (including QMB only members), Healthy Montana Kids Plus (HMK Plus) card.
Members must never throw away the card, even if their Montana Healthcare Programs eligibility ends.
The ID card lists the member’s name, member number, and date of birth. The member number may be used for checking eligibility and for billing Montana Healthcare Programs.
Since eligibility information is not on the card, providers must verify eligibility before providing services. See the Verifying Member Eligibility section below.
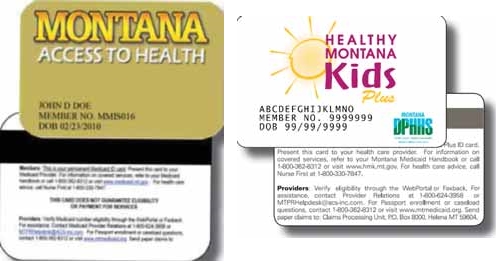
Providers should verify eligibility before providing services.
Verifying Member Eligibility
Member eligibility may change monthly. Providers should verify eligibility at each visit using any of the methods described in the following table.
The list below shows information returned to the provider in response to an eligibility inquiry:
- Member’s Montana Healthcare Programs ID number. Used when billing Montana Healthcare Programs.
- Eligibility Status. Montana Healthcare Programs eligibility status for the requested dates:
- Standard Montana Healthcare Programs. Member is eligible for all Montana Healthcare Programs covered services.
- QMB. Member is a qualified Medicare beneficiary. See the section titled When a Member Has Other Coverage in this chapter.
- Team Care. TC indicator means member is enrolled in the Team Care program. All services must be provided or approved by the designated Passport provider.
- Designated Provider. The member’s primary care provider’s name and phone number are shown for members who are enrolled in Passport to Health or Team Care. In either case, all services must be provided or approved by the designated provider. See the Passport to Health provider manual.
- TPL. If the member has other insurance coverage (TPL), the name of the other insurance carrier is shown.
- Medicare ID Number. A Medicare identification number for members who are eligible for both Montana Healthcare Programs and Medicare.
Member without Card
Since eligibility information is not on the card, it is necessary for providers to verify eligibility before providing services whether or not the member presents a card. Confirm eligibility using one of the methods shown in the Verifying Member Eligibility table. If eligibility is not available, the provider may contact the member’s local Office of Public Assistance (OPA).
Newborns
Care rendered to newborns can be billed under the newborn’s original Montana Healthcare Programs ID number assigned by the mother’s local OPA until a permanent ID number becomes available. The hospital or the parents may apply for the child’s Social Security number. Parents are responsible for notifying their local OPA when they have received the child’s new Social Security number.
Inmates in Public Institutions (ARM 37.82.1321)
Montana Healthcare Programs does not cover members who are inmates in a public institution.
Presumptive Eligibility
Presumptive eligibility is available to hospitals and their affiliated facilities that participate with Montana Healthcare Programs.
Personnel must be trained and certified to make presumptive eligibility determinations for short-term, temporary coverage for the following coverage groups:
- Adults between the ages of 18 and 26 who were in Foster Care and receiving Montana Healthcare Programs at age 18
- Healthy Montana Kids Plus
- Healthy Montana Kids
- Parent/Caretaker Relative Montana Healthcare Programs
- Pregnant women (ambulatory prenatal care)
- Women between the ages of 19 and 64 who have been screened and diagnosed with breast or cervical cancer.
To encourage prenatal care, uninsured pregnant women may receive presumptive eligibility for Montana Healthcare Programs.
Presumptive eligibility may be for only part of a month and does not cover inpatient hospital services, but does include other applicable Montana Healthcare Programs services.
Retroactive Eligibility
When a member is determined retroactively eligible for Montana Healthcare Programs, the member should give the provider a Notice of Retroactive Eligibility (160-M). The provider has 12 months from the date retroactive eligibility was determined to bill for those services.
Retroactive Montana Healthcare Programs eligibility does not allow a provider to bypass prior authorization requirements. See specific provider manuals for requirements.
When a member becomes retroactively eligible for Montana Healthcare Programs, the provider may:
- Accept the member as a Montana Healthcare Programs member from the current date.
- Accept the member as a Montana Healthcare Programs member from the date retroactive eligibility was effective.
- Require the member to continue as a private-pay member.
Institutional providers (nursing facilities, skilled care nursing facilities, intermediate care facilities for the mentally retarded, institutions for mental disease, inpatient psychiatric hospitals, and residential treatment facilities) must accept retroactively eligible member from the date eligibility was effective. Non-emergency transportation and eyeglass providers cannot accept retroactive eligibility. For more information on billing Montana Healthcare Programs for retroactive eligibility services, see the Billing Procedures chapter in this manual.
Coverage for the Medically Needy
This coverage is for members who have an income level that is higher than the SSI-eligible Montana Healthcare Programs program standards. However, when a member has high medical expenses relative to income he/she can become eligible for Montana Healthcare Programs by incurring medical expenses and/or making a cash payment equal to the spend down amount on a monthly basis. The spend down amount is based on the member's countable income. When the member chooses to use the Medical Expense option to meet their spend down, he/she is responsible to pay for medical services before Montana Healthcare Programs eligibility begins and Montana Healthcare Programs pays for remaining covered services.
Providers should verify if medically needy members are covered by Montana Healthcare Programs on the date of service to determine whether to bill the member or Montana Healthcare Programs.
Because eligibility does not cover an entire month, when the medical expense option is used the member’s eligibility information may show eligibility for only part of the month and the provider may receive a One Day Authorization Notice. The One Day Authorization Notice , sent by the local OPA, states the date eligibility began and the portion of the bill the member must pay. If the provider has not received a One Day Authorization Notice , he/she should verify eligibility for the date of service by any method described in this chapter or by contacting the member’s local OPA. Since this eligibility may be determined retroactively, the provider may receive the One Day Authorization Notice weeks or months after services have been provided.
Members may choose the cash option process where they can pay a monthly premium to Montana Healthcare Programs equal to the spend down amount, instead of making payments to providers, and have Montana Healthcare Programs coverage for the entire month. This method results in quicker payment, simplifies the eligibility process, and eliminates spend down notices. Providers may encourage but not require members to use the cash option.
It is important to note that after a member submits their payment to Montana Healthcare Programs, the Department requires time to process the payment. Once the payment is processed, the system will provide the Montana Healthcare Programs coverage. The member may choose to submit their payment to Montana Healthcare Programs after medical services have been provided. In that situation, the member's Montana Healthcare Programs eligibility information will not be available at the time the service is provided and any claims submitted at that time will be denied. Once the spend down has been paid and processed, active eligibility will display and claims can be submitted.
Nurse First
Nurse First programs provide disease management and nurse triage services for Montana Healthcare Programs members throughout the state.
Nurse First Advice Line, 1-800-330-7847. A toll-free, confidential telephone number members may call 24/7/365 for advice from a registered nurse about injuries, diseases, healthcare, or medications. The nurses do not diagnose or provide treatment. Most Montana Healthcare Programs members are eligible to use the Nurse First Advice Line,The program is voluntary though participation is strongly encouraged.
Montana Breast and Cervical Cancer Treatment Program
This program provides Standard Montana Healthcare Programs coverage for women who have been screened through the Montana Breast and Cervical Health Program (MBCHP) and diagnosed with breast and/or cervical cancer or a pre-cancerous condition. All other policies and procedures in this chapter apply. For information regarding screening through the MBCHP program, call 1-888-803-9343.
When a Member Has Other Coverage
Montana Healthcare Programs members often have coverage through Medicare, workers’ compensation, employment-based coverage, individually purchased coverage, etc. Coordination of benefits is the process of determining which source of coverage is the primary payer in a particular situation. In general, providers should bill other carriers before billing Montana Healthcare Programs, but there are some exceptions. (See the section titled Exceptions to Billing Third Party First in this chapter.) Medicare is processed differently than other sources of coverage.
Identifying Additional Coverage
The member’s Montana Healthcare Programs eligibility verification may identify other payers such as Medicare or other third party payers. If a member has Medicare, the Medicare ID number is provided. If a member has additional coverage, the carrier is shown. Some examples of third party payers include:
- Private health insurance
- Employment-related health insurance
- Workers’ compensation insurance*
- Health insurance from an absent parent
- Automobile insurance*
- Court judgments and settlements*
- Long-term care insurance
*These third party payers (and others) may not be listed on the member’s eligibility verification.
Providers should use the same procedures for locating third party sources for Montana Healthcare Programs members as for their non-Montana Healthcare Programs members. Providers cannot refuse service because of a third party payer or potential third party payer.
When a Member Has Medicare
Medicare claims are processed and paid differently than other non-Montana Healthcare Programs claims. The other sources of coverage are called third party liability or TPL, but Medicare is not.
Medicare Part A Claims
Medicare Part A carriers and Montana Healthcare Programs use electronic exchange of institutional claims covering Part A services. Providers must submit these claims first to Medicare. After Medicare processes the claim, an Explanation of Medicare Benefits (EOMB) is sent to the provider. The provider then reviews the EOMB and submits the claim to Montana Healthcare Programs.
Medicare Part B Crossover Claims
The Department has an agreement with the Medicare Part B carrier for Montana (Noridian) and the Durable Medical Equipment Regional Carrier (DMERC) under which the carriers provide the Department with claims for members who have both Medicare and Montana Healthcare Programs coverage. Providers must tell Medicare that they want their claims sent to Montana Healthcare Programs automatically, and must have their Medicare provider number on file with Montana Healthcare Programs.
When members have both Medicare and Montana Healthcare Programs covered claims, and have made arrangements with both Medicare and Montana Healthcare Programs, Part B services need not be submitted to Montana Healthcare Programs. When a crossover claim is submitted only to Medicare, Medicare will process the claim, submit it to Montana Healthcare Programs, and send the provider an explanation of Medicare benefits (EOMB). Providers must check the EOMB for the statement indicating that the claim has been referred to Montana Healthcare Programs for further processing. It is the provider’s responsibility to follow up on crossover claims and make sure they are correctly billed to Montana Healthcare Programs within the timely filing limit. (See the Billing Procedures chapter in this manual.)
Providers should submit Medicare crossover claims to Montana Healthcare Programs only when:
- The referral to Montana Healthcare Programs statement is missing. In this case, submit a claim and a copy of the Medicare EOMB to Montana Healthcare Programs for processing.
- The referral to Montana Healthcare Programs statement is present, but there is no response from Montana Healthcare Programs within 45 days of receiving the Medicare EOMB. Submit a claim and a copy of the Medicare EOMB to Montana Healthcare Programs for processing.
- Medicare denies the claim. The provider may submit the claim to Montana Healthcare Programs with the EOMB and denial explanation (as long as the claim has not automatically crossed over from Medicare).
When submitting electronic claims with paper attachments, see the Billing Electronically with Paper Attachments section of the Billing Procedures chapter.
When submitting a claim with the Medicare EOMB, use Montana Healthcare Programs billing instructions and codes. Medicare’s instructions, codes, and modifiers may not be the same as Montana Healthcare Programs’s. The claim must also include the Montana Healthcare Programs provider number and Montana Healthcare Programs member ID number. It is the provider’s responsibility to follow up on crossover claims and make sure they are correctly billed to Montana Healthcare Programs within the timely filing limit.
When a Member Has TPL (ARM 37.85.407)
When a Montana Healthcare Programs member has additional medical coverage (other than Medicare) it is often referred to as third party liability or TPL. In most cases, providers must bill other insurance carriers before billing Montana Healthcare Programs.
Providers are required to notify their members that any funds the member receives from third party payers (when the services were billed to Montana Healthcare Programs) must be turned over to the Department. These words printed on the member’s statement fulfill this obligation: When services are covered by Montana Healthcare Programs and another source, any payment the member receives from the other source must be turned over to Montana Healthcare Programs.
Exceptions to Billing Third Party First
In a few cases, providers may bill Montana Healthcare Programs first:
- When a Montana Healthcare Programs member is also covered by Indian Health Service (IHS) or the Crime Victim Compensation Program, providers must bill Montana Healthcare Programs first. These are not considered a third party liability.
- When a member has Montana Healthcare Programs eligibility and MHSP eligibility for the same month, Montana Healthcare Programs must be billed first.
- ICD prenatal and ICD preventive pediatric diagnosis conditions may be billed to Montana Healthcare Programs first. In these cases, Montana Healthcare Programs will “pay and chase” or recover payment itself from the third party payer.
- The following services may also be billed to Montana Healthcare Programs first:
- Nursing facility (as billed on nursing home claims)
- Audiology
- Eyeglasses
- Hearing aids and batteries
- Home and community-based services (waiver)
- Optometry
- Oxygen in a nursing facility
- Personal assistance/Community First Choice
- Transportation (other than ambulance)
- If the third party has only potential liability, the provider may bill Montana Healthcare Programs first. Do not indicate the potential third party on the claim. Instead, notify the Department by sending the claim and notification to Third Party Liability, P.O. Box 5838, Helena, MT 59604.
Requesting an Exemption
Providers may request to bill Montana Healthcare Programs first under certain circumstances. In each of these cases, the claim and required information should be sent directly to the Third Party Liability unit.
- When a provider is unable to obtain a valid assignment of benefits, the provider should submit the claim with documentation that he/she attempted to obtain assignment and certification that the attempt was unsuccessful.
- When the provider has billed the third party insurance and has received a non-specific denial (e.g., no member name, date of service, amount billed), submit the claim with a copy of the denial and a letter of explanation.
- When the Child Support Enforcement Division has required an absent parent to have insurance on a child, the claim can be submitted to Montana Healthcare Programs then the following requirements are met:
- The third party carrier has been billed, and 30 days or more have passed since the date of service.
- The claim is accompanied by a certification that the claim was billed to the third party carrier, and payment or denial has not been received.
- If another insurance has been billed, and 90 days have passed with no response, submit the claim with a note explaining that the insurance company has been billed (or a copy of the letter sent to the insurance company). Include the date the claim was submitted to the insurance company and certification that there has been no response.
When the Third Party Pays or Denies a Service
When a third party payer is involved (excluding Medicare) and the other payer:
- Pays the claim, indicate the amount paid when submitting the claim to Montana Healthcare Programs for processing.
- Allows the claim, and the allowed amount went toward the member’s deductible, include the insurance explanation of benefits (EOB) when billing Montana Healthcare Programs.
- Denies the claim, submit the claim and a copy of the denial (including the reason explanation) to Montana Healthcare Programs.
- Denies a line on the claim, bill the denied line on a separate claim and submit to Montana Healthcare Programs. Include the EOB from the other payer and an explanation of the reason for denial (e.g., definition of denial codes).
When the Third Party Does Not Respond
If another insurance has been billed, and 90 days have passed with no response, bill Montana Healthcare Programs as follows:
- Submit the claim and a note explaining that the insurance company has been billed, or submit a copy of the letter sent to the insurance company.
- Include the date the claim was submitted to the insurance company.
- Send this information to the Third Party Liability Unit.
Coordination Between Medicare and Montana Healthcare Programs
Coordination of benefits between Medicare and Montana Healthcare Programs is generally accomplished through electronic crossover of claims. It is important to always bill Medicare prior to Montana Healthcare Programs for healthcare services. After Medicare processes the claim, it will automatically cross over to Montana Healthcare Programs. If a claim does not cross automatically to Montana Healthcare Programs from Medicare, the provider should not submit the claim to Montana Healthcare Programs until Medicare has processed. Montana Healthcare Programs payment is subsequent to Medicare and will only pay up to the Montana Healthcare Programs fee after considering the payment from Medicare. See the How Payment Is Calculated chapter in the provider type manuals to learn how Montana Healthcare Programs payments are calculated.
- Qualified Medicare Beneficiary (QMB). For QMBs, Montana Healthcare Programs pays their Medicare A and B premiums and some or all of the Medicare coinsurance and deductibles (up to the Montana Healthcare Programs fee). QMB members may or may not also be eligible for Montana Healthcare Programs benefits.
- QMB Only. Montana Healthcare Programs will make payments only toward the Medicare coinsurance and deductible.
- QMB and Montana Healthcare Programs. Covered services include the same services as for Montana Healthcare Programs only members. If a service is covered by Medicare but not by Montana Healthcare Programs, Montana Healthcare Programs will pay all or part of the Medicare coinsurance and deductible. If a service is covered by Montana Healthcare Programs but not by Medicare, then Montana Healthcare Programs will be the primary payer for that service.
- Specified Low-Income Medicare Beneficiary (SLMB). Montana Healthcare Programs pays the Medicare Part B premium only.
- SLMB Only. Members do not receive Montana Healthcare Programs cards, are not eligible for other Montana Healthcare Programs benefits, and must pay their own Medicare coinsurance and deductibles.
- SLMB and Montana Healthcare Programs. For services Medicare covers, Montana Healthcare Programs will pay the lower of the Medicare coinsurance and deductible or the Montana Healthcare Programs fee less Medicare payments for Montana Healthcare Programs covered services. If a service is covered by Medicare but not by Montana Healthcare Programs, Montana Healthcare Programs will not pay coinsurance, deductible, or any other cost of the service. For services Medicare does not cover but Montana Healthcare Programs covers, Montana Healthcare Programs will be the primary payer for that service.
- Qualifying Individual (QI). Montana Healthcare Programs pays the Medicare Part B premium only. Members should not have a dual eligibility when qualifying under the QI program. In other words, members cannot have QI and Montana Healthcare Programs at the same time. When a QI recipient becomes Montana Healthcare Programs-eligible, the QI benefit is canceled and replaced by the Montana Healthcare Programs eligibility.
Montana Healthcare Programs Benefits for Dually Eligible Members
Type of Dual Eligible: QMB only
Medicare Premium Paid by: Montana Healthcare Programs
Medicare Coinsurance and Deductible Paid by: Montana Healthcare Programs*
Type of Dual Eligible: QMB/Montana Healthcare Programs
Medicare Premium Paid by: Montana Healthcare Programs
Medicare Coinsurance and Deductible Paid by: Montana Healthcare Programs*
Type of Dual Eligible: Other dual eligibles
Medicare Premium Paid by: Member
Medicare Coinsurance and Deductible Paid by: Montana Healthcare Programs*
Type of Dual Eligible: Specified Low-Income Medicare Beneficiary
Medicare Premium Paid by: Montana Healthcare Programs
Medicare Coinsurance and Deductible Paid by: Member
*See the How Payment Is Made chapter in your provider type manual to learn how Montana Healthcare Programs calculates payment for Medicare coinsurance and deductibles.
Members with Other Sources of Coverage
Montana Healthcare Programs members may also have coverage through workers’ compensation, employment-based coverage, individually purchased coverage, etc. Other parties also may be responsible for healthcare costs. Examples of these situations include communal living arrangements, child support, or auto accident insurance. These other sources of coverage have no effect on what services Montana Healthcare Programs covers. However, other coverage does affect the payment procedures. (See the How Payment Is Calculated chapter in your provider type manual.)
The Health Insurance Premium Payment (HIPP) Program
Some Montana Healthcare Programs members have access to private insurance coverage, typically through a job, but do not enroll because they cannot afford the premiums. In these cases, Montana Healthcare Programs may pay the premiums, at which time the private insurance plan becomes the primary insurer. The member also remains eligible for Montana Healthcare Programs. When Montana Healthcare Programs members have access to private insurance coverage, they may apply for the HIPP program.
Indian Health Service (IHS)
The Indian Health Service (IHS) provides federal health services to American Indians and Alaska Natives. IHS is a secondary payer to Montana Healthcare Programs. For more information, see the Subsidized Health Insurance Programs in Montana table at the end of this chapter.
Crime Victims
The Crime Victim Compensation Program is designed to help victims of crime heal. This program may provide funding for medical expenses, mental health counseling, lost wages support, funerals, and attorney fees. Crime Victim Compensation is a secondary payer to Montana Healthcare Programs. For more information, see the Subsidized Health Insurance Programs in Montana table later in this chapter.
When Members Are Uninsured
Several state and federal programs are available to help the uninsured; see the Subsidized Health Insurance Programs in Montana table at the end of this chapter.
Member Responsibilities
Montana Healthcare Programs members are required to:
- Know and understand what Standard Montana Healthcare Programs benefits include.
- Notify providers that they have Montana Healthcare Programs coverage.
- Present a valid Montana Access to Health (MATH) or Healthy Montana Kids (HMK) Plus card at each visit.
- Notify providers of any other coverage, such as Medicare or private insurance.
- Notify providers of any change in coverage.
- Forward any money received from other insurance payers to the provider.
- Inform their local office of public assistance about any changes in address, income, etc.
Montana Healthcare Programs members may see any Montana Healthcare Programs-enrolled provider as long as Passport to Health and prior authorization guidelines are followed, and as long as they are not enrolled in Team Care.
Other Programs
Member eligibility provisions also apply to Department of Public Health and Human Services programs other than Montana Healthcare Programs. The information covered in this chapter applies to members enrolled in the Mental Health Services Plan (MHSP) and Healthy Montana Kids (HMK) dental services and eyeglasses only.
Chemical Dependency Bureau State Paid Substance Dependency/Abuse Treatment Program (CDB-SPSDATP)
Members in this program are not issued a Montana Access to Health card. Members should apply for services directly from the state-approved programs. For a list of these programs, call 406-444-9408. Services require prior authorization and authorization for continued stay review.
Healthy Montana Kids (HMK)
Few children are eligible for both Montana Healthcare Programs and HMK simultaneously. If a patient presents both cards, check the dates of Montana Healthcare Programs eligibility and the child’s HMK enrollment. If both cards are valid, treat the patient as an HMK patient. Services not covered by HMK may be covered by Montana Healthcare Programs.
If a member presents an HMK card for dental services, the provider should refer to the HMK dental services manual for information about coverage and billing. If a member presents an HMK card for eyeglasses, the card is valid only with the HMK program’s designated supplier. (See the HMK section of the Optometric and Eyeglass Services manual.) If a member presents an HMK card for any other service, see the HMK provider manual published by Blue Cross and Blue Shield of Montana. Call 1-800-447-7828 for more information.
Mental Health Services Plan (MHSP)
MHSP members will present a hard white plastic card. Their MHSP card makes them eligible only for those services covered by MHSP, which are described in the mental health and prescription drug manuals. Montana Healthcare Programs members do not need an MHSP card to receive mental health services.
Subsidized Health Insurance Programs in Montana
Providers may refer member to the following programs.
Program: Children’s Special Health Services
Administered by: Montana DPHHS
Target Populations: Children with special healthcare needs.
For Information on Eligibility:
(800) 762-9891
(406) 444-3622
Program: Crime Victim Compensation Program
Administered by: Montana Department of Justice
Target Populations: Crime victims and their dependents and relatives.
For Information on Eligibility:
406-444-3653 Helena
800-498-6455
https://dojmt.gov/victims/crime-victim-compensation/
Program: Indian Health Service
Administered by: Billings Area Indian Health Service
Target Populations: All enrolled members of federally recognized tribes.
For Information on Eligibility:
406-247-7107
Program: Montana Healthcare Programs
Administered by: Montana DPHHS
Target Populations: Low-income children and their family members, and disabled individuals.
For Information on Eligibility:
Local Office of Public Assistance
https://dphhs.mt.gov/hcsd/OfficeofPublicAssistance
Program: Medicare
Administered by: Centers for Medicare and Montana Healthcare Programs Services
Target Populations: People who are age 65 and over, have a disability, or have end-stage renal disease.
For Information on Eligibility:
U.S. Social Security Administration office
Program: Mental Health Services Plan (MHSP)
Administered by: Montana DPHHS
Target Populations: Individuals with a qualifying mental health diagnosis who are ineligible for Montana Healthcare Programs.
For Information on Eligibility:
Community Mental Health Center
https://dphhs.mt.gov/BHDD/mentalhealthservices/MHSP/index
Program: Workers’ Compensation
Administered by: State Fund and independent workers’ compensation insurers
Target Populations: People with injuries or illnesses related to their work.
For Information on Eligibility:
406-444-6543 Workers Compensation
Note: Eligibility rules are complex; members and providers should check with the program administrator for specifics.
End of Member Eligibility and Responsibilities Chapter
Surveillance and Utilization Review
Claims Review (MCA 53-6-111, ARM 37.85.406)
The Department is committed to paying Montana Healthcare Programs providers’ claims as quickly as possible. Montana Healthcare Programs claims are electronically processed and usually are not reviewed by medical experts prior to payment to determine if the services provided were appropriately billed. Although the computerized system can detect and deny some erroneous claims, there are many erroneous claims it cannot detect. For this reason, payment of a claim does not mean the service was correctly billed or the payment made to the provider was correct. Periodic retrospective reviews are performed that may lead to the discovery of incorrect billing or incorrect payment. If a claim is paid and the Department later discovers the service was incorrectly billed or paid or the claim was erroneous in some other way, the Department is required by federal regulation to recover any overpayment, regardless of whether the incorrect payment was the result of Department or provider error or other cause.
Surveillance and Utilization Review (42 CFR 456)
The Department’s Surveillance and Utilization Review Section (SURS) performs federally mandated retrospective reviews of paid claims (42 CFR 456). SURS is required to safeguard against unnecessary and inappropriate use of Montana Healthcare Programs services and against excess payments. If the Department pays a claim, but subsequently discovers that the provider was not entitled to payment for any reasons, the Department is entitled to recover the resulting overpayment (ARM 37.85.406).
SURS monitors compliance with state and federal rules, laws, and policies in several ways:
- New Provider Audits. SURS reviews the billing data of newly enrolled providers and may also review documentation.
- Provider Self-Audits. A self-audit is an opportunity for the provider to perform an audit and self-disclose errors to SURS. Providers may access the website for Office of Inspector General (OIG) provider self-disclosure protocol resources at http://oig.hhs.gov/compliance/self-disclosure-info/index.asp.
- Individual Audits. An individual audit is conducted by the Program Integrity Compliance Specialist in charge of reviewing the provider type being audited.
- Team Audits. Team audits are conducted by a team of Program Integrity Compliance Specialists whose individual expertise contributes to the review of the issue being audited.
- Data Mining Audits. An audit conducted by data mining which reviews the appropriateness of the data submitted on the claim, such as dates of service, procedure code, units, etc.
- Statistical Sampling. When a provider is audited, claims data is gathered for the audit time frame. If a provider has a large number of claims for which records collection and submission for a complete review would be burdensome to the provider, a statistical sample of the claims may be reviewed at the option of the Department. SURS uses a program called RAT-STATS to pull a random subset (sample) of the total claims under review (universe). The audit is then completed on the sample of claims. The determination made on the sample is then extrapolated to the entire universe. If a provider disagrees with the final determination, a 100% review of claims may be requested by the provider. More information about the statistical sampling process can be found in ARM 37.85.416.
During an audit, SURS personnel send a spreadsheet to the provider with paid claims data. The provider is required to send supporting documentation for the items listed on the spreadsheet. A SURS Program Integrity Compliance Specialist reviews the documentation and/or data submitted by the provider.
If SURS determines an overpayment that exceeds $5,000, the audit is presented to the Montana Healthcare Programs Review Committee for review and approval. With the approval of the committee, an overpayment letter will be sent to the provider.
If SURS determines an overpayment that is less than $5,000, the case is reviewed by the associated program bureau chief, program officer, SURS supervisor, and Program Compliance bureau chief. Their approval will initiate an overpayment letter to the provider.
The overpayment letter specifies the amount of the overpayment, the date the funds are due, how to appeal the Department’s decision, and the appropriate contact person.
Key Points
- The SURS unit encourages providers to call with any questions or concerns regarding the audit of paid claims.
- The Department is entitled to recover payment made to providers when a claim was paid incorrectly for any reason. (MCA 53-6-111, ARM 37.85.406)
- The Department may charge interest on recovered funds. (MCA 53-6-111)
- When an inappropriate payment has been identified, the Department may recover the overpayment by any legal means, including withholding of provider payments on subsequent claims. (MCA 53-6-111)
- The Department may sanction a provider, including suspension or termination of Montana Healthcare Programs enrollment, if the provider has failed to abide by terms of the Montana Healthcare Programs contract, federal and state laws, regulations and/or policies. (MCA 53-6-111, ARM 37.85.501–502, ARM 37.85.513)
- Prior authorization does not guarantee payment; a claim may be denied or money paid to providers may be recovered if the claim is found to be inappropriate. (MCA 53-6-111, ARM 37.85.406, ARM 37.85.410)
- The provider must upon request provide to the Department or its designated review organization without charge any records related to services or items provided to a member. The provider shall submit a true and accurate copy of each record of the service or item being reviewed as it existed within 90 days after the date on which the claim was submitted to Montana Healthcare Programs. (ARM 37.85.410, ARM 37.85.414)
Billing Tips
The following suggestions may help reduce billing errors but are not inclusive of all possible errors and recoupment scenarios.
- Be familiar with the Montana Healthcare Programs provider manuals, fee schedules, and provider notices that are in effect for the claim dates of service. Read the Claim Jumper provider newsletter. These are available on the Provider Information website.
- Comply with applicable state and federal regulations, including but not limited to the Administrative Rules of Montana. (ARM 37.85.401)
- Use CPT, HCPCS, and ICD coding books that are in effect for the claim dates of service, and refer to the long descriptions. Relying on short descriptions can result in inappropriate billing. Additional coding resources such as those noted in CPT are also recommended.
- All providers of services must maintain complete records which fully demonstrate the extent, nature, and medical necessity of services and items provided to Montana Healthcare Programs members. Information regarding the minimum requirements for records are found in ARM 37.85.414. In addition to complying with these minimum requirements, providers must also comply with any specific record keeping requirements applicable to the type of services the provider furnishes. See the Record Keeping section in the Provider Requirements chapter in this manual.
- When reimbursement is based on the length of time spent providing the service, the records must specify the time spent or the time treatment began and ended for each procedure. (ARM 37.85.414)
- Attend classes on coding offered by certified coding specialists.
- Avoid billing for the same service/supply twice. Contact Provider Relations for the status of submitted claims.
- Use specific codes rather than miscellaneous codes. For example, Code 99213 is more specific (problem-focused visit) than Code 99499 (unlisted evaluation and management service).
- Verify that the item/service meets criteria for payment by the Department. (See current fee schedule, provider manuals, and Administrative Rules of Montana.)
- Bill only under your own provider number.
- Bill only for services you provided.
- Bill for the appropriate level of service provided. For example, the CPT coding book contains detailed descriptions and examples of what differentiates a level 1 office visit (Code 99201) from a level 5 office visit (Code 99205).
- Services covered within “global periods” for certain CPT procedures are not paid separately and should not be billed separately. Most surgical and obstetric procedures and some medical procedures include routine care before and after the procedure. Montana Healthcare Programs fee schedules show the global period for each CPT service.
- Pay close attention to modifiers used with CPT and HCPCS codes on both CMS-1500 bills and UB-04 bills. Modifiers are becoming more prevalent in healthcare billing, and they often affect payment calculations.
- Choose the least costly alternative. For example, if a member is able to operate a standard wheelchair, then a motorized wheelchair should not be prescribed or provided.
- For repeat members, use an established patient code (e.g., Code 99213) instead of a first time patient code (e.g., Code 99203).
- Use the correct units measurement on CMS-1500 and UB-04 bills. In general, Montana Healthcare Programs follows the definitions in the CPT and HCPCS coding books. Unless otherwise specified, one unit equals one visit or one procedure. For specific codes, however, one unit may be 15 minutes, a percentage of body surface area, or another quantity. Always check the long text of the code description. A service must take at least 8 minutes to bill one unit of service if the procedure has “per 15 minutes” in its description.
End of Surveillance and Utilization Review Chapter
Billing Procedures
Claim Forms
Services provided by the healthcare professionals covered in this manual may be billed electronically or on paper claim forms, which are available from various publishing companies; they are not available from the Department or Provider Relations.
Timely Filing Limits (ARM 37.85.406)
Providers must submit clean claims to Montana Healthcare Programs within:
- Twelve months from whichever is later:
- the date of service
- the date retroactive eligibility or disability is determined
- Six months from the date on the Medicare explanation of benefits approving the service.
- Six months from the date on an adjustment notice from a third party payer who has previously processed the claim for the same service, and the adjustment notice is dated after the periods described above.
For claims involving Medicare or TPL, if the 12-month time limit has passed, providers must submit clean claims to Montana Healthcare Programs within:
- Medicare Crossover Claims. Six months from the date on the Medicare explanation of benefits, if the Medicare claim was timely filed and the member eligible for Medicare at the time the Medicare claim was filed.
- Claims Involving Other Third Party Payers (excluding Medicare). Six months from the date on an adjustment notice from a third party payer who has previously processed the claim for the same service, and the adjustment notice is dated after the periods described above.
Clean claims are claims that can be processed without additional information or action from the provider. The submission date is defined as the date that the claim was received by the Department or the claims processing contractor. All problems with claims must be resolved within this 12-month period.
Tips to Avoid Timely Filing Denials
- Correct and resubmit denied claims promptly. (See the Remittance Advices and Adjustments chapter in this manual.)
- If a claim submitted to does not appear on the remittance advice within 45 days, contact Provider Relations for claim status.
- If another insurer has been billed and 90 days have passed with no response, a provider can bill Montana Healthcare Programs . (See the Member Eligibility and Responsibilities chapter in this manual for more information.)
- To meet timely filing requirements for Medicare/Montana Healthcare Programs crossover claims, see the Member Eligibility and Responsibilities chapter in this manual and, if applicable, the Coordination of Benefits chapter in your provider type manual.
When to Bill Montana Healthcare Programs Members (ARM 37.85.406)
Providers may not bill Montana Healthcare Programs members for services covered under Montana Healthcare Programs .
If a provider bills Montana Healthcare Programs and the claim is denied because the member is not eligible, the provider may bill the member directly.
More specifically, providers cannot bill members directly:
- For the difference between charges and the amount Montana Healthcare Programs paid.
- For a covered service provided to a Montana Healthcare Program-enrolled member who was accepted as a Montana Healthcare Programs member by the provider, even if the claim was denied.
- When a third party payer does not respond.
- When a member fails to arrive for a scheduled appointment. Montana Healthcare Programs may not be billed for no-show appointments either.
- When services are free to the member, such as in a public health clinic. Montana Healthcare Programs may not be billed for those services either.
Exceptions are outlined in ARM 37.85.204.
Under certain circumstances, providers may need a signed agreement to bill a member.
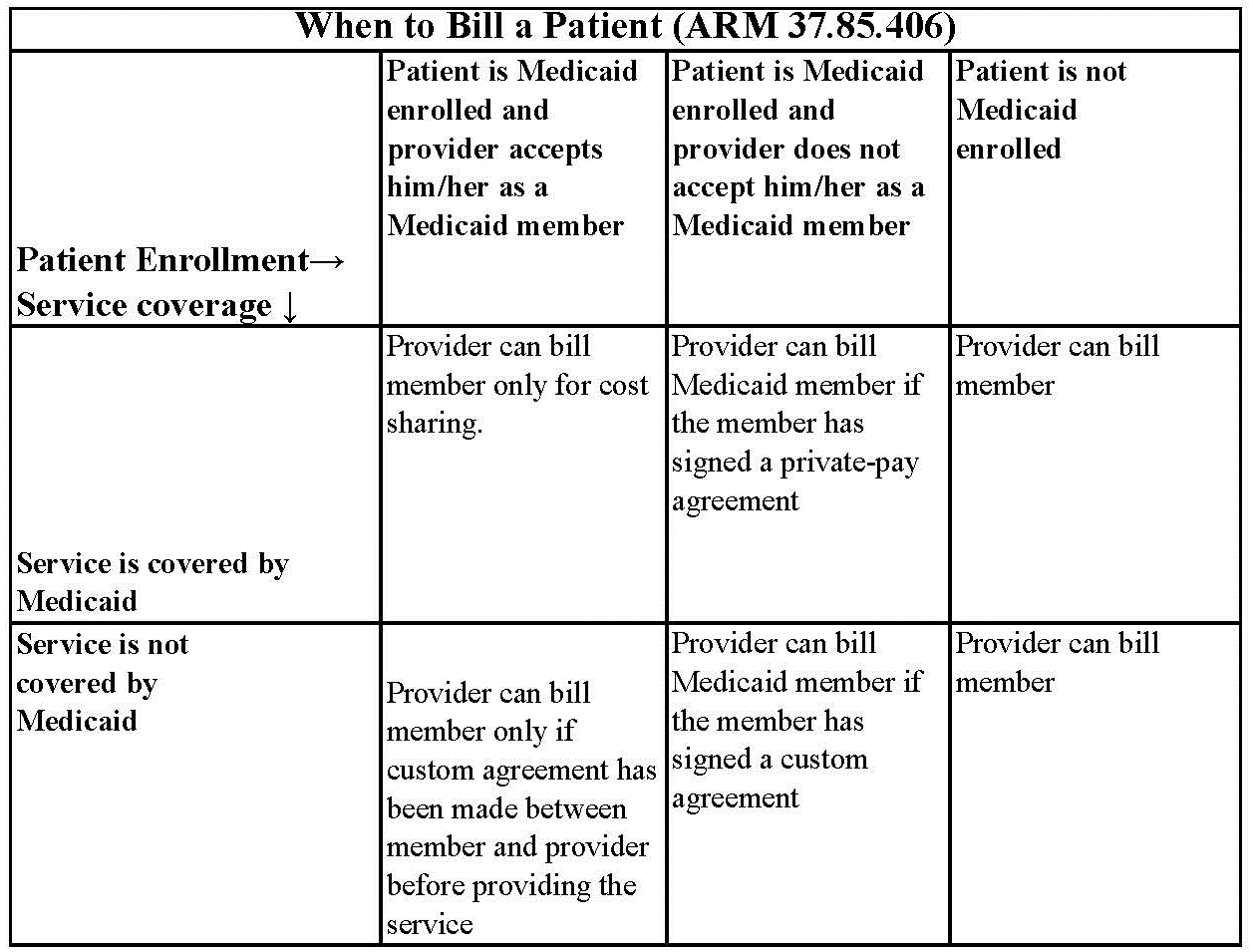
Private-Pay Agreement. A nonspecific private-pay agreement between the provider and member stating that the member is not accepted as a Montana Healthcare Programs member, and that he/she must pay for the services received.
Custom Agreement. A specific agreement that includes the dates of service, actual services or procedures, and the cost to the member. It states the services are not covered by Montana Healthcare Programs and the member will pay for them.
Member Co-Payment (ARM 37.85.204)
Effective for claims paid on or after January 1, 2020, members covered under Montana Healthcare Programs or Medicaid Expansion will not be assessed a co-payment, as denied in ARM 37.84.102, for any covered service.
Billing for Members with Other Insurance
A Montana Healthcare Programs member may also be covered by Medicare or have other insurance, or some other third party is responsible for the cost of the member’s healthcare,
When completing a claim for members with Medicare and Montana Healthcare Programs , Medicare coinsurance and deductible amounts must correspond with the payer listed. For example, if the member has Medicare and Montana Healthcare Programs , any Medicare deductible and coinsurance amounts must be listed and preceded by an A1, A2, etc. Because these amounts are for Medicare, Medicare must be listed in the corresponding field. (See the Submitting a Claim section in this manual.)
Billing for Retroactively Eligible Members
When a member becomes retroactively eligible for Montana Healthcare Programs , the provider may:
- Accept the member as a Montana Healthcare Programs member from the current date.
- Accept the member as a Montana Healthcare Programs member from the date retroactive eligibility was effective.
- Require the member to continue as a private-pay member.
Always refer to the long descriptions in coding books.
When the provider accepts the member’s retroactive eligibility, the provider has 12 months from the date retroactive eligibility was determined to bill for those services. When submitting claims for retroactively eligible members in which the date of service is more than 12 months earlier than the date the claim is submitted, attach a copy of the Provider Notice of Eligibility (Form 160-M). To obtain this form, the provider should contact the member’s county Office of Public Assistance. See https://dphhs.mt.gov/hcsd/OfficeofPublicAssistance.
When a provider chooses to accept the member from the date retroactive eligibility was effective, and the member has made a full or partial payment for services, the provider must refund the member’s payment for the services before billing Montana Healthcare Programs for the services.
Coding Tips
Standard use of medical coding conventions is required when billing Montana Healthcare Programs . Provider Relations or the Department cannot suggest specific codes to be used in billing for services. See the Coding Resources table. The following may reduce coding errors and unnecessary claim denials:
- Use current CPT, CDT, HCPCS, and ICD diagnosis coding books.
- Always read the complete description and guidelines in the coding books. Relying on short descriptions can result in inappropriate billing.
- Attend classes on coding offered by certified coding specialists.
- Use specific codes rather than unlisted codes.
- Bill for the appropriate level of service provided. Evaluation and management services have 3 to 5 levels. See your CPT manual for instructions on determining appropriate levels of service.
- CPT codes that are billed based on the amount of time spent with the member must be billed with the code that is closest to but not over the time spent.
- Revenue Codes 25X are required to have valid and rebateable National Drug Codes (NDCs) on each line to be paid.
- Revenue Codes 27X do not require CPT or HCPCS codes; however, providers are advised to place appropriate NDC, CPT, and/or HCPCS codes on each line. Providers are paid based on the presence of line item CPT and HCPCS codes. If these codes are omitted, hospitals may be underpaid.
- Take care to use the correct units measurement. In general, Montana Healthcare Programs follows the definitions in the CPT and HCPCS coding books. Unless otherwise specified, one unit equals one visit or one procedure. For specific codes, however, one unit may be “each 15 minutes. A service must take at least 8 minutes to bill one unit of service if the procedure has “per 15 minutes” in its description. Always check the long text of the code description published in the CPT or HCPCS coding books.
Coding Resources
Please note that the Department does not endorse the products of any particular publisher.
CDT - http://www.ada.org/en/publications/
Description:
The CDT is the official coding used by dentists.
Contact:
American Dental Association
(312) 440-2500
CPT - https:/commerce.ama-assn.org/store/
Description:
CPT codes and definitions.
Updated each January.
Contact:
American Medical Association
(800) 621-8335
CPT Assistant - https://commerce.ama-assn.org/store/
Description:
A newsletter on CPT coding issues.
Contacts:
American Medical Association
(800) 621-8335
HCPCS Level II
Description:
HCPCS codes and definitions.
Updated each January and throughout the year.
Contact:
Available through various publishers and bookstores or from CMS at www.cms.gov.
ICD
Description:
ICD diagnosis and procedure code definitions.
Updated each October .
Contact:
Available through various publishers and bookstores.
Various newsletters and other coding resources are available in the commercial marketplace.
Number of Lines on Claim
The Montana claims processing system supports 40 lines on a UB-04 claim, 21 lines on a CMS-1500, and 21 lines on a dental claim.
Multiple Services on Same Date
Outpatient hospital providers must submit a single claim for all services provided to the same member on the same day. If services are repeated on the same day, use appropriate modifiers. The only exception to this is if the member has multiple emergency room visits on the same date. Two or more emergency room visits on the same day must be billed on separate claims with the correct admission hour on each claim.
Span Bills
Outpatient hospital providers may include services for more than one day on a single claim, so long as the service is paid by fee schedule (e.g., partial hospitalization, therapies) and the date is shown on the line. However, the Outpatient Code Editor (OCE) will not price APC procedures when more than one date of service appears at the line level, so we recommend billing for only one date at a time when APC services are involved.
Reporting Service Dates
All line items must have a valid date of service. The revenue codes on the following page require a separate line for each date of service and a valid CPT or HCPCS code:
Revenue Codes That Require a Separate Line for Each Date of Service and a Valid CPT or HCPCS Code
26X - IV Therapy
28X - Oncology
30X - Laboratory
31X - Laboratory Pathological
32X -Radiology – Diagnostic
33X - Radiology – Therapeutic
34X - Nuclear Medicine
35X - Computed Tomographic (CT) Scan
36X - Operating Room Services
38X - Blood
39X - Blood Storage and Processing
40X - Other Imaging Services
41X - Respiratory Services
42X - Physical Therapy
43X - Occupational Therapy
44X - Speech-Language Pathology
45X - Emergency Department
46X - Pulmonary Function
47X - Audiology
48X - Cardiology
49X - Ambulatory Surgical Care
51X - Clinic
52X - Free-Standing Clinic
61X - Magnetic Resonance Imaging (MRI)
63X - Drugs Requiring Specific Identification
70X - Cast Room
72X - Labor Room/Delivery
73X - Electrocardiogram (EKG/ECG)
74X - Electroencephalogram (EEG)
75X - Gastro-Intestinal Services
76X - Treatment or Observation Room
77X - Preventive Care Services
79X - Lithotripsy
82X - Hemodialysis – Outpatient or Home
83X - Peritoneal Dialysis – Outpatient or Home
84X - Continuous Ambulatory Peritoneal Dialysis (CAPD) – Outpatient
85X - Continuous Cycling Peritoneal Dialysis (CCPD) – Outpatient
88X - Miscellaneous Dialysis
90X - Psychiatric/Psychological Treatments
91X - Psychiatric/Psychological Services
92X - Other Diagnostic Services
94X - Other Therapeutic Services
Using Modifiers
- Review the guidelines for using modifiers in the most current CPT book, HCPCS book, and other helpful resources (e.g., CPT Assistant, APC Answer Letter, and others).
- Always read the complete description for each modifier; some modifiers are described in the CPT manual while others are in the HCPCS book.
- Montana Healthcare Programs accepts most of the same modifiers as Medicare, but not all.
- The Montana Healthcare Programs claims processing system recognizes three pricing modifiers and one informational modifier per claim line on the CMS-1500. Providers are asked to place any modifiers that affect pricing in the first two modifier fields.
- Discontinued or reduced service modifiers must be listed before other pricing modifiers on the CMS-1500. For a list of modifiers that change pricing, see the How Payment Is Calculated chapter in this manual.
Billing Tips for Specific Services
Prior authorization is required for some services. Passport and prior authorization are different; some services may require both. Different numbers are issued for each type of approval and must be included on the claim form.
Abortions
A completed Montana Healthcare Programs Physician Certification for Abortion Services (MA-37) form must be attached to every abortion claim or payment will be denied. Complete only one section of this form. This is the only form Montana Healthcare Programs accepts for abortions.
Drugs and Biologicals
While most drugs are bundled, there are some items that have a fixed payment amount and some that are designated as transitional pass-through items. (See the Pass-Through section in the How Payment Is Calculated chapter of this manual.) Bundled drugs and biologicals have their costs included as part of the service with which they are billed. The following drugs may generate additional payment:
- Vaccines, antigens, and immunizations
- Chemotherapeutic agents and the supported and adjunctive drugs used with them
- Immunosuppressive drugs
- Orphan drugs
- Radiopharmaceuticals
- Certain other drugs, such as those provided in an emergency department for heart attacks
NDC Requirements
The Federal Deficit Reduction Act of 2005 mandates that all State Montana Healthcare Programs require the submission of National Drug Codes (NDCs) on claims submitted with certain procedure codes for physician-administered drugs. This mandate affects all providers who submit claims for procedure-coded drugs both electronically and manually.
Montana Healthcare Programs require all claims submitted for physician administered drugs to include the NDC(s), the corresponding CPT/HCPCS code(s), unit of measure, and the units administered for each code. Montana Healthcare Programs will only reimburse for drugs manufactured by companies that have a signed rebate agreement with the Centers for Medicare and Montana Healthcare Programs Services (CMS). A list of drug manufacturers who have a rebate agreement with CMS can be found on the provider website, https://medicaidprovider.mt.gov/, under the Rebateable Manufacturers list in the Site Index.
When a procedure or revenue code requires an NDC, Montana Healthcare Programs covers only those NDCs that are rebateable. An NDC is considered rebateable ONLY if all the following conditions are met:
-
The drug is a Montana Healthcare Programs covered drug
-
The NDC on the drug dispensed is valid
-
The drug dispensed is NOT terminated
-
The drug is a product of an eligible manufacturer
-
The DESI indicator is NOT 5 or 6.
NDC Formatting
When billing Montana Healthcare Programs, the required NDC is 11-digits. The NDC should be structured in the 5-4-2 format. Some manufacturers omit leading zeros in one of the three positions. This results in a 10-digit number, which is invalid. To ensure proper reimbursement, the provider must add the appropriate leading zero to the affected segment of the format.
The below table provides examples of where the leading zero should be placed in three separate instances.
NDC Example Conversion: 10 Digit to 11 Digit
Leading Zero Location Examples of 10 Digit Format: Add a zero (0) to:
5 digit segment XXXX-XXXX-XX 0XXXX-XXXX-XX
4 digit segment XXXXX-XXX-XX XXXXX-0XXX-XX
2 digit segment XXXXX-XXXX-X XXXXX-XXXX-0X
Reporting a NDC on paper CMS-1500, under Form Locator 24 (A) must included the following:
-
Enter the NDC qualifier of “N4” in the first two positions on the left side of the field.
-
Enter the 11-digit NDC numeric code in the 5-4-2 format, without the hyphens.
-
Enter the NDC unit of measure qualifier, such as:
-
F2 — International Unit
-
GR — Gram (includes mg, mcg)
-
ML — Milliliter
-
UN — Units (includes “each”)
-
-
Enter the NDC quantity (the administered amount) with up to three decimal places.
-
When using the paper CMS-1500, insert a space between the 11-digit NDC and the unit of measure.
Example only: N459148001665 ML0.8
Reporting a NDC on a paper UB-04, in Form Locator 43, in the Revenue Description Field must included the following:
-
Enter the NDC qualifier of “N4” in the first two positions on the left side of the field.
-
Enter the 11-digit NDC numeric code in the 5-4-2 format., without delimiters such as hyphens or commas
-
Enter the NDC unit of measure qualifier, such as:
-
F2 — International Unit
-
GR — Gram (includes mg, mcg)
-
ML — Milliliter
-
UN — Units (includes “each”)
-
-
Enter the NDC quantity (the administered amount) with up to three decimal places.
-
Any unused spaces for the entire quantity are left blank.
-
The Description Field allows for a maximum of 24 total characters.
Example only: N459148001665ML0.8
The NDC on the claim MUST be the NDC that was dispensed to the member. DO NOT include the name of the physician-administered drug when reporting the NDC.
Compound Drugs
Professional providers that bill compound drugs using the paper CMS-1500 must bill them using the corresponding CPT/HCPCS codes and NDC on paper claim forms and must attach the supplier’s invoice. The invoice must contain an NDC for each component of the compound. Invoices that do not include NDCs will be denied. Payment will be made from the NDCs listed on the invoices that qualify for rebates.
Crossover Claims
Dual-eligible claims billed to Medicare with an NDC will cross to Montana Healthcare Programs with the NDC. Any claim with a physician-administered drug crossing to Montana Healthcare Programs from Medicare without an NDC will be denied. Claims denied for this reason may be re-billed with the proper NDC within one year of the date of service.
340B Drug Pricing Programs or Vaccines
Providers participating in the 340B Drug Pricing Programs are not required to include NDC information on the claim. Vaccines do not require NDC information.
Lab Services
If all tests that make up an organ or disease organ panel are performed, the panel code should be billed instead of the individual tests.
Some panel codes are made up of the same test or tests performed multiple times. When billing one unit of these panels, bill one line with the panel code and one unit. When billing multiple units of a panel (the same test is performed more than once on the same day) bill the panel code with units corresponding to the number of times the panel was performed.
Outpatient Clinic Services
Montana Healthcare Programs does not recognize provider-based clinic status in reimbursing evaluation and management codes on the institutional claims (UB-04/8381) transactions. Clinic services provided by an individual physician or mid-level practitioner in the clinic must be billed on a CMS 1500 with place of service (POS) 11.
For services that have both technical and professional components, physicians providing services in hospitals must bill only for the professional component if the hospital is going to bill Montana Healthcare Programs for the technical component. Refer to the Physician-Related Services manual and the Billing Procedures chapter in this manual for more information. Provider type manuals are located on the provider type pages of the Provider Information website.
Partial Hospitalization
Partial hospitalization services must be billed with the national code for partial hospitalization, the appropriate modifier, and the prior authorization code.
Current Payment Rates for Partial Hospitalization
Code: H0035 Modifier: — Service Level: Partial hospitalization, sub-acute, half day
Code: H0035 Modifier: U6 Service Level: Partial hospitalization, sub-acute, full day
Code: H0035 Modifier: U7 Service Level: Partial hospitalization, acute, half day
Code: H0035 Modifier: U8 Service Level: Partial hospitalization, acute, full day
Sterilization/Hysterectomy (ARM 37.86.104)
Elective sterilizations are sterilizations done for the purpose of becoming sterile. Montana Healthcare Programs covers elective sterilization for men and women when all of the following requirements are met:
- Member must complete and sign the Informed Consent to Sterilization (MA-38) form at least 30 days, but not more than 180 days, prior to the sterilization procedure. This form is the only form Montana Healthcare Programs accepts for elective sterilizations. If this form is not properly completed, payment will be denied. The 30-day waiting period may be waived for either of the following:
- Premature Delivery. The Informed Consent to Sterilization must be completed and signed by the member at least 30 days prior to the estimated delivery date and at least 72 hours prior to the sterilization.
- Emergency Abdominal Surgery. The Informed Consent to Sterilization form must be completed and signed by the member at least 72 hours prior to the sterilization procedure.
- Member must be at least 21 years of age when signing the form.
- Member must not have been declared mentally incompetent by a federal, state, or local court, unless the member has been declared competent to specifically consent to sterilization.
- Member must not be confined under civil or criminal status in a correctional or rehabilitative facility, including a psychiatric hospital or other correctional facility for the treatment of the mentally ill.
Before performing a sterilization, the following requirements must be met:
- The member must have the opportunity to have questions regarding the sterilization procedure answered to his/her satisfaction.
- The member must be informed of his/her right to withdraw or withhold consent anytime before the sterilization without being subject to retribution or loss of benefits.
- The member must be made aware of available alternatives of birth control and family planning.
- The member must understand the sterilization procedure being considered is irreversible.
- The member must be made aware of the discomforts and risks which may accompany the sterilization procedure being considered.
- The member must be informed of the benefits and advantages of the sterilization procedure.
- The member must know that he/she must have at least 30 days to reconsider his/her decision to be sterilized.
- An interpreter must be present and sign for members who are blind or deaf, or do not understand the language to assure the person has been informed.
Informed consent for sterilization may not be obtained under the following circumstances:
- If the member is in labor or childbirth.
- If the member is seeking or obtaining an abortion.
- If the member is under the influence of alcohol or other substance which affects his/her awareness.
For elective sterilizations, a completed Informed Consent to Sterilization (MA-38) form must be attached to the claim for each provider involved or payment will be denied. This form must be legible, complete, and accurate. It is the provider’s responsibility to obtain a copy of the form from the primary or attending physician.
For medically necessary sterilizations, including hysterectomies, oophorectomies, salpingectomies, and orchiectomies, one of the following must be attached to the claim, or payment will be denied:
- A completed Montana Healthcare Programs Hysterectomy Acknowledgement form (MA-39) for each provider submitting a claim. It is the billing provider’s responsibility to obtain a copy of the form from the primary or attending physician. Complete only one section of this form. When no prior sterility (Section B) or life-threatening emergency (Section C) exists, the member (or representative, if any) and physician must sign and date Section A of this form prior to the procedure. (See 42 CFR 441.250 for the federal policy on hysterectomies and sterilizations.) Also, for Section A, signatures dated after the surgery date require manual review of medical records by the Department. The Department must verify that the member (and representative, if any) was informed orally and in writing, prior to the surgery, that the procedure would render the member permanently incapable of reproducing. The member does not need to sign this form when Sections B or C are used.
- For members who have become retroactively eligible for Montana Healthcare Programs , the physician must certify in writing that the surgery was performed for medical reasons and must document one of the following:
- The individual was informed prior to the hysterectomy that the operation would render the member permanently incapable of reproducing.
- The reason for the hysterectomy was a life-threatening emergency.
- The member was already sterile at the time of the hysterectomy and the reason for prior sterility.
When submitting claims for retroactively eligible members, for which the date of service is more than 12 months earlier than the date the claim is submitted, contact the member’s local Office of Public Assistance and request a Notice of Retroactive Eligibility (160-M). Attach the form to the claim.
Supplies
Supplies are generally bundled, so they usually do not need to be billed individually. A few supplies are paid separately by Montana Healthcare Programs . The fee schedules on the website lists the supply codes that may be separately payable.
Submitting a Claim
Paper Claims
Unless otherwise stated, all paper claims must be mailed to:
Claims Processing
P.O. Box 8000
Helena, MT 59604
On the CMS-1500, EPSDT/Family Planning, is used as an indicator to specify additional details for certain members or services. The following are accepted codes:
EPSDT/Family Planning Indicators
Code: 1 Member/Service: EPSDT
Purpose: Used when the member is under age 21.
Code: 2 Member/Service: Family planning
Purpose: Used when providing family planning services.
Code: 3 Member/Service: EPSDT and family planning
Purpose: Used when the member is under age 21 and is receiving family planning services.
Code: 4 Member/Service: Pregnancy (any service provided to a pregnant woman)
Purpose: Used when providing services to pregnant women.
Code: 6 Member/Service: Nursing facility member
Purpose: Used when providing services to nursing facility residents.
Submitting Electronic Claims
Providers who submit claims electronically experience fewer errors and quicker payment. Claims may be submitted using the methods below. For detailed submission methods, see the electronic submissions manual on the Electronic Billing page of the website.
- WINASAP 5010. This free software provided by Conduent allows for the creation of basic claim submissions. Please note that this software is not compatible with Windows 10 and has limited support as it is free software.
o Utilizes either a dial-up modem or submissions through the Montana Access to Health (MATH) Web Portal.
o Requires completion of the X12N Transaction Packet to allow for claim submissions.
- Clearinghouses/Contracted Claim Submitter. Providers can make arrangements with a clearinghouse/contracted claim submitter for claim submission. Please note that the clearinghouse must be enrolled to submit claims to Montana Healthcare Programs .
- Montana Access to Health (MATH) Web Portal . A secure website that allows providers to verify eligibility, check claim status, and view medical claims history. Valid X12N files can be uploaded through this website.
o Requires completion of the X12N Transactions Packet to allow for claim submissions.
- MoveIt DMZ. This secure transfer protocol is for providers and clearinghouses that submit large volumes of files (in excess of 20 per day) or are regularly submitting files larger than 2 MB. This utilizes SFTP and an intermediate storage area for the exchange of files.
o A request for this must be made through Conduent Provider Relations for established trading partners.
Providers should be familiar with federal rules and regulations related to electronic claims submission.
Billing Electronically With Paper Attachments
When submitting claims that require additional supporting documentation, the Attachment Control Number field must be populated with an identifier.
Identifier formats can be designed by software vendors or clearinghouses, but the preferred method is the provider's Montana Healthcare Programs ID number followed by the member's ID number and the date of service, each separated by a dash:
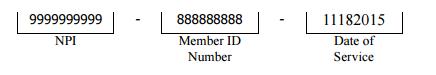
When submitting claims that require additional supporting documentation, the Attachment Control Number field must be populated with an identifier. Identifier formats can be designed by software vendors or clearinghouses, but the preferred method is the provider's Montana Healthcare Programs ID number followed by the member's ID number and the date of service, each separated by a dash:
The supporting documentation must be submitted with a Paperwork Attachment Cover Sheet. ( See Forms page on the Provider Information website.) The number in the paper Attachment Control Number field must match the number on the cover sheet.
Claim Inquiries
Contact Provider Relations for general claim questions and questions regarding payments, denials, member eligibility.
The Most Common Billing Errors and How to Avoid Them
Paper claims are often returned to the provider before they can be processed, and many other claims, both paper and electronic, are denied. To avoid unnecessary returns and denials, double check each claim to confirm the following items are included and accurate.
Common Billing Errors
Reasons for Return or Denial: Provider’s National Provider Identifier (NPI) and/or Taxonomy is missing or invalid
How to Prevent Returned or Denied Claims:
- The provider NPI is a 10-digit number assigned to the provider by the national plan and provider enumerator system. Verify the correct NPI and Taxonomy are on the claim.
Reasons for Return or Denial: Authorized signature missing
How to Prevent Returned or Denied Claims:
- Each claim must have an authorized signature belonging to the provider, billing clerk, or office personnel. The signature may be typed, stamped, hand-written, or computer-generated.
Reasons for Return or Denial: Signature date missing
How to Prevent Returned or Denied Claims:
- Each claim must have a signature date.
Reasons for Return or Denial: Incorrect claim form used
How to Prevent Returned or Denied Claims:
- The claim must be the correct form for the provider type.
Reasons for Return or Denial: Information on claim form not legible
How to Prevent Returned or Denied Claims:
- Information on the claim form must be legible. Use dark ink and center the information in the form locator. Information must not be obscured by lines.
Reasons for Return or Denial: Member ID number not on file, or member was not eligible on date of service
How to Prevent Returned or Denied Claims:
- Before providing services to the member, verify member eligibility by using one of the methods described in the Member Eligibility and Responsibilities chapter of this manual. Montana Healthcare Programs eligibility may change monthly.
Reasons for Return or Denial: Procedure requires Passport provider referral – No Passport provider number on claim
How to Prevent Returned or Denied Claims:
- A Passport provider number must be on the claim form when a referral is required. Passport approval is different from prior authorization. See the Passport to Health provider manual.
Reasons for Return or Denial: Prior authorization number is missing
How to Prevent Returned or Denied Claims:
- Prior authorization is required for certain services, and the prior authorization number must be on the claim form. Prior authorization is different from Passport. See the Prior Authorization chapter in this manual.
Reasons for Return or Denial: Prior authorization does not match current information
How to Prevent Returned or Denied Claims:
- Claims must be billed and services performed during the prior authorization span. The claim will be denied if it is not billed according to the spans on the authorization.
Reasons for Return or Denial: Duplicate claim
How to Prevent Returned or Denied Claims:
- Check all remittance advices for previously submitted claims before resubmitting.
- When making changes to previously paid claims, submit an adjustment form rather than a new claim form. (See Remittance Advices and Adjustments in this manual.)
Reasons for Return or Denial: TPL on file and no credit amount on claim
How to Prevent Returned or Denied Claims:
- If the member has any other insurance (or Medicare), bill the other carrier before Montana Healthcare Programs .
- If the member’s TPL coverage has changed, providers must notify the TPL unit before submitting a claim.
Reasons for Return or Denial: Claim past 365-day filing limit
How to Prevent Returned or Denied Claims:
- The Claims Processing unit must receive all clean claims and adjustments within the timely filing limits described in this chapter.
- To ensure timely processing, claims and adjustments must be mailed to Claims Processing.
Reasons for Return or Denial: Missing Medicare EOMB
How to Prevent Returned or Denied Claims:
- All denied Medicare crossover claims must have an Explanation of Medicare Benefits (EOMB) with denial reason codes attached, and be billed to Montana Healthcare Programs on paper.
Reasons for Return or Denial: Provider is not eligible during dates of services, enrollment has lapsed due to licensing requirements, or provider number terminated
How to Prevent Returned or Denied Claims:
- Out-of-state providers must update licensure for Montana Healthcare Programs enrollment early to avoid denials. If enrollment has lapsed due to expired licensure, claims submitted with a date of service after the expiration date will be denied until the provider updates his or her enrollment.
- New providers cannot bill for services provided before Montana Healthcare Programs enrollment begins.
- If a provider is terminated from the Montana Healthcare Programs program, claims submitted with a date of service after the termination date will be denied.
- After updating his/her license, the claims that have been denied must be resubmitted by the provider.
Reasons for Return or Denial: Procedure is not allowed for provider type
How to Prevent Returned or Denied Claims:
- Provider is not allowed to perform the service.
- Verify the procedure code is correct using current HCPCS and CPT coding books.
- Check the appropriate Montana Healthcare Programs fee schedule to verify the procedure code is valid for your provider type.
Other Programs
The information in this chapter also applies to those services covered under the Mental Health Services Plan (MHSP).
End of Billing Procedures Chapter
Remittance Advices and Adjustments
The Remittance Advice
The remittance advice is the best tool providers have to determine the status of a claim. Remittance advices accompany payment for services rendered. The remittance advice provides details of all transactions that have occurred during the previous remittance advice cycle. Each line represents all or part of a claim and explains whether the claim or service has been paid, denied, or suspended/pending. If the claim was suspended or denied, the remittance advice also shows the reason.
Remittance advices are available electronically through the Montana Access to Health (MATH) web portal. To access the web portal and receive electronic remittance advices, providers must first complete an EDI Provider Enrollment Form and an EDI Trading Partner Agreement, and then register for the web portal.
Each provider must complete an EDI Trading Partner Agreement, but if there are several providers in one location who are under one tax ID number, they can use one submitter number. These providers should enter the submitter ID in both the provider number and submitter ID fields. Otherwise, enter the provider number in the provider number field.
After the forms have been processed, the provider receives a user ID and password to use to log into the MATH web portal. The verification process also requires a provider ID, a submitter ID, and a tax ID number.
Remittance advices are available in PDF format. Providers can read, print, or download PDF files using PDF reader software available online. Due to space limitations, each remittance advice is only available for 90 days. The remittance is divided into the following sections:
Remittance Advice Notice
This section is on the first page of the remittance advice. It contains important messages about rate changes, revised billing procedures, and many other items that may affect providers and claims.
Remittance advices are available for only 90 days on the web portal.
Paid Claims
This section shows claims paid during the previous cycle. It is the provider’s responsibility to verify that claims were paid correctly. If Montana Healthcare Programs overpays a claim and the problem is not corrected, it may result in an audit and the provider having to return the overpayment plus interest. If a claim was paid at the wrong amount or with incorrect information, the claim must be adjusted. (See the Adjustments section later in this chapter.)
Denied Claims
This section shows claims denied during the previous cycle. If a claim has been denied, refer to the Reason/Remark column. The Reason and Remark Code description explains why the claim was denied and is located at the end of the remittance advice. See the section titled The Most Common Billing Errors and How to Avoid Them in the Billing Procedures chapter.
Pending Claims
All claims that have not reached final disposition will appear in this area of the remittance advice (pended claims are not available on X12 835 transactions). The remittance advice uses suspended and pending interchangeably. They both mean that the claim has not reached final disposition. If a claim is pending, refer to the Reason/Remark Code column. The Reason and Remark Code description located at the end of the remittance advice explains why the claim is suspended. This section is informational only and no action should be taken on claims displayed here. Processing continues until each claim is paid or denied.
Claims shown as pending with reason code 133 require additional review before a decision to pay or deny is made. If a claim is being held while waiting for member eligibility information, it may be suspended for a maximum of 30 days. If Montana Healthcare Programs receives eligibility information within the 30-day period, the claim will continue processing. If no eligibility information is received within 30 days, the claim will be denied. When a claim is denied for lack of eligibility, the provider should verify that the correct Montana Healthcare Programs ID number was billed. If the ID number was incorrect, resubmit the claim with the correct ID number.
Credit Balance Claims
Credit balance claims are shown in this section until the credit has been satisfied.
Gross Adjustments
Any gross adjustments performed during the previous cycle are shown in this section.
Reason and Remark Code Description
This section lists the reason and remark codes that appear throughout the remittance advice with a brief description of each.
Credit Balance Claims
Credit balances occur when claim adjustments reduce original payments causing the provider to owe money to the Department. These claims are considered in process and continue to appear on the remittance advice until the credit has been satisfied. Credit balances can be resolved in two ways:
- By working off the credit balance. Remaining credit balances can be deducted from future claims. These claims will continue to appear on consecutive remittance advices until the credit has been paid.
- By sending a check payable to DPHHS for the amount owed. This method is required for providers who no longer submit claims to Montana Healthcare Programs. Please attach a note stating that the check is to pay off a credit balance and include your provider number. Send the check to the attention of the Third Party Liability unit.
Rebilling and Adjustments
Rebillings and adjustments are important steps in correcting any billing problems providers may experience. Knowing when to use the rebilling process versus the adjustment process is important.
Timeframe for Rebilling or Adjusting a Claim
Providers may resubmit, modify, or adjust any initial claim within the timely filing limits described in the Billing Procedures chapter.
The time periods do not apply to overpayments that the provider must refund to the Department. After the 12-month time period, a provider may not refund overpayments to the Department by completing a claim adjustment. The provider may refund overpayments by issuing a check or requesting a gross adjustment be made.
Rebilling Montana Healthcare Programs
Rebilling is when a provider submits a claim to Montana Healthcare Programs that was previously submitted for payment but was either returned or denied. Claims are often returned to the provider before processing because key information such as Montana Healthcare Programs provider number or authorized signature and date are missing or unreadable. For tips on preventing returned or denied claims, see the Billing Procedures chapter in this manual.
When to Rebill Montana Healthcare Programs
- Claim Denied. Providers may rebill Montana Healthcare Programs when a claim is denied. Check the reason and remark codes, make the appropriate corrections and resubmit the claim. Do not attempt to adjust denied claims.
- Line Denied. When an individual line is denied on a multiple-line claim, correct any errors and rebill Montana Healthcare Programs. For CMS-1500 claims, do not use an adjustment form. In the case of a UB-04, the line should be adjusted rather than rebilled. (See the Adjustments section.)
- Claim Returned. Rebill Montana Healthcare Programs when the claim is returned under separate cover. Occasionally, Montana Healthcare Programs is unable to process the claim and will return it to the provider with a letter stating that additional information is needed to process the claim. Correct the information as directed and resubmit the claim.
How to Rebill
- Check any reason and remark code listed and make corrections on a copy of the claim, or produce a new claim with the correct information.
- When making corrections on a copy of the claim, remember to line out or omit all lines that have already been paid.
- Submit insurance information with the corrected claim.
Adjustments
If a provider believes that a claim has been paid incorrectly, the provider may call Provider Relations. Once an incorrect payment has been verified, the provider should submit an Individual Adjustment Request form to Provider Relations. If incorrect payment was the result of a Conduent keying error, contact Provider Relations.
When adjustments are made to previously paid claims, the Department recovers the original payment and issues appropriate repayment. The result of the adjustment appears on the provider’s remittance advice as two transactions. The original payment will appear as a credit transaction. The replacement claim reflecting the corrections will be listed as a separate transaction and may or may not appear on the same remittance as the credit transaction. The replacement transaction will have nearly the same ICN number as the credit transaction, except the 12th digit will be a 2, indicating an adjustment. Adjustments are processed in the same time frame as claims.
When to Request an Adjustment
- Request an adjustment when the claim was overpaid or underpaid.
- Request an adjustment when the claim was paid but the information on the claim was incorrect (e.g., member ID, provider number, date of service, procedure code, diagnoses, units).
- Request an adjustment when an individual line is denied on a multiple-line UB-04 claim. The denied service must be submitted as an adjustment rather than a rebill.
How to Request an Adjustment
To request an adjustment, use the Individual Adjustment Request form available on the Forms page of the website. Requirements for adjusting a claim are:
- Adjustments can only be submitted on paid claims; denied claims cannot be adjusted.
- Claims Processing must receive individual claim adjustments within 12 months from the date of service. (See the Timely Filing section in the Billing Procedures chapter in this manual.) After this time, gross adjustments are required.
- Use a separate adjustment request form for each ICN.
- If correcting more than one error per ICN, use only one adjustment request form, and include each error on the form.
- If more than one line of the claim needs to be adjusted, indicate which lines and items need to be adjusted in the Remarks section.
Completing an Adjustment Request Form
- Download the Individual Adjustment Request form from the Provider Information website. Complete Section A with provider and member information and the claim’s ICN (see following table).
- Complete Section B with information about the claim. Remember to fill in only the items that need to be corrected (see following table):
- Enter the date of service or the line number in the Date of Service or Line Number column.
- Enter the information from the claim form that was incorrect in the Information on Statement column.
- Enter the correct information in the Corrected Information column.
- Attach copies of the remittance advice and a corrected claim if necessary.
- If the original claim was billed electronically, a copy of the remittance advice will suffice.
- If the remittance advice is electronic, attach a screen print of it.
- Verify the adjustment request has been signed and dated.
- Send the adjustment request to Claims Processing.
- If an original payment was an underpayment by Montana Healthcare Programs, the adjustment will result in the provider receiving the additional payment amount allowed.
- If an original payment was an overpayment by Montana Healthcare Programs, the adjustment will result in recovery of the overpaid amount from the provider. This can be done in two ways, by the provider issuing a check to the Department, or by maintaining a credit balance until it has been satisfied with future claims. (See Credit Balance earlier in this chapter.)
- Direct questions regarding claims or adjustments to Provider Relations.
Completing an Individual Adjustment Request Form
Section A
Field: 1. Provider Name and Address
Description: Provider’s name and address (and mailing address if different).
Field: 2. Name
Description: The member’s name
Field: 3. Internal Control Number (ICN)
Description: There can be only one ICN per Adjustment Request Form. When adjusting a claim that has been previously adjusted, use the ICN of the most-recent claim.
Field: 4. Provider number
Description: The provider’s NPI/API.
Field: 5. Member Montana Healthcare Programs Number
Description: Member’s Montana Healthcare Programs ID number.
Field: 6. Date of Payment
Description: Date claim was paid.
Field: 7. Amount of Payment
Description: The amount of payment from the remittance advice.
Section B
Field: 1. Units of Service
Description: If a payment error was caused by an incorrect number of units, complete this line.
Field: 2. Procedure Code/NDC Revenue Code
Description: If the procedure code, NDC, or revenue code are incorrect, complete this line.
Field: 3. Dates of Service (DOS)
Description: If the date of service is incorrect, complete this line.
Field: 4. Billed Amount
Description: If the billed amount is incorrect, complete this line.
Field: 5. Personal Resource (Nursing Facility)
Description: If the member’s personal resource amount is incorrect, complete this line.
Field: 6. Insurance Credit Amount
Description: If the member’s insurance credit amount is incorrect, complete this line.
Field: 7. Net (Billed - TPL or Medicare Paid)
Description: If the payment error was caused by a missing or incorrect insurance credit, complete this line. Net is billed amount minus the amount TPL or Medicare paid.
Field: 8. Other/Remarks
Description: If none of the above items apply, or if unsure what caused the payment error, complete this line.
Mass Adjustments
Mass adjustments are done when it is necessary to reprocess multiple claims. They generally occur when:
- Montana Healthcare Programs has a change of policy or fees that is retroactive. In this case federal laws require claims affected by the changes to be mass adjusted.
- A system error that affected claims processing is identified.
Providers are informed of mass adjustments on the first page of the remittance advice, the monthly Claim Jumper, or provider notices. Mass adjustment claims shown on the remittance advice have an ICN that begins with a 4.
Payment and the Remittance Advice
Montana Healthcare Programs payment and remittance advices are available weekly. Payment is via electronic funds transfer (EFT). Direct deposit is another name for EFT. The electronic remittance advices (ERAs) are available on the web portal for 90 days.
With EFT, the Department deposits the funds directly to the provider’s financial institution account. Holidays may delay payments until the next business day.
Other Programs
The information in this chapter also applies to the Mental Health Services Plan (MHSP), and Healthy Montana Kids (HMK) dental and eyeglasses benefits.
End of Remittance Advice and Adjustments Chapter
Appendix A: Forms
The forms listed below and others are available on the Forms page of the Montana Healthcare Programs Provider Information website. See the left menu on https://medicaidprovider.mt.gov.
- Presumptive Eligibility Notice of Decision
- Montana Healthcare Programs Incurment Notice
- Montana Healthcare Programs Form Order
- Individual Adjustment Request Form
- Paperwork Attachment Cover Sheet
- Provider Address Correction Form
- Blanket Denial
End of Appendix A: Forms Chapter
Appendix B: Place of Service Codes
End of Appendix B: Place of Service Codes Chapter
Appendix C: County Offices of Public Assistance
See the DPHHS webpage https://dphhs.mt.gov/hcsd/OfficeofPublicAssistance.
End of Appendix C: County Offices of Public Assistance Chapter
Definitions and Acronyms
End of Definitions and Acronyms Chapter
Index
Previous editions of this manual contained an index.
This edition has three search options.
- Search the whole manual. Open the Complete Manual pane. From your keyboard press the Ctrl and F keys at the same time. A search box will appear. Type in a descriptive or key word (for example "Denials". The search box will show all locations where denials discussed in the manual.
- Search by Chapter. Open any Chapter tab (for example the "Billing Procedures" tab). From your keyboard press the Ctrl and F keys at the same time. A search box will appear. Type in a descriptive or key word (for example "Denials". The search box will show where denials discussed in just that chapter.
- Site Search. Search the manual as well as other documents related to a particular search term on the Montana Healthcare Programs Site Specific Search page.
End of Index Chapter
End of General Information for Providers Manual
Update Log
Publication History
This publication supersedes all versions of previous general information provider handbooks. This publication is to be used conjunction with provider type manuals. Published by the Montana Department of Public Health & Human Services, February 2002.
Updated September 2002, October 2003, September 2004, November 2004, April 2005, April 2008, February 2012, April 2012, June 2014, July 2014, September 2014, November 2014, August 2015, November 2015, January 2016, July 2016, August 2016, February 2017, September 2017,November 2017, April 2018, June 2018, May 2019, November 2019 ,January 2020, and February 2020.
CPT codes, descriptions and other data only are copyright 1999 American Medical Association (or such other date of publication of CPT). All Rights Reserved. Applicable FARS/DFARS Apply.
Update Log
02/20/2020
SURS and Billing Procedures chapters updated to include acceptable minutes for billing a 15 minute unit of service.
01/01/2020
- Cost Share references removed from the Provider Requirements, Member Eligibility and Responsibility, and Billing Procedures Chapters.
- Term "Medicaid" replaced with "Montana Healthcare Programs" throughout the manual.
- Terms "client" and "patient" replaced with "member".
11/18/2019
The EPSDT Well-Child Chapter language was updated to included current age, rule, and service information.
05/03/2019
The Provider Requirements Chapter was revised to include rule language for usual and customary billing practices. The Billing Procedures Chapter was revised to included updated NDC information.
06/04/2018
Removed commercial resource references.
04/30/2018
The Outpatient Clinic Services section of the Billing Procedure Chapter was updated to include current provider-based clinic status.
11/24/2017
The Billings Procedure chapter was updated with current electronic submission information.
09/21/2017
General Information for Providers Manual converted to an HTML format and adapted to 508 Accessibility Standards. An additional paragraph was added under the EPSDT Well Child chapter regarding caregiver depression screening coverage. Language was changed regarding manual maintenance in the Introduction chapter.
02/06/2017
In summary, the Telemedicine Chapter was added as a new chapter. And the Medically Needy section of the Member Responsibilities Chapter page 6.5 was updated.
08/02/2016
The Introduction contains updated links in the HELP section.
Cost Share was updated in the Billings Procedure.
A duplicate word was removed in the RA chapter.
The Cover Page was changed to reflect the current date of the new General Manual revision.
01/01/2020
- Cost Share references removed from the Provider Requirements, Member Eligibility and Responsibilities, and Billing Procedures Chapters.
- Term "Medicaid" replaced with "Montana Healthcare Programs" throughout the manual.
- Terms "client" and "patient" replaced with "member".
07/12/2016
General Information For Providers, July 2016
Table of Contents was amended by changing the title of “Basic Medicaid Waiver” to “Waiver for Additional Services and Populations (formerly Basic Medicaid Waiver)”.
Index was amended by changing the title of “Basic Medicaid Waiver” to “Waiver for Additional Services and Populations (formerly Basic Medicaid Waiver)”.
Page 1.3 changed the title “Basic Medicaid Waiver for Additional Services and Populations” to “Waiver for Additional Services and Populations (formerly Basic Medicaid Waiver)”
01/19/2016
General Information for Providers, January 2016: Introduction Regarding HELP Plan Information
01/15/2016
General Information for Providers, January 2016: Introduction Regarding HELP Plan Information
12/31/2015
General Information for Providers, January 2016: HELP Plan-Related Updates and Others
11/17/2015
General Information for Providers, November 2015: Billing Procedures, Revenue Codes 25X and 27X
07/31/2015
General Information for Providers, August 2015: Entire Manual
11/19/2014
General Information for Providers, November 2014: Billing Procedures
10/08/2014
General Information for Providers, September 2014: Billing Procedures
07/22/2014
General Information for Providers, July 2014: Member Eligibility and Responsibilities
06/30/2014
General Information for Providers, June 2014: General Information for Providers
If information is found on the website, it has been removed from the manual, and a link to the source is provided.
04/13/2012
General Information for Providers, April 2012: Medicaid Covered Services and Member Eligibility
End of Update Log Chapter
Table of Contents
Key Contacts and Key Websites
Introduction
Rule References
Manual Organization
Manual Maintenance
Website Information
Provider Training Opportunities
Contract Services
Standard Montana Healthcare Programs
- Standard Montana Healthcare Programs Benefits
- Waiver for Additional Services and Populations (formerly Basic Montana Healthcare Programs Waiver)
- Montana Healthcare Programs Expansion Benefits
Other Programs
- Chemical Dependency Bureau State Paid Substance Dependency/Abuse Treatment Programs
- Children’s Mental Health Bureau Non-Montana Healthcare Programs Services
- Children’s Special Health Services (CSHS)
- Health Insurance Premium Payment (HIPP)
- Healthy Montana Kids (HMK)
- Mental Health Services Plan (MHSP)
- Plan First
Provider Requirements
Provider Enrollment
- Enrollment Materials
- Montana Healthcare Programs Renewal
- Changes in Enrollment
- Change of Ownership
- Electronic Claims
- Terminating Montana Healthcare Programs Enrollment
Authorized Signature (ARM 37.85.406)
Provider Rights
Administrative Reviews and Fair Hearings (ARM 37.5.310)
Provider Participation (ARM 37.85.401)
- Accepting Montana Healthcare Programs Members (ARM 37.85.406)
- Non-Discrimination (ARM 37.85.402)
- Montana Healthcare Programs Payment Is Payment in Full (ARM 37.85.406)
- Payment Return (ARM 37.85.406)
- Disclosure
- Member Services
- Confidentiality (ARM 37.85.414)
- Record Keeping (ARM 37.85.414)
- Compliance with Applicable Laws, Regulations, and Policies
Provider Sanctions (ARM 37.85.501–507 and ARM 37.85.513)
Other Programs
EPSDT Well-Child
Who Can Provide EPSDT Screenings?
The Well-Child Screen
- Initial/Interval History
- Developmental Assessments
- Nutritional Screen
- Unclothed Physical Inspection
- Vision Screen
- Hearing Screen
- Autism Screen
- Critical Congenital Heart Defect Screen
- Laboratory Tests
- Immunizations
- Dental Screen
- Discussion and Counseling/Anticipatory Guidance
Prior Authorization
What Is Prior Authorization?
Telemedicine
Program Overview
When to Use Telemedicine
Telemedicine Confidentiality Requirements
General Billing Instructions
Originating Provider Requirements
Distance Provider Requirements
Member Eligibility and Responsibilities
Verifying Member Eligibility
- Member without Card
- Newborns
Inmates in Public Institutions (ARM 37.82.1321)
Presumptive Eligibility
Retroactive Eligibility
Coverage for the Medically Needy
Nurse First
Montana Breast and Cervical Cancer Treatment Program
When a Member Has Other Coverage
- Identifying Additional Coverage
When a Member Has Medicare
- Medicare Part A Claims
- Medicare Part B Crossover Claims
When a Member Has TPL (ARM 37.85.407)
- Exceptions to Billing Third Party First
- Requesting an Exemption
- When the Third Party Pays or Denies a Service
- When the Third Party Does Not Respond
- Coordination Between Medicare and Montana Healthcare Programs
- Members with Other Sources of Coverage
- The Health Insurance Premium Payment (HIPP) Program
- Indian Health Service (IHS)
- Crime Victims
When Members Are Uninsured
Member Responsibilities
Other Programs
- Chemical Dependency Bureau State Paid Substance Dependency/Abuse Treatment Program (CDB-SPSDATP)
- Healthy Montana Kids (HMK)
- Mental Health Services Plan (MHSP)
- Plan First
Surveillance and Utilization Review
Surveillance and Utilization Review (42 CFR 456)
Key Points
Billing Tips
Billing Procedures
Claim Forms
Timely Filing Limits (ARM 37.85.406)
- Tips to Avoid Timely Filing Denials
When to Bill Montana Healthcare Programs Members (ARM 37.85.406)
Member Co-Payment (ARM 37.85.204)
Billing for Members with Other Insurance
Billing for Retroactively Eligible Members
Coding Tips
Number of Lines on Claim
Multiple Services on Same Date
Span Bills
Reporting Service Dates
Using Modifiers
Billing Tips for Specific Services
- Abortions
- Drugs and Biologicals
- Lab Services
Outmember Clinic Services
Partial Hospitalization
- Sterilization/Hysterectomy (ARM 37.86.104)
- Supplies
Submitting a Claim
- Paper Claims
- Electronic Claims
- Billing Electronically With Paper Attachments
Claim Inquiries
The Most Common Billing Errors and How to Avoid Them
Other Programs
Remittance Advices and Adjustments
The Remittance Advice
- Remittance Advice Notice
- Paid Claims
- Denied Claims
- Pending Claims
- Credit Balance Claims
- Gross Adjustments
- Reason and Remark Code Description
Credit Balance Claims
Rebilling and Adjustments
- Timeframe for Rebilling or Adjusting a Claim
- Rebilling Montana Healthcare Programs
- When to Rebill Montana Healthcare Programs
- How to Rebill
- Adjustments
- When to Request an Adjustment
- How to Request an Adjustment
- Completing an Adjustment Request Form
- Mass Adjustments
Payment and the Remittance Advice
Other Programs
Appendix A: Forms
Appendix B: Place of Service Codes
Appendix C: Local Offices of Public Assistance
Definitions and Acronyms
Index
End of Table of Contents Chapter
Key Contacts and Key Websites
End of Key Contacts and Key Websites Chapter
Introduction
The Montana Healthcare Programs program plays an essential role in providing health insurance for Montanans. Before the enactment of Medicare and Montana Healthcare Programs, healthcare for the elderly and the indigent was provided through a patchwork of programs sponsored by governments, charities, and community hospitals.
Today, Medicare is a federal program that provides insurance for persons aged 65 and over and for people with severe disabilities, regardless of income. Montana Healthcare Programs provides healthcare coverage to specific populations, especially low-income families with children, pregnant women, disabled people, and the elderly. Montana Healthcare Programs is administered by state governments under broad federal guidelines. Recent healthcare laws have greatly increased the number of people who qualify for Montana Healthcare Programs. See the Montana Healthcare Programs Program: Report to the 2017 Legislature.
Rule References
Providers must be familiar with current rules and regulations governing the Montana Healthcare Programs program. The provider manuals are meant to assist providers in billing Montana Healthcare Programs; they do not contain all Montana Healthcare Programs rules and regulations.
Rule citations in the text are a reference tool; they are not a summary of the entire rule. In the event that a manual conflicts with a rule, the rule prevails. Links to rules are available online on the provider type pages on the Provider Information website or at http://www.sos.mt.gov/ARM/index.asp.
Providers can order the Administrative Rules of Montana, including individual titles, online or by mail, through the Secretary of State website. Select the How to Order option in the Additional Resources section.
Manual Organization
The General Information for Providers manual provides answers to general Montana Healthcare Programs questions about provider enrollment, member eligibility, and surveillance and utilization review.
This manual is designed to work with Montana Healthcare Programs provider type manuals, which contain program information on covered services, prior authorization, and billing for specific services.
It is divided by chapters, and a table of contents and index allow providers to find answers to most questions. The margins contain important information and space for writing notes. For eligibility and coordination of benefit information, see the Member Eligibility and Responsibilities chapter in this manual. Provider-specific information is in provider type manuals. Contact Provider Relations at 1-800-624-3958 with questions.
Manual Maintenance
Manuals must be kept current.
Notification of manual updates are provided through the weekly web postings under “Recent Website Posts” on the home page of the provider website and under Provider Notices on the provider type page of the provider website. Older versions of the manual may be found through the Archive page on the Provider website. Printing the manual material found at this website for long-term use is not advisable. Department Policy material is updated periodically and it is the responsibility of the users to check and make sure that the policy they are researching or applying has the correct effective date for their circumstances.
Website Information
Additional information is available through the Provider Information website.
Providers can stay informed with the latest Montana Healthcare Programs news and events, download provider manuals/replacement pages, provider notices, fee schedules, newsletters, and forms. Other resources are also available. See the menu for links.
Provider Training Opportunities
Montana Healthcare Programs offers a variety of training opportunities that are announced on the Provider Information website and in the Claim Jumper newsletter. Recorded training sessions are available on the Training page of the website.
Contract Services
Montana Healthcare Programs works with various contractors who represent Montana Healthcare Programs through the services they provide. While it is not necessary for providers to know contractor duties, the information below is provided as informational.
- Conduent State Healthcare, LLC. Answers provider inquiries and enrolls providers in Montana Healthcare Programs and Passport to Health; processes claims for Montana Healthcare Programs, MHSP, HMK, pharmacy, dental, and eyeglasses, and HELP claims listed in the HELP Plan section.
- Mountain-Pacific Quality Health. Provides prior authorization for many Montana Healthcare Programs services.
- Magellan Montana Healthcare Programs Administration (dba First Health Services). Provides prior authorization, utilization review, and continued stay review for some mental health services.
Standard Montana Healthcare Programs
Standard Montana Healthcare Programs Benefits
All Montana Healthcare Programs members are eligible for Standard Montana Healthcare Programs services if medically necessary. Covered services include, but are not limited to, audiology services, clinic services, community health centers services, dental services, doctor visits, hospital services, immunizations, Indian Health Services, laboratory services, mental health services, Nurse First services, nursing facility, occupational therapy, pharmacy, public health clinic services, substance dependency services, tobacco cessation, transportation, vision services, well-child checkups, and x-rays.
Waiver for Additional Services and Populations (formerly Basic Montana Healthcare Programs Waiver)
This waiver includes individuals age 18 or older, with Severe Disabling Mental Illnesses (SDMI) who qualify for or are enrolled in the state-financed Mental Health Services Plan (MHSP), but are otherwise ineligible for Montana Healthcare Programs benefits and either have:
- Income 0–138% of the federal poverty level (FPL) and are eligible for or enrolled in Medicare; or
- Income 139–150% of the FPL regardless of Medicare status (they can be covered or not covered by Medicare and be eligible).
Members covered under this waiver receive Standard Montana Healthcare Programs benefits. To apply or for more information, contact the Addictive and Mental Disorders Division at 1-406-444-2878 or visit the BHDD website.
HELP Plan Benefits
The Montana Health and Economic Livelihood Partnership (HELP) Plan provides health coverage to adults ages 19–64 with incomes up to 138% of the FPL; who are not enrolled or eligible for Medicare; who are not incarcerated; and who are U.S. citizens or documented, qualified aliens who are Montana residents.
Most services will be administered through Blue Cross and Blue Shield of Montana (BCBSMT), a third party administrator, and some services will be administered through Conduent.
Services for the HELP Plan Processed by BCBSMT Most medical and behavior health services will be processed by BCBSMT, including:
- Behavioral Health (Mental Health and Substance Use Disorder)
- Convalescent Home (excludes Custodial Care)
- Durable Medical Equipment/Supplies
- Early and Periodic Screening, Diagnostic, and Treatment (EPSDT)
- Emergency
- Hospital
- Lab and X-Ray (Medical)
- Medical Vision and Exams
- Mid-Level
- Physician
- Preventive
- Rehabilitative and Habilitative
- Surgical
Services for the HELP Plan Processed by Conduent
- Audiology
- Dental
- Diabetes Prevention Program
- Eyeglasses
- Federally Qualified Health Center
- Hearing Aids
- Home Infusion
- Indian Health Services/Tribal Health
- Pharmacy
- Rural Health Clinic
- Transportation
Contact Information
• HELP Plan Provider Services 1 (877) 296-8206 (BCBSMT)
• BCBSMT website http://www.bcbsmt.com/mthelpplan
• HELP Plan Provider Services 1 (800) 624-3958 (Conduent)
• Provider Information website https://medicaidprovider.mt.gov
• HELP Plan Information website https://dphhs.mt.gov/healthcare
Other Programs
In addition to Montana Healthcare Programs, the Department of Public Health and Human Services (DPHHS, the Department) offers other programs. In addition to those listed below, other subsidized health insurance plans may be available from programs funded by the federal government or private organizations.
Chemical Dependency Bureau State Paid Substance Dependency/Abuse Treatment Programs
For individuals who are ineligible for Montana Healthcare Programs and whose family income is within program standards. For more information on these programs, call 406-444-3964 or visit https://dphhs.mt.gov/BHDD/SubstanceAbuse/index.
Children’s Mental Health Bureau Non-Montana Healthcare Programs Services
Funding sources for short-term use, not entitlement programs. Planning efforts toward family reunification are the primary objective, with transition planning essential for youth in out-of-home care. For information, call 406-444-4545, or refer to the Non-Montana Healthcare Programs Services Provider Manual at https://dphhs.mt.gov/BHDD/cmb/Manuals.
Children’s Special Health Services (CSHS)
A program that assists children with special healthcare needs who are not eligible for Montana Healthcare Programs by paying medical costs, finding resources, and conducting clinics. For more information, call 406-444-3622 (local) or 800-762-9891 (toll-free in Montana) or visit https://dphhs.mt.gov/ecfsd/cshs/index.
Health Insurance Premium Payment (HIPP)
A program that allows Montana Healthcare Programs funds to be used to pay for private health insurance coverage when it is cost effective to do so. Visit https://dphhs.mt.gov/MontanaHealthcarePrograms/HIPP.
Healthy Montana Kids (HMK)
HMK offers low-cost or free health insurance for low-income children younger than 19. Children must be uninsured U.S. citizens or qualified aliens, Montana residents who are not eligible for Montana Healthcare Programs. Visit https://dphhs.mt.gov/HMK.
Mental Health Services Plan (MHSP)
A program for adults who are ineligible for Montana Healthcare Programs and whose family income is within program standards. Visit https://dphhs.mt.gov/BHDD/mentalhealthservices/index.
Plan First
If a member loses Montana Healthcare Programs, family planning services may be paid by Plan First, which is a separate Montana Healthcare Programs program that covers family planning services for eligible women. Some of the services covered include office visits, contraceptive supplies, laboratory services, and testing and treatment of sexually transmitted diseases (STDs). Visit https://dphhs.mt.gov/MontanaHealthcarePrograms/PlanFirst.
End of Introduction Chapter
Provider Requirements
Provider Enrollment
To be eligible for enrollment, a provider must:
- Provide proof of licensure, certification, accreditation, or registration according to Montana state laws and regulations.
- Provide a completed W-9.
- Meet the conditions in this chapter and in program instructions regulating the specific type of provider, program, and/or service.
Providers must complete a Montana Healthcare Programs Provider Enrollment Form, which is a contract between the provider and the Department. Healthcare providers must have a National Provider Identifier (NPI) or atypical provider identifier (API), which should be used in all correspondence with Montana Healthcare Programs. Providers must enroll for each type of service they provide. For example, a pharmacy that also sells durable medical equipment (DME) must enroll for the pharmacy and again for DME.
Montana Healthcare Programs payment is made only to enrolled providers.
Enrollment Materials
Each newly enrolled provider is sent an enrollment letter confirming enrollment. The letter includes instructions for obtaining additional information from the Provider Information website.
Letters to atypical providers include their API.
Montana Healthcare Programs-related forms are available on the Provider Information website. However, providers must order CMS-1500, UB-04, and dental claim forms from an authorized vendor.
Out-of-state providers can avoid denials and late payments by renewing Montana Healthcare Programs enrollment early.
Montana Healthcare Programs Renewal
For continued Montana Healthcare Programs participation, providers must maintain a valid license or certificate. For Montana providers, licensure or certification is automatically verified and enrollment renewed each year. If licensure or certification cannot be confirmed, the provider is contacted. Out-of-state providers are notified when Montana Healthcare Programs enrollment is about to expire. To renew enrollment, providers should mail or fax a copy of their license or certificate to Provider Relations. See the Contact Us link on the Provider Information website.
Changes in Enrollment
Changes in address, telephone/fax, name, ownership, legal status, tax ID, or licensure must be submitted in writing to Provider Relations. Faxes are not accepted because the provider’s original signature and NPI (healthcare providers) or API (atypical providers) are required. For change of address, providers can use the form on the website; for a physical address change, providers must include a completed W-9 form.
To avoid payment delays, notify Provider Relations of an address change in advance.
Change of Ownership
When ownership changes, the new owner must re-enroll in Montana Healthcare Programs. For income tax reporting purposes, the provider must notify Provider Relations at least 30 days in advance about any changes to a tax identification number. Early notification helps avoid payment delays and claim denials.
Electronic Claims
Providers who submit claims electronically experience fewer errors and quicker payment. For more information on electronic claims submission options, see the Electronic Claims section in the Billing Procedures chapter in this manual.
Terminating Montana Healthcare Programs Enrollment
Montana Healthcare Programs enrollment may be terminated by writing to Provider Relations; however, some provider types have additional requirements. Providers should include their NPI (healthcare providers) or API (atypical providers) and the termination date in the letter. The Department may also terminate a provider’s enrollment under the following circumstances:
- Breaches of the provider agreement.
- Demonstrated inability to perform under the terms of the provider agreement.
- Failure to abide by applicable Montana and U.S. laws.
- Failure to abide by the regulations and policies of the U.S. Department of Health and Human Services or the Montana Healthcare Programs program.
Authorized Signature (ARM 37.85.406)
All correspondence and claim forms submitted to Montana Healthcare Programs must have an NPI (healthcare providers) or API (atypical providers) and an authorized signature. The signature may belong to the provider, billing clerk, or office personnel, and may be handwritten, typed, stamped, or computer-generated. When a signature is from someone other than the provider, that person must have written authority to bind and represent the provider for this purpose. Changes in enrollment information require the provider’s original signature.
Provider Rights
- Providers have the right to end participation in Montana Healthcare Programs in writing at any time; however, some provider types have additional requirements.
- Providers may bill Montana Healthcare Programs members when the conditions are met outlined in ARM 37.85.204.
- Providers may bill Montana Healthcare Programs members for services not covered by Montana Healthcare Programs if the provider and member have agreed in writing prior to providing services.
- When the provider does not accept the member as a Montana Healthcare Programs member, a specific custom agreement is required stating that the member agrees to be financially responsible for the services received.
- A provider may bill a member for non-covered services if the provider has informed the member in advance of providing the services that Montana Healthcare Programs will not cover the services and that the member will be required to pay privately for the services, and if the member has agreed to pay privately for the services. Non-covered services are services that may not be reimbursed for the particular member by the Montana Healthcare Programs program under any circumstances and covered services are services that may be reimbursed by the Montana Healthcare Programs program for the particular member if all applicable requirements, including medical necessity, are met (ARM 37.85.406).
- Providers have the right to choose Montana Healthcare Programs members, subject to the conditions in Accepting Montana Healthcare Programs Members later in this chapter.
- Providers have the right to request administrative reviews and fair hearings for a Department action that adversely affects the provider’s rights or the member’s eligibility (ARM 37.85.411).
Administrative Reviews and Fair Hearings (ARM 37.5.310)
A provider may request an administrative review if he/she believes the Department has made a decision that fails to comply with applicable laws, regulations, rules, or policies.
To request an administrative review, state in writing the objections to the Department’s decision and include substantiating documentation for consideration in the review. The request must be addressed to the division that issued the decision and delivered (or mailed) to the Department. The Department must receive the request within 30 days from the date the Department’s contested determination was mailed. Providers may request extensions in writing within this 30 days. See the Contact Us link on the Provider Information website.
If the provider is not satisfied with the administrative review results, a fair hearing may be requested. Fair hearing requests must contain concise reasons the provider believes the Department’s administrative review determination fails to comply with applicable laws, regulations, rules, or policies. This document must be signed and received by the Fair Hearings Office within 30 days from the date the Department mailed the administrative review determination. A copy must be delivered or mailed to the division that issued the determination within 3 working days of filing the request.
Provider Participation (ARM 37.85.401)
By enrolling in the Montana Healthcare Programs program, providers must comply with all applicable state and federal statutes, rules, and regulations, including but not limited to, federal regulations and statutes found in Title 42 of the Code of Federal Regulations and the United States Code governing the Montana Healthcare Programs program and all applicable Montana statutes and rules governing licensure and certification.
Accepting Montana Healthcare Programs Members (ARM 37.85.406)
Institutional providers, eyeglass providers, and non-emergency transportation providers may not limit the number of Montana Healthcare Programs members they will serve. Institutional providers include nursing facilities, skilled care nursing facilities, intermediate care facilities, hospitals, institutions for mental disease, inpatient psychiatric hospitals, and residential treatment facilities.
Other providers may limit the number of Montana Healthcare Programs members. They may also stop serving private-pay members who become eligible for Montana Healthcare Programs. Any such decisions must follow these principles:
- No member should be abandoned in a way that would violate professional ethics.
- Members may not be refused service because of race, color, national origin, age, or disability.
- Members enrolled in Montana Healthcare Programs must be advised in advance if they are being accepted only on a private-pay basis.
- In service settings where the member is admitted or accepted as a Montana Healthcare Programs member by a provider, facility, institution, or other entity that arranges provision of services by other or ancillary providers, all other or ancillary providers will be deemed to have accepted the individual as a Montana Healthcare Programs member and may not bill the member for the services unless, prior to provision of services, the particular provider informed the member of their refusal to accept Montana Healthcare Programs and the member agreed to pay privately for the services. See ARM 37.85.406(11)(d) for details.
- Most providers may begin Montana Healthcare Programs coverage for retroactively eligible members at the current date or from the date retroactive eligibility was effective. See the Retroactive Eligibility section in the Member Eligibility and Responsibilities chapter of this manual for details.
- When a provider bills Montana Healthcare Programs for services rendered to a member, the provider has accepted the member as a Montana Healthcare Programs member.
- Once a member has been accepted as a Montana Healthcare Programs member, the provider may not accept Montana Healthcare Programs payment for some covered services but refuse to accept Montana Healthcare Programs payment for other covered services.
Non-Discrimination (ARM 37.85.402)
Providers may not discriminate illegally in the provision of service to eligible Montana Healthcare Programs members or in employment of persons on the grounds of race, creed, religion, color, sex, national origin, political ideas, marital status, age, or disability. Providers shall comply with the Civil Rights Act of 1964 (42 USC 2000d, et seq.), the Age Discrimination Act of 1975 (42 USC 6101, et seq.), the Americans With Disabilities Act of 1990 (42 USC 12101, et seq.), section 504 of the Rehabilitation Act of 1973 (29 USC 794), and the applicable provisions of Title 49, MCA, as amended and all regulations and rules implementing the statutes.
Providers are entitled to Montana Healthcare Programs payment for diagnostic, therapeutic, rehabilitative or palliative services when the following conditions are met:
- Provider must be enrolled in Montana Healthcare Programs. (ARM 37.85.402)
- Services must be performed by practitioners licensed and operating within the scope of their practice as defined by law. (ARM 37.85.401)
- Member must be enrolled in Montana Healthcare Programs and be nonrestricted. See Member Eligibility and Responsibilities for restrictions. (ARM 37.85.415 and ARM 37.85.205)
- Service must be medically necessary. The Department may review medical necessity at any time before or after payment. (ARM 37.85.410)
- Service must be covered by Montana Healthcare Programs and not be considered cosmetic, experimental, or investigational. (ARM 37.82.102, ARM 37.85.207, and ARM 37.86.104)
- Montana Healthcare Programs and/or third party payers must be billed according to rules and instructions as described in the Billing Procedures chapter, current provider notices and manual replacement pages, and according to ARM 37.85.406 (Billing, reimbursement, claims processing and payment) and ARM 37.85.407 (third party liability).
- Charges must be usual and customary. (ARM 37.85.212 and ARM 37.85.406)
For all purposes of this rule, the amount of the provider's usual and customary charge may not exceed the reasonable charge usually and customarily charged to all payers. - ARM 37.85.406(19)
- Reimbursement to providers from Montana Healthcare Programs and all other payers may not exceed the total Montana Healthcare Programs fee. For example, if payment to the provider from all responsible parties ($75.00) is greater than the Montana Healthcare Programs fee ($70.00), Montana Healthcare Programs will pay at $0. (ARM 37.85.406)
- Claims must meet timely filing requirements. See the Billing Procedures chapter in this manual for timely filing requirements. (ARM 37.85.406)
Montana Healthcare Programs Payment Is Payment in Full (ARM 37.85.406)
Providers must accept Montana Healthcare Programs payment as payment in full for any covered service. Zero paid claims are considered paid.
Payment Return (ARM 37.85.406)
If Montana Healthcare Programs pays a claim, and then discovers that the provider was not entitled to the payment for any reason, the provider must return the payment.
Disclosure
- Providers are required to fully disclose ownership and control information when requested by the Department. (ARM 37.85.402)
- Providers are required to make all medical records available to the Department. (ARM 37.85.410 and ARM 37.85.414)
Member Services
- All services must be made a part of the medical record. (ARM 37.85.414)
- Providers must treat Montana Healthcare Programs members and private-pay members equally in terms of scope, quality, duration, and method of delivery of services unless specifically limited by regulations. (ARM 37.85.402)
Confidentiality (ARM 37.85.414)
All Montana Healthcare Programs member and applicant information and related medical records are confidential. Providers are responsible for maintaining confidentiality of healthcare information subject to applicable laws.
Record Keeping (ARM 37.85.414)
Providers must maintain all Montana Healthcare Programs-related medical and financial records for 6 years and 3 months following the date of service. The provider must furnish these records to the Department or its designee upon request. The Department or its designee may audit any Montana Healthcare Programs-related records and services at any time. Such records may include but are not limited to:
- Original prescriptions
- Certification of medical necessity
- Treatment plans
- Medical records and service reports including but not limited to:
- Member’s name and date of birth
- Date and time of service
- Name/title of person providing service (other than billing practitioner)
- Chief complaint or reason for each visit
- Pertinent medical history
- Pertinent findings on examination
- Medication, equipment, and/or supplies prescribed or provided
- Description and length of treatment
- Recommendations for additional treatments, procedures, or consultations
- X-rays, tests, and results
- Dental photographs/teeth models
- Plan of treatment and/or care, and outcome
- Specific claims and payments received for services
- Each medical record entry must be signed and dated by the person ordering or providing the service.
- Prior authorization information
- Claims, billings, and records of Montana Healthcare Programs payments and amounts received from other payers for services provided to Montana Healthcare Programs members
- Records/original invoices for items prescribed, ordered, or furnished
- Any other related medical or financial data
Compliance with Applicable Laws, Regulations, and Policies
All providers must follow all applicable rules of the Department and all applicable state and federal laws, regulations, and policies. Provider manuals are to assist providers in billing Montana Healthcare Programs; they do not contain all Montana Healthcare Programs rules and regulations. Rule citations in the text are a reference tool; they are not a summary of the entire rule. In the event that a manual conflicts with a rule, the rule prevails.
The following are references for some of the rules that apply to Montana Healthcare Programs. The provider manual for each individual program contains rule references specific to that program.
- Title XIX Social Security Act 1901 et seq.
- 42 U.S.C. 1396 et seq.
- Code of Federal Regulations (CFR)
- CFR Title 42 – Public Health
- Montana Codes Annotated (MCA)
- MCA Title 53 – Social Services and Institutions
- Administrative Rules of Montana (ARM)
- ARM Title 37 – Public Health and Human Services
Links to rules are available on the provider type pages of the Provider Information website. Paper copies of rules are available through the Secretary of State’s office.
Provider Sanctions (ARM 37.85.501–507 and ARM 37.85.513)
The Department may withhold a provider’s payment or suspend or terminate Montana Healthcare Programs enrollment if the provider has failed to abide by terms of the Montana Healthcare Programs contract, federal and state laws, regulations, and policies.
Providers are responsible for keeping informed about applicable laws, regulations, and policies.
Other Programs
Below is a list of non-Montana Healthcare Programs Department of Public Health and Human Services (DPHHS) programs.
- Chemical Dependency Bureau Substance Dependency/Abuse Treatment https://dphhs.mt.gov/BHDD/SubstanceAbuse/index
- Children’s Mental Health Bureau Non-Montana Healthcare Programs Services https://dphhs.mt.gov/BHDD/cmb/Manuals
- Health Insurance Premium Payment (HIPP) https://dphhs.mt.gov/MontanaHealthcarePrograms/HIPP
- Healthy Montana Kids (HMK) https://dphhs.mt.gov/HMK
- Mental Health Services Plan (MHSP) https://dphhs.mt.gov/BHDD/mentalhealthservices/index
- Plan First https://dphhs.mt.gov/MontanaHealthcarePrograms/PlanFirst
End of Provider Requirements Chapter
EPSDT Well-Child
The Early and Periodic Screening, Diagnostic, and Treatment (EPSDT) Services program is the federally sponsored, comprehensive healthcare benefits package for Montana Healthcare Programs-enrolled children through age 20. It helps families get early identification and treatment of medical, dental, vision, mental health, and developmental problems for their children. All Montana Healthcare Programs families are encouraged to use these services. See ARM 37.86.2201–2235.
EPSDT Well-Child Check-Ups
At the core of EPSDT is the well child visit. These regularly scheduled check-ups help your child’s primary care provider identify problems and assist with a treatment plan for your child. . By following the Bright Futures schedule of well child visits, parents can ensure their children receive the full benefit of their comprehensive health care coverage.
EPSDT Well-Child visits include:
- Comprehensive health & developmental history
- Comprehensive unclothed physical examination
- Assessment of physical, emotional & developmental health
- Immunizations appropriate to age & health history
- Laboratory tests (including blood lead levels)
- Assessment of mental/behavioral health
- Assessment of mouth, oral cavity & teeth, including referral to a dentist
- Assessment of nutritional status
- Assessment of vision, including referrals
- Assessment of overall health, including referrals
- Health education (also called anticipatory guidance)
- Family planning services and adolescent maternity care
In addition to well child visits, EPSDT includes inter-periodic sick visits, or other visits as needed by the individual child.
EPSDT Provider Resources:
Immunization Schedule - The American Academy of Pediatrics Bright Futures recommended immunization schedule for children through the age of 18.
Montana Healthcare Programs Member Guide - Learn more about Montana Healthcare Programs coverage through the Early and Periodic Screening, Diagnosis and Treatment Program at pages 30-31 in the handbook.
Bright Futures - A link to the American Academy of Pediatrics Bright Futures website.
Additional Services Under EPSDT
If a child (up to the age of 21), needs medically necessary services, outside the normal realm of covered services (non-covered, over the limit, does not meet criteria, etc), these can be approved on a case by case basis. EPSDT prior authorization requests must be submitted by a child’s primary care provider or medical specialist, within their scope of practice, who determines the child needs additional treatment, services, or supplies for a primary health condition.
These requests are reviewed and decision determinations completed within 2 weeks of receipt of all required documentation.
EPSDT Prior Authorization & Medical Necessity Form is found on the Forms Page of the provider website.
For more information regarding EPSDT services contact the DPHHS Health Resources Division, Maternal and Child Health Nurse .
Who Can Provide EPSDT Screenings?
- Physicians
- Advanced Registered Nurse Practitioners (ARNP)
- Physician assistants
- Registered nurse under guidance of a physician or ARNP may perform the screenings but not diagnose or treat.
- Providers must be Montana Healthcare Programs-enrolled to receive payment from Montana Healthcare Programs.
The Well-Child Screen
The foundation of EPSDT is the well-child screen. These screens should begin as early as possible in a child’s life or as soon as the child is enrolled in Montana Healthcare Programs. The well-child screens are based on a periodicity schedule established by medical, dental, and other healthcare experts, including the American Academy of Pediatrics. The Well-Child Screen Recommendations are found on the Bright Futures website, https://brightfutures.aap.org.
Every infant should have a newborn evaluation after birth. If a child comes under care for the first time at any point on the schedule, or if any items are not accomplished at the suggested age, the schedule should be brought up-to-date at the earliest possible time. If a well-child screen shows that a child is at risk based on the child’s environment, history, or test results, the provider should perform required or recommended tests even though they may not be indicated for the child’s age. Developmental, psychosocial, and chronic disease issues for children and adolescents may require frequent counseling and treatment visits separate from preventive care visits.
Using an evidence-based screening tool, a caregiver depression screening is covered under an enrolled child's Montana Healthcare Programs benefit, during their first year of life. This includes anyone that is considered a child's primary care provider. Positive screenings must be appropriately referred. Screenings are covered under the child’s Montana Healthcare Programs benefit due to the dyadic relationship of a caregiver and child. The service is directed at treating the health and well-being of the child, with a goal of providing a healthy start to their life.
Initial/Interval History
A comprehensive history, obtained from the parent or other responsible adult who is familiar with the child’s history should be done during the initial visit. Once it is done, it only needs to be updated at subsequent visits. The history should include the following:
- Developmental history to determine whether the child’s individual developmental processes fall within a normal range of achievement compared to other children of his/her age and cultural background.
- Discussion of the child’s development, as well as techniques to enhance the child’s development, with the parents.
- Nutritional history and status. Questions about dietary practices identify unusual eating habits, such as pica, or extended use of bottle feedings, or diets that are deficient or excessive in one or more nutrients.
- Complete dental history.
Developmental Assessments
Appropriate Developmental Surveillance. Providers should administer an age-appropriate developmental screen at each well-child visit. Any concerns raised during the surveillance should be promptly addressed with standardized developmental screening tests. See the recommended algorithm provided by Bright Futures at http://pediatrics.aappublications.org/content/118/1/405.full.
Appropriate Developmental Screening. Providers should administer an age appropriate developmental screen at age 9, 18, and 30 months. Results should be considered in combination with other information gained through the history, physical examination, observation, and reports of behavior. If developmental problems are identified, appropriate follow-up and/or referral to proper resources should be made.
Speech and language screens identify delays in development. The most important readiness period for speech is 9 to 24 months. Parents should be urged to talk to their children early and frequently. Refer the child for speech and language evaluation as indicated.
Parents of children with developmental disabilities should be encouraged to contact Parents Let’s Unite for Kids (PLUK).
PLUK is an organization designed to provide support, training, and assistance to children with disabilities and their parents. Call, write, or visit the PLUK website, http://www. pluk.org/.
PLUK
516 North 32nd Street
Billings, MT 59101-6003
(406) 255-0540 Phone
(800) 222-7585 Toll Free
(406) 255-0523 Fax
E-Mail info@pluk.org
Depression Screening. Signs and symptoms of emotional disturbances represent deviations from or limitations in healthy development. These problems usually will not warrant a psychiatric referral but can be handled by the provider. He/she should discuss problems with parents and give advice. If a psychiatric referral is warranted, the provider should refer the child to an appropriate provider. Recommended screening using the Member Health Questionnaire (PHQ-2) or other tools found on the Bright Futures website.
Alcohol and Drug Use Screen. The provider should screen for risky behaviors (e.g., substance abuse, unprotected sexual activity, tobacco use, firearm possession). In most instances, indications of such behavior will not warrant a referral but can be handled by the provider, who should discuss the problems with the member and the parents and give advice. If a referral is warranted, the provider should refer to an appropriate provider. Recommended screening tool can be found on the Bright Futures website.
Nutritional Screen
Providers should assess the nutritional status at each well-child screen. Children with nutritional problems may be referred to a licensed nutritionist or dietician for further assessment or counseling.
Unclothed Physical Inspection
At each visit, a complete physical examination is essential. Infants should be totally unclothed and older children undressed and suitably draped.
Vision Screen
A vision screen appropriate to the age of the child should be conducted at each well-child screen. If the child is uncooperative, rescreen within six months.
Hearing Screen
A hearing screen appropriate to the age of the child should be conducted at each well-child screen. All newborns should be screened.
Autism Screen
Autism screenings are recommended at age 18 and 24 months, and a recommended tool is provided on the Bright Futures website.
Critical Congenital Heart Defect Screen
Screening using pulse oximetry should be performed in newborns, after 24 hours old and before discharge.
Laboratory Tests
Providers who conduct well-child screens must use their medical judgment in determining applicability of performing specific laboratory tests. Appropriate tests should be performed on children determined at risk through screening and assessment.
Hematocrit and Hemoglobin. Hematocrit or hemoglobin tests should be done for at-risk (premature and low birth weight) infants at ages newborn and 2 months. For children who are not at risk, follow the recommended schedule.
Blood Lead Level. All children in Montana Healthcare Programs are at risk of lead poisoning. To ensure their good health, the federal government requires that all Montana Healthcare Programs-enrolled children be tested for lead poisoning. Testing is recommended at 12 and 24 months of age. Children up to age 6 years who have not been checked for lead poisoning before should also be tested.
A blood lead level test should be performed on all children at 12 and 24 months of age.
All Montana Healthcare Programs children at other ages should be screened. Complete a verbal risk assessment for all Montana Healthcare Programs children up to age 6 years at each EPSDT screening:
- Does your child live in Butte, Walkerville, or East Helena, which are designated high-risk areas?
- Does your child live near a lead smelter, battery recycling plant, or other industry (operating or closed) likely to release lead?
- Does your child live in or regularly visit a house built before 1960, which contains lead paint?
- Does your child live near a heavily traveled major highway where soil and dust may be contaminated with lead?
- Does your child live in a home where the plumbing consists of lead pipes or copper with lead solder joints?
- Does your child frequently come in contact with an adult who works with lead, such as construction, welding, pottery, reloading ammunition (making own bullets), etc.?
- Is the child given any home or folk remedies? If yes, discuss.
If the answer to all questions is no, a child is considered at low risk for high doses of lead exposure. Children at low risk for lead exposure should receive a blood test at 12 and 24 months.
If the answer to any question is yes, a child is considered at high risk for high doses of lead exposure and a blood lead level test must be obtained immediately regardless of the child’s age.
Tuberculin Screening. Tuberculin testing should be done on individuals in high-risk populations or if historical findings, physical examination, or other risk factors so indicate.
Dyslipidemia Screening. Screening should be considered based on risk factors and family history at 24 months, 4, 6, 8, 12, 13, 14, 15, 16, and 17 years, and is indicated at or around 10 and 20 years of age.
STI/HIV Screening. All adolescent members should be screened for sexually transmitted infections (STIs) and HIV based on risk assessment starting at age 11 and reassessed annually with at least one assessment occurring between the ages of 16–18 years old.
Cervical Dysplasia Screening. Adolescents are not routinely screened for cervical dysplasia until age 21. See the 2010 AAP statement for indications at https://www.aap.org/en-us/Pages/Default.aspx.
Immunizations
The immunization status of each child should be reviewed at each well-child screen. This includes interviewing parents or caretakers, reviewing immunization records, and reviewing risk factors.
The Recommended Childhood Immunization schedule is available on the AMA website and the Centers for Disease Control and Prevention website.
Dental Screen
The child’s provider should perform annual dental screens, and results should be included in the child’s initial/interval history. Annual dental screens include an oral inspection, fluoride varnish (as available) and making a referral to a dentist for any of the following reasons:
- When the first tooth erupts, and every six months thereafter.
- If a child with a first tooth has not obtained a complete dental examination by a dentist in the past 12 months.
- If an oral inspection reveals cavities or infection, or if the child is developing a handicapping malocclusion or significant abnormality.
Discussion and Counseling/Anticipatory Guidance
Providers should discuss examination results, address assessed risks, and answer any questions in accordance with parents’ level of understanding. Age-appropriate discussion and counseling should be an integral part of each visit. Allow sufficient time for unhurried discussions.
At each screening visit, provide age-appropriate anticipatory guidance concerning such topics as the following:
- Auto safety: Car seats, seat belts, air bags, positioning young or lightweight children in the backseat.
- Recreational safety: Helmets and protective padding, playground equipment.
- Home hazards: Poisons, accidents, weapons, matches/lighters, staying at home alone, use of detectors for smoke, radon gas, and carbon monoxide.
- Exposure to sun and secondhand smoke.
- Adequate sleep, exercise, and nutrition, including eating habits and eating disorders.
- Peer pressure.
- General health: Immunizations, patterns of respiratory infections, skin eruptions, care of teeth.
- Problems such as whining, stealing, setting fires, etc. as indicated by parental concern.
- Behavior and development: Sleep patterns, temper, attempts at independence (normal and unpleasant behavior), curiosity, speech and language, sex education and development, sexual activities, attention span, toilet training, alcohol and tobacco use, substance abuse.
- Interpersonal relations: Attitude of father; attitude of mother; place of child in family; jealousy; selfishness, sharing, taking turns; fear of strangers; discipline, obedience; manners, courtesy; peer companionship/relations; attention getting; preschool, kindergarten and school readiness and performance; use of money; assumption of responsibility; need for affection and praise; competitive athletics.
End of EPSDT Well-Child Chapter
Prior Authorization
What Is Prior Authorization?
Prior authorization refers to a list of services that require Department authorization before they are performed. Some services may require both Passport referral and prior authorization.
Montana Healthcare Programs does not pay for services when prior authorization, Passport, or Team Care requirements are not met.
In practice, providers will often encounter members who are enrolled in Passport. Whether the member is enrolled in Passport or Team Care, the eligibility information denotes the member’s primary care provider. Services are only covered when they are provided or approved by the designated Passport provider or Team Care pharmacy shown in the eligibility information.
If a service requires prior authorization, the requirement exists for all Montana Healthcare Programs members. Prior authorization is usually obtained through the Department or a prior authorization contractor.
When both Passport and prior authorization are required, they must be recorded in different places on the claim.
If both Passport referral and prior authorization are required for a service, then both numbers must be recorded in different fields on the Montana Healthcare Programs claim form. (See the Submitting a Claim section in this manual.)
Most Montana Healthcare Programs fee schedules indicate when prior authorization is required for a service. For more information, see your provider type fee schedule and/or the Prior Authorization page of the Provider Information website.
End of Prior Authorization Chapter
Telemedicine
Program Overview
Telemedicine is the use of interactive audio-video equipment to link practitioners and members located at different sites. The Montana Healthcare Programs Program reimburses providers for medically necessary telemedicine services furnished to eligible members.
Telemedicine is not itself a unique service but a means of providing selected services approved by Montana Healthcare Programs. Telemedicine involves two collaborating providers, an originating provider and a distance provider. The provider where the member is located is the originating provider or originating site. In most cases, the distant provider is a clinician who acts as a consultant to the originating provider. However, in some cases the distant provider may be the only provider involved in the service.
Providers must be enrolled as Montana Healthcare Programs providers and be licensed in the State of Montana in order to:
- Treat a Montana Healthcare Programs member; and
- Submit claims for payment to Montana Healthcare Programs
When to Use Telemedicine
Montana Healthcare Programs considers the primary purposes of telemedicine are to bring providers to people living in rural areas, and to allow members access to care that is not available within their community. Providers should weigh these advantages against quality of care and member safety considerations. Members may choose which is more convenient for them when providers make telemedicine available.
Telemedicine should not be selected when face-to-face services are medically necessary. Members should establish relationships with primary care providers who are available on a face-to-face basis.
Telemedicine can be provided in member’s residence; the distance provider is responsible for the confidentiality requirements. Member’s residences do not qualify for originating provider reimbursement.
Telemedicine Confidentiality Requirements
All Montana Healthcare Programs providers using telemedicine to deliver Montana Healthcare Programs services must employ existing quality-of-care protocols and member confidentiality guidelines when providing telemedicine services. Health benefits provided through telemedicine must meet the same standard of care as in-person care. Record keeping should comply with Montana Healthcare Programs requirements in Administrative Rules of Montana (ARM) 37.85.414.
Transmissions must be performed on dedicated secure lines or must utilize an acceptable method of encryption adequate to protect the confidentiality and integrity of the transmission. Transmissions must employ acceptable authentication and identification procedures by both the sender and receiver.
General Billing Instructions
Providers may only bill procedure codes for which they are already eligible to bill. Services not otherwise covered by Montana Healthcare Programs are not covered when delivered via telemedicine. The use of telecommunication equipment does not change prior authorization or any other Montana Healthcare Programs requirements established for the services being provided.
The availability of services through telemedicine in no way alters the scope of practice of any health care provider; or authorizes the delivery of health care services in a setting or manner not otherwise authorized by law.
Telemedicine reimbursement does not include:
- Consultations provided by telephone (interactive audio); or
- Facsimile machine transmissions.
- Crisis hotlines
The originating and distant providers may not be within the same facility or community. The same provider may not be the pay to for both the originating and distance provider.
If a rendering provider’s number is required on the claim for a face-to-face visit, it is required on a telemedicine claim.
Originating Provider Requirements
The originating site provider must have secure and appropriate equipment to ensure confidentiality, including camera(s), lighting, transmission and other needed electronics.
Originating providers bill using procedure code Q3014 (telemedicine originating site fee) for the use of a room and telecommunication equipment. The telehealth place of service code 02 does not apply to originating site facilities billing a facility fee.
The following provider types may bill procedure code Q3014:
- Outpatient Hospital;
- Critical Access Hospital*;
- Federally Qualified Health Center*;
- Rural Health Center*;
- Indian Health Service*;
- Physician;
- Psychiatrist;
- Mid-Levels;
- Dieticians;
- Psychologists;
- Licensed Clinical Social Worker;
- Licensed Professional Counselor;
- Mental Health Center:
- Chemical Dependency Clinic;
- Group/Clinic;
- Public Health Clinic; or
- Family Planning Clinic.
*Reimbursement for Q3014 is a set fee and is paid outside of both the cost to charge ratio and the all-inclusive rate.
Originating provider claims must include a specific diagnosis code to indicate why a member is being seen by the distance provider. The originating site must request the diagnosis code(s) from the distance site prior to billing the telemedicine appointment.
The originating provider may also, as appropriate; bill for clinical services provided on-site the same day that a telemedicine originating site service is provided. This originating site may not bill for assisting the distant provider with an examination, this includes any services that would be normally included in a face-to-face visit.
Distance Provider Requirements
Distance providers should submit claims for telehealth services using the appropriate CPT or HCPCS code for the professional service along with the GT modifier (interactive communication). Effective January 1, 2017, providers must also use the telehealth place of service of 02 for claims submitted on a CMS-1500 claim. By coding with the GT modifier and the 02 place of service, the provider is certifying that the service was a face-to-face visit provided via interactive audio-video telemedicine.
Any out of state distance providers must be licensed in the State of Montana and enrolled in Montana Healthcare Programs in order to provide telemedicine services to Montana Healthcare Programs members. Providers must contact the Montana Department of Labor and Industry to find out details on licensing requirements for their applicable professional licensure.
End of Telemedicine Chapter
Member Eligibility and Responsibilities
Montana Healthcare Programs ID Cards
Each Montana Healthcare Programs member is issued his/her own permanent Montana Access to Health Montana Healthcare Programs ID card (including QMB only members), Healthy Montana Kids Plus (HMK Plus) card.
Members must never throw away the card, even if their Montana Healthcare Programs eligibility ends.
The ID card lists the member’s name, member number, and date of birth. The member number may be used for checking eligibility and for billing Montana Healthcare Programs.
Since eligibility information is not on the card, providers must verify eligibility before providing services. See the Verifying Member Eligibility section below.
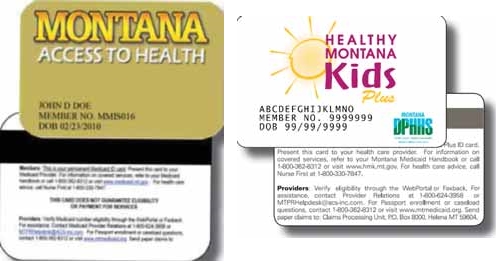
Providers should verify eligibility before providing services.
Verifying Member Eligibility
Member eligibility may change monthly. Providers should verify eligibility at each visit using any of the methods described in the following table.
The list below shows information returned to the provider in response to an eligibility inquiry:
- Member’s Montana Healthcare Programs ID number. Used when billing Montana Healthcare Programs.
- Eligibility Status. Montana Healthcare Programs eligibility status for the requested dates:
- Standard Montana Healthcare Programs. Member is eligible for all Montana Healthcare Programs covered services.
- QMB. Member is a qualified Medicare beneficiary. See the section titled When a Member Has Other Coverage in this chapter.
- Team Care. TC indicator means member is enrolled in the Team Care program. All services must be provided or approved by the designated Passport provider.
- Designated Provider. The member’s primary care provider’s name and phone number are shown for members who are enrolled in Passport to Health or Team Care. In either case, all services must be provided or approved by the designated provider. See the Passport to Health provider manual.
- TPL. If the member has other insurance coverage (TPL), the name of the other insurance carrier is shown.
- Medicare ID Number. A Medicare identification number for members who are eligible for both Montana Healthcare Programs and Medicare.
Member without Card
Since eligibility information is not on the card, it is necessary for providers to verify eligibility before providing services whether or not the member presents a card. Confirm eligibility using one of the methods shown in the Verifying Member Eligibility table. If eligibility is not available, the provider may contact the member’s local Office of Public Assistance (OPA).
Newborns
Care rendered to newborns can be billed under the newborn’s original Montana Healthcare Programs ID number assigned by the mother’s local OPA until a permanent ID number becomes available. The hospital or the parents may apply for the child’s Social Security number. Parents are responsible for notifying their local OPA when they have received the child’s new Social Security number.
Inmates in Public Institutions (ARM 37.82.1321)
Montana Healthcare Programs does not cover members who are inmates in a public institution.
Presumptive Eligibility
Presumptive eligibility is available to hospitals and their affiliated facilities that participate with Montana Healthcare Programs.
Personnel must be trained and certified to make presumptive eligibility determinations for short-term, temporary coverage for the following coverage groups:
- Adults between the ages of 18 and 26 who were in Foster Care and receiving Montana Healthcare Programs at age 18
- Healthy Montana Kids Plus
- Healthy Montana Kids
- Parent/Caretaker Relative Montana Healthcare Programs
- Pregnant women (ambulatory prenatal care)
- Women between the ages of 19 and 64 who have been screened and diagnosed with breast or cervical cancer.
To encourage prenatal care, uninsured pregnant women may receive presumptive eligibility for Montana Healthcare Programs.
Presumptive eligibility may be for only part of a month and does not cover inpatient hospital services, but does include other applicable Montana Healthcare Programs services.
Retroactive Eligibility
When a member is determined retroactively eligible for Montana Healthcare Programs, the member should give the provider a Notice of Retroactive Eligibility (160-M). The provider has 12 months from the date retroactive eligibility was determined to bill for those services.
Retroactive Montana Healthcare Programs eligibility does not allow a provider to bypass prior authorization requirements. See specific provider manuals for requirements.
When a member becomes retroactively eligible for Montana Healthcare Programs, the provider may:
- Accept the member as a Montana Healthcare Programs member from the current date.
- Accept the member as a Montana Healthcare Programs member from the date retroactive eligibility was effective.
- Require the member to continue as a private-pay member.
Institutional providers (nursing facilities, skilled care nursing facilities, intermediate care facilities for the mentally retarded, institutions for mental disease, inpatient psychiatric hospitals, and residential treatment facilities) must accept retroactively eligible member from the date eligibility was effective. Non-emergency transportation and eyeglass providers cannot accept retroactive eligibility. For more information on billing Montana Healthcare Programs for retroactive eligibility services, see the Billing Procedures chapter in this manual.
Coverage for the Medically Needy
This coverage is for members who have an income level that is higher than the SSI-eligible Montana Healthcare Programs program standards. However, when a member has high medical expenses relative to income he/she can become eligible for Montana Healthcare Programs by incurring medical expenses and/or making a cash payment equal to the spend down amount on a monthly basis. The spend down amount is based on the member's countable income. When the member chooses to use the Medical Expense option to meet their spend down, he/she is responsible to pay for medical services before Montana Healthcare Programs eligibility begins and Montana Healthcare Programs pays for remaining covered services.
Providers should verify if medically needy members are covered by Montana Healthcare Programs on the date of service to determine whether to bill the member or Montana Healthcare Programs.
Because eligibility does not cover an entire month, when the medical expense option is used the member’s eligibility information may show eligibility for only part of the month and the provider may receive a One Day Authorization Notice. The One Day Authorization Notice , sent by the local OPA, states the date eligibility began and the portion of the bill the member must pay. If the provider has not received a One Day Authorization Notice , he/she should verify eligibility for the date of service by any method described in this chapter or by contacting the member’s local OPA. Since this eligibility may be determined retroactively, the provider may receive the One Day Authorization Notice weeks or months after services have been provided.
Members may choose the cash option process where they can pay a monthly premium to Montana Healthcare Programs equal to the spend down amount, instead of making payments to providers, and have Montana Healthcare Programs coverage for the entire month. This method results in quicker payment, simplifies the eligibility process, and eliminates spend down notices. Providers may encourage but not require members to use the cash option.
It is important to note that after a member submits their payment to Montana Healthcare Programs, the Department requires time to process the payment. Once the payment is processed, the system will provide the Montana Healthcare Programs coverage. The member may choose to submit their payment to Montana Healthcare Programs after medical services have been provided. In that situation, the member's Montana Healthcare Programs eligibility information will not be available at the time the service is provided and any claims submitted at that time will be denied. Once the spend down has been paid and processed, active eligibility will display and claims can be submitted.
Nurse First
Nurse First programs provide disease management and nurse triage services for Montana Healthcare Programs members throughout the state.
Nurse First Advice Line, 1-800-330-7847. A toll-free, confidential telephone number members may call 24/7/365 for advice from a registered nurse about injuries, diseases, healthcare, or medications. The nurses do not diagnose or provide treatment. Most Montana Healthcare Programs members are eligible to use the Nurse First Advice Line,The program is voluntary though participation is strongly encouraged.
Montana Breast and Cervical Cancer Treatment Program
This program provides Standard Montana Healthcare Programs coverage for women who have been screened through the Montana Breast and Cervical Health Program (MBCHP) and diagnosed with breast and/or cervical cancer or a pre-cancerous condition. All other policies and procedures in this chapter apply. For information regarding screening through the MBCHP program, call 1-888-803-9343.
When a Member Has Other Coverage
Montana Healthcare Programs members often have coverage through Medicare, workers’ compensation, employment-based coverage, individually purchased coverage, etc. Coordination of benefits is the process of determining which source of coverage is the primary payer in a particular situation. In general, providers should bill other carriers before billing Montana Healthcare Programs, but there are some exceptions. (See the section titled Exceptions to Billing Third Party First in this chapter.) Medicare is processed differently than other sources of coverage.
Identifying Additional Coverage
The member’s Montana Healthcare Programs eligibility verification may identify other payers such as Medicare or other third party payers. If a member has Medicare, the Medicare ID number is provided. If a member has additional coverage, the carrier is shown. Some examples of third party payers include:
- Private health insurance
- Employment-related health insurance
- Workers’ compensation insurance*
- Health insurance from an absent parent
- Automobile insurance*
- Court judgments and settlements*
- Long-term care insurance
*These third party payers (and others) may not be listed on the member’s eligibility verification.
Providers should use the same procedures for locating third party sources for Montana Healthcare Programs members as for their non-Montana Healthcare Programs members. Providers cannot refuse service because of a third party payer or potential third party payer.
When a Member Has Medicare
Medicare claims are processed and paid differently than other non-Montana Healthcare Programs claims. The other sources of coverage are called third party liability or TPL, but Medicare is not.
Medicare Part A Claims
Medicare Part A carriers and Montana Healthcare Programs use electronic exchange of institutional claims covering Part A services. Providers must submit these claims first to Medicare. After Medicare processes the claim, an Explanation of Medicare Benefits (EOMB) is sent to the provider. The provider then reviews the EOMB and submits the claim to Montana Healthcare Programs.
Medicare Part B Crossover Claims
The Department has an agreement with the Medicare Part B carrier for Montana (Noridian) and the Durable Medical Equipment Regional Carrier (DMERC) under which the carriers provide the Department with claims for members who have both Medicare and Montana Healthcare Programs coverage. Providers must tell Medicare that they want their claims sent to Montana Healthcare Programs automatically, and must have their Medicare provider number on file with Montana Healthcare Programs.
When members have both Medicare and Montana Healthcare Programs covered claims, and have made arrangements with both Medicare and Montana Healthcare Programs, Part B services need not be submitted to Montana Healthcare Programs. When a crossover claim is submitted only to Medicare, Medicare will process the claim, submit it to Montana Healthcare Programs, and send the provider an explanation of Medicare benefits (EOMB). Providers must check the EOMB for the statement indicating that the claim has been referred to Montana Healthcare Programs for further processing. It is the provider’s responsibility to follow up on crossover claims and make sure they are correctly billed to Montana Healthcare Programs within the timely filing limit. (See the Billing Procedures chapter in this manual.)
Providers should submit Medicare crossover claims to Montana Healthcare Programs only when:
- The referral to Montana Healthcare Programs statement is missing. In this case, submit a claim and a copy of the Medicare EOMB to Montana Healthcare Programs for processing.
- The referral to Montana Healthcare Programs statement is present, but there is no response from Montana Healthcare Programs within 45 days of receiving the Medicare EOMB. Submit a claim and a copy of the Medicare EOMB to Montana Healthcare Programs for processing.
- Medicare denies the claim. The provider may submit the claim to Montana Healthcare Programs with the EOMB and denial explanation (as long as the claim has not automatically crossed over from Medicare).
When submitting electronic claims with paper attachments, see the Billing Electronically with Paper Attachments section of the Billing Procedures chapter.
When submitting a claim with the Medicare EOMB, use Montana Healthcare Programs billing instructions and codes. Medicare’s instructions, codes, and modifiers may not be the same as Montana Healthcare Programs’s. The claim must also include the Montana Healthcare Programs provider number and Montana Healthcare Programs member ID number. It is the provider’s responsibility to follow up on crossover claims and make sure they are correctly billed to Montana Healthcare Programs within the timely filing limit.
When a Member Has TPL (ARM 37.85.407)
When a Montana Healthcare Programs member has additional medical coverage (other than Medicare) it is often referred to as third party liability or TPL. In most cases, providers must bill other insurance carriers before billing Montana Healthcare Programs.
Providers are required to notify their members that any funds the member receives from third party payers (when the services were billed to Montana Healthcare Programs) must be turned over to the Department. These words printed on the member’s statement fulfill this obligation: When services are covered by Montana Healthcare Programs and another source, any payment the member receives from the other source must be turned over to Montana Healthcare Programs.
Exceptions to Billing Third Party First
In a few cases, providers may bill Montana Healthcare Programs first:
- When a Montana Healthcare Programs member is also covered by Indian Health Service (IHS) or the Crime Victim Compensation Program, providers must bill Montana Healthcare Programs first. These are not considered a third party liability.
- When a member has Montana Healthcare Programs eligibility and MHSP eligibility for the same month, Montana Healthcare Programs must be billed first.
- ICD prenatal and ICD preventive pediatric diagnosis conditions may be billed to Montana Healthcare Programs first. In these cases, Montana Healthcare Programs will “pay and chase” or recover payment itself from the third party payer.
- The following services may also be billed to Montana Healthcare Programs first:
- Nursing facility (as billed on nursing home claims)
- Audiology
- Eyeglasses
- Hearing aids and batteries
- Home and community-based services (waiver)
- Optometry
- Oxygen in a nursing facility
- Personal assistance/Community First Choice
- Transportation (other than ambulance)
- If the third party has only potential liability, the provider may bill Montana Healthcare Programs first. Do not indicate the potential third party on the claim. Instead, notify the Department by sending the claim and notification to Third Party Liability, P.O. Box 5838, Helena, MT 59604.
Requesting an Exemption
Providers may request to bill Montana Healthcare Programs first under certain circumstances. In each of these cases, the claim and required information should be sent directly to the Third Party Liability unit.
- When a provider is unable to obtain a valid assignment of benefits, the provider should submit the claim with documentation that he/she attempted to obtain assignment and certification that the attempt was unsuccessful.
- When the provider has billed the third party insurance and has received a non-specific denial (e.g., no member name, date of service, amount billed), submit the claim with a copy of the denial and a letter of explanation.
- When the Child Support Enforcement Division has required an absent parent to have insurance on a child, the claim can be submitted to Montana Healthcare Programs then the following requirements are met:
- The third party carrier has been billed, and 30 days or more have passed since the date of service.
- The claim is accompanied by a certification that the claim was billed to the third party carrier, and payment or denial has not been received.
- If another insurance has been billed, and 90 days have passed with no response, submit the claim with a note explaining that the insurance company has been billed (or a copy of the letter sent to the insurance company). Include the date the claim was submitted to the insurance company and certification that there has been no response.
When the Third Party Pays or Denies a Service
When a third party payer is involved (excluding Medicare) and the other payer:
- Pays the claim, indicate the amount paid when submitting the claim to Montana Healthcare Programs for processing.
- Allows the claim, and the allowed amount went toward the member’s deductible, include the insurance explanation of benefits (EOB) when billing Montana Healthcare Programs.
- Denies the claim, submit the claim and a copy of the denial (including the reason explanation) to Montana Healthcare Programs.
- Denies a line on the claim, bill the denied line on a separate claim and submit to Montana Healthcare Programs. Include the EOB from the other payer and an explanation of the reason for denial (e.g., definition of denial codes).
When the Third Party Does Not Respond
If another insurance has been billed, and 90 days have passed with no response, bill Montana Healthcare Programs as follows:
- Submit the claim and a note explaining that the insurance company has been billed, or submit a copy of the letter sent to the insurance company.
- Include the date the claim was submitted to the insurance company.
- Send this information to the Third Party Liability Unit.
Coordination Between Medicare and Montana Healthcare Programs
Coordination of benefits between Medicare and Montana Healthcare Programs is generally accomplished through electronic crossover of claims. It is important to always bill Medicare prior to Montana Healthcare Programs for healthcare services. After Medicare processes the claim, it will automatically cross over to Montana Healthcare Programs. If a claim does not cross automatically to Montana Healthcare Programs from Medicare, the provider should not submit the claim to Montana Healthcare Programs until Medicare has processed. Montana Healthcare Programs payment is subsequent to Medicare and will only pay up to the Montana Healthcare Programs fee after considering the payment from Medicare. See the How Payment Is Calculated chapter in the provider type manuals to learn how Montana Healthcare Programs payments are calculated.
- Qualified Medicare Beneficiary (QMB). For QMBs, Montana Healthcare Programs pays their Medicare A and B premiums and some or all of the Medicare coinsurance and deductibles (up to the Montana Healthcare Programs fee). QMB members may or may not also be eligible for Montana Healthcare Programs benefits.
- QMB Only. Montana Healthcare Programs will make payments only toward the Medicare coinsurance and deductible.
- QMB and Montana Healthcare Programs. Covered services include the same services as for Montana Healthcare Programs only members. If a service is covered by Medicare but not by Montana Healthcare Programs, Montana Healthcare Programs will pay all or part of the Medicare coinsurance and deductible. If a service is covered by Montana Healthcare Programs but not by Medicare, then Montana Healthcare Programs will be the primary payer for that service.
- Specified Low-Income Medicare Beneficiary (SLMB). Montana Healthcare Programs pays the Medicare Part B premium only.
- SLMB Only. Members do not receive Montana Healthcare Programs cards, are not eligible for other Montana Healthcare Programs benefits, and must pay their own Medicare coinsurance and deductibles.
- SLMB and Montana Healthcare Programs. For services Medicare covers, Montana Healthcare Programs will pay the lower of the Medicare coinsurance and deductible or the Montana Healthcare Programs fee less Medicare payments for Montana Healthcare Programs covered services. If a service is covered by Medicare but not by Montana Healthcare Programs, Montana Healthcare Programs will not pay coinsurance, deductible, or any other cost of the service. For services Medicare does not cover but Montana Healthcare Programs covers, Montana Healthcare Programs will be the primary payer for that service.
- Qualifying Individual (QI). Montana Healthcare Programs pays the Medicare Part B premium only. Members should not have a dual eligibility when qualifying under the QI program. In other words, members cannot have QI and Montana Healthcare Programs at the same time. When a QI recipient becomes Montana Healthcare Programs-eligible, the QI benefit is canceled and replaced by the Montana Healthcare Programs eligibility.
Montana Healthcare Programs Benefits for Dually Eligible Members
Type of Dual Eligible: QMB only
Medicare Premium Paid by: Montana Healthcare Programs
Medicare Coinsurance and Deductible Paid by: Montana Healthcare Programs*
Type of Dual Eligible: QMB/Montana Healthcare Programs
Medicare Premium Paid by: Montana Healthcare Programs
Medicare Coinsurance and Deductible Paid by: Montana Healthcare Programs*
Type of Dual Eligible: Other dual eligibles
Medicare Premium Paid by: Member
Medicare Coinsurance and Deductible Paid by: Montana Healthcare Programs*
Type of Dual Eligible: Specified Low-Income Medicare Beneficiary
Medicare Premium Paid by: Montana Healthcare Programs
Medicare Coinsurance and Deductible Paid by: Member
*See the How Payment Is Made chapter in your provider type manual to learn how Montana Healthcare Programs calculates payment for Medicare coinsurance and deductibles.
Members with Other Sources of Coverage
Montana Healthcare Programs members may also have coverage through workers’ compensation, employment-based coverage, individually purchased coverage, etc. Other parties also may be responsible for healthcare costs. Examples of these situations include communal living arrangements, child support, or auto accident insurance. These other sources of coverage have no effect on what services Montana Healthcare Programs covers. However, other coverage does affect the payment procedures. (See the How Payment Is Calculated chapter in your provider type manual.)
The Health Insurance Premium Payment (HIPP) Program
Some Montana Healthcare Programs members have access to private insurance coverage, typically through a job, but do not enroll because they cannot afford the premiums. In these cases, Montana Healthcare Programs may pay the premiums, at which time the private insurance plan becomes the primary insurer. The member also remains eligible for Montana Healthcare Programs. When Montana Healthcare Programs members have access to private insurance coverage, they may apply for the HIPP program.
Indian Health Service (IHS)
The Indian Health Service (IHS) provides federal health services to American Indians and Alaska Natives. IHS is a secondary payer to Montana Healthcare Programs. For more information, see the Subsidized Health Insurance Programs in Montana table at the end of this chapter.
Crime Victims
The Crime Victim Compensation Program is designed to help victims of crime heal. This program may provide funding for medical expenses, mental health counseling, lost wages support, funerals, and attorney fees. Crime Victim Compensation is a secondary payer to Montana Healthcare Programs. For more information, see the Subsidized Health Insurance Programs in Montana table later in this chapter.
When Members Are Uninsured
Several state and federal programs are available to help the uninsured; see the Subsidized Health Insurance Programs in Montana table at the end of this chapter.
Member Responsibilities
Montana Healthcare Programs members are required to:
- Know and understand what Standard Montana Healthcare Programs benefits include.
- Notify providers that they have Montana Healthcare Programs coverage.
- Present a valid Montana Access to Health (MATH) or Healthy Montana Kids (HMK) Plus card at each visit.
- Notify providers of any other coverage, such as Medicare or private insurance.
- Notify providers of any change in coverage.
- Forward any money received from other insurance payers to the provider.
- Inform their local office of public assistance about any changes in address, income, etc.
Montana Healthcare Programs members may see any Montana Healthcare Programs-enrolled provider as long as Passport to Health and prior authorization guidelines are followed, and as long as they are not enrolled in Team Care.
Other Programs
Member eligibility provisions also apply to Department of Public Health and Human Services programs other than Montana Healthcare Programs. The information covered in this chapter applies to members enrolled in the Mental Health Services Plan (MHSP) and Healthy Montana Kids (HMK) dental services and eyeglasses only.
Chemical Dependency Bureau State Paid Substance Dependency/Abuse Treatment Program (CDB-SPSDATP)
Members in this program are not issued a Montana Access to Health card. Members should apply for services directly from the state-approved programs. For a list of these programs, call 406-444-9408. Services require prior authorization and authorization for continued stay review.
Healthy Montana Kids (HMK)
Few children are eligible for both Montana Healthcare Programs and HMK simultaneously. If a patient presents both cards, check the dates of Montana Healthcare Programs eligibility and the child’s HMK enrollment. If both cards are valid, treat the patient as an HMK patient. Services not covered by HMK may be covered by Montana Healthcare Programs.
If a member presents an HMK card for dental services, the provider should refer to the HMK dental services manual for information about coverage and billing. If a member presents an HMK card for eyeglasses, the card is valid only with the HMK program’s designated supplier. (See the HMK section of the Optometric and Eyeglass Services manual.) If a member presents an HMK card for any other service, see the HMK provider manual published by Blue Cross and Blue Shield of Montana. Call 1-800-447-7828 for more information.
Mental Health Services Plan (MHSP)
MHSP members will present a hard white plastic card. Their MHSP card makes them eligible only for those services covered by MHSP, which are described in the mental health and prescription drug manuals. Montana Healthcare Programs members do not need an MHSP card to receive mental health services.
Subsidized Health Insurance Programs in Montana
Providers may refer member to the following programs.
Program: Children’s Special Health Services
Administered by: Montana DPHHS
Target Populations: Children with special healthcare needs.
For Information on Eligibility:
(800) 762-9891
(406) 444-3622
Program: Crime Victim Compensation Program
Administered by: Montana Department of Justice
Target Populations: Crime victims and their dependents and relatives.
For Information on Eligibility:
406-444-3653 Helena
800-498-6455
https://dojmt.gov/victims/crime-victim-compensation/
Program: Indian Health Service
Administered by: Billings Area Indian Health Service
Target Populations: All enrolled members of federally recognized tribes.
For Information on Eligibility:
406-247-7107
Program: Montana Healthcare Programs
Administered by: Montana DPHHS
Target Populations: Low-income children and their family members, and disabled individuals.
For Information on Eligibility:
Local Office of Public Assistance
https://dphhs.mt.gov/hcsd/OfficeofPublicAssistance
Program: Medicare
Administered by: Centers for Medicare and Montana Healthcare Programs Services
Target Populations: People who are age 65 and over, have a disability, or have end-stage renal disease.
For Information on Eligibility:
U.S. Social Security Administration office
Program: Mental Health Services Plan (MHSP)
Administered by: Montana DPHHS
Target Populations: Individuals with a qualifying mental health diagnosis who are ineligible for Montana Healthcare Programs.
For Information on Eligibility:
Community Mental Health Center
https://dphhs.mt.gov/BHDD/mentalhealthservices/MHSP/index
Program: Workers’ Compensation
Administered by: State Fund and independent workers’ compensation insurers
Target Populations: People with injuries or illnesses related to their work.
For Information on Eligibility:
406-444-6543 Workers Compensation
Note: Eligibility rules are complex; members and providers should check with the program administrator for specifics.
End of Member Eligibility and Responsibilities Chapter
Surveillance and Utilization Review
Claims Review (MCA 53-6-111, ARM 37.85.406)
The Department is committed to paying Montana Healthcare Programs providers’ claims as quickly as possible. Montana Healthcare Programs claims are electronically processed and usually are not reviewed by medical experts prior to payment to determine if the services provided were appropriately billed. Although the computerized system can detect and deny some erroneous claims, there are many erroneous claims it cannot detect. For this reason, payment of a claim does not mean the service was correctly billed or the payment made to the provider was correct. Periodic retrospective reviews are performed that may lead to the discovery of incorrect billing or incorrect payment. If a claim is paid and the Department later discovers the service was incorrectly billed or paid or the claim was erroneous in some other way, the Department is required by federal regulation to recover any overpayment, regardless of whether the incorrect payment was the result of Department or provider error or other cause.
Surveillance and Utilization Review (42 CFR 456)
The Department’s Surveillance and Utilization Review Section (SURS) performs federally mandated retrospective reviews of paid claims (42 CFR 456). SURS is required to safeguard against unnecessary and inappropriate use of Montana Healthcare Programs services and against excess payments. If the Department pays a claim, but subsequently discovers that the provider was not entitled to payment for any reasons, the Department is entitled to recover the resulting overpayment (ARM 37.85.406).
SURS monitors compliance with state and federal rules, laws, and policies in several ways:
- New Provider Audits. SURS reviews the billing data of newly enrolled providers and may also review documentation.
- Provider Self-Audits. A self-audit is an opportunity for the provider to perform an audit and self-disclose errors to SURS. Providers may access the website for Office of Inspector General (OIG) provider self-disclosure protocol resources at http://oig.hhs.gov/compliance/self-disclosure-info/index.asp.
- Individual Audits. An individual audit is conducted by the Program Integrity Compliance Specialist in charge of reviewing the provider type being audited.
- Team Audits. Team audits are conducted by a team of Program Integrity Compliance Specialists whose individual expertise contributes to the review of the issue being audited.
- Data Mining Audits. An audit conducted by data mining which reviews the appropriateness of the data submitted on the claim, such as dates of service, procedure code, units, etc.
- Statistical Sampling. When a provider is audited, claims data is gathered for the audit time frame. If a provider has a large number of claims for which records collection and submission for a complete review would be burdensome to the provider, a statistical sample of the claims may be reviewed at the option of the Department. SURS uses a program called RAT-STATS to pull a random subset (sample) of the total claims under review (universe). The audit is then completed on the sample of claims. The determination made on the sample is then extrapolated to the entire universe. If a provider disagrees with the final determination, a 100% review of claims may be requested by the provider. More information about the statistical sampling process can be found in ARM 37.85.416.
During an audit, SURS personnel send a spreadsheet to the provider with paid claims data. The provider is required to send supporting documentation for the items listed on the spreadsheet. A SURS Program Integrity Compliance Specialist reviews the documentation and/or data submitted by the provider.
If SURS determines an overpayment that exceeds $5,000, the audit is presented to the Montana Healthcare Programs Review Committee for review and approval. With the approval of the committee, an overpayment letter will be sent to the provider.
If SURS determines an overpayment that is less than $5,000, the case is reviewed by the associated program bureau chief, program officer, SURS supervisor, and Program Compliance bureau chief. Their approval will initiate an overpayment letter to the provider.
The overpayment letter specifies the amount of the overpayment, the date the funds are due, how to appeal the Department’s decision, and the appropriate contact person.
Key Points
- The SURS unit encourages providers to call with any questions or concerns regarding the audit of paid claims.
- The Department is entitled to recover payment made to providers when a claim was paid incorrectly for any reason. (MCA 53-6-111, ARM 37.85.406)
- The Department may charge interest on recovered funds. (MCA 53-6-111)
- When an inappropriate payment has been identified, the Department may recover the overpayment by any legal means, including withholding of provider payments on subsequent claims. (MCA 53-6-111)
- The Department may sanction a provider, including suspension or termination of Montana Healthcare Programs enrollment, if the provider has failed to abide by terms of the Montana Healthcare Programs contract, federal and state laws, regulations and/or policies. (MCA 53-6-111, ARM 37.85.501–502, ARM 37.85.513)
- Prior authorization does not guarantee payment; a claim may be denied or money paid to providers may be recovered if the claim is found to be inappropriate. (MCA 53-6-111, ARM 37.85.406, ARM 37.85.410)
- The provider must upon request provide to the Department or its designated review organization without charge any records related to services or items provided to a member. The provider shall submit a true and accurate copy of each record of the service or item being reviewed as it existed within 90 days after the date on which the claim was submitted to Montana Healthcare Programs. (ARM 37.85.410, ARM 37.85.414)
Billing Tips
The following suggestions may help reduce billing errors but are not inclusive of all possible errors and recoupment scenarios.
- Be familiar with the Montana Healthcare Programs provider manuals, fee schedules, and provider notices that are in effect for the claim dates of service. Read the Claim Jumper provider newsletter. These are available on the Provider Information website.
- Comply with applicable state and federal regulations, including but not limited to the Administrative Rules of Montana. (ARM 37.85.401)
- Use CPT, HCPCS, and ICD coding books that are in effect for the claim dates of service, and refer to the long descriptions. Relying on short descriptions can result in inappropriate billing. Additional coding resources such as those noted in CPT are also recommended.
- All providers of services must maintain complete records which fully demonstrate the extent, nature, and medical necessity of services and items provided to Montana Healthcare Programs members. Information regarding the minimum requirements for records are found in ARM 37.85.414. In addition to complying with these minimum requirements, providers must also comply with any specific record keeping requirements applicable to the type of services the provider furnishes. See the Record Keeping section in the Provider Requirements chapter in this manual.
- When reimbursement is based on the length of time spent providing the service, the records must specify the time spent or the time treatment began and ended for each procedure. (ARM 37.85.414)
- Attend classes on coding offered by certified coding specialists.
- Avoid billing for the same service/supply twice. Contact Provider Relations for the status of submitted claims.
- Use specific codes rather than miscellaneous codes. For example, Code 99213 is more specific (problem-focused visit) than Code 99499 (unlisted evaluation and management service).
- Verify that the item/service meets criteria for payment by the Department. (See current fee schedule, provider manuals, and Administrative Rules of Montana.)
- Bill only under your own provider number.
- Bill only for services you provided.
- Bill for the appropriate level of service provided. For example, the CPT coding book contains detailed descriptions and examples of what differentiates a level 1 office visit (Code 99201) from a level 5 office visit (Code 99205).
- Services covered within “global periods” for certain CPT procedures are not paid separately and should not be billed separately. Most surgical and obstetric procedures and some medical procedures include routine care before and after the procedure. Montana Healthcare Programs fee schedules show the global period for each CPT service.
- Pay close attention to modifiers used with CPT and HCPCS codes on both CMS-1500 bills and UB-04 bills. Modifiers are becoming more prevalent in healthcare billing, and they often affect payment calculations.
- Choose the least costly alternative. For example, if a member is able to operate a standard wheelchair, then a motorized wheelchair should not be prescribed or provided.
- For repeat members, use an established patient code (e.g., Code 99213) instead of a first time patient code (e.g., Code 99203).
- Use the correct units measurement on CMS-1500 and UB-04 bills. In general, Montana Healthcare Programs follows the definitions in the CPT and HCPCS coding books. Unless otherwise specified, one unit equals one visit or one procedure. For specific codes, however, one unit may be 15 minutes, a percentage of body surface area, or another quantity. Always check the long text of the code description. A service must take at least 8 minutes to bill one unit of service if the procedure has “per 15 minutes” in its description.
End of Surveillance and Utilization Review Chapter
Appendix A: Forms
The forms listed below and others are available on the Forms page of the Montana Healthcare Programs Provider Information website. See the left menu on https://medicaidprovider.mt.gov.
- Presumptive Eligibility Notice of Decision
- Montana Healthcare Programs Incurment Notice
- Montana Healthcare Programs Form Order
- Individual Adjustment Request Form
- Paperwork Attachment Cover Sheet
- Provider Address Correction Form
- Blanket Denial
End of Appendix A: Forms Chapter
Appendix B: Place of Service Codes
End of Appendix B: Place of Service Codes Chapter
Appendix C: County Offices of Public Assistance
See the DPHHS webpage https://dphhs.mt.gov/hcsd/OfficeofPublicAssistance.
End of Appendix C: County Offices of Public Assistance Chapter
Definitions and Acronyms
End of Definitions and Acronyms Chapter
Index
Previous editions of this manual contained an index.
This edition has three search options.
- Search the whole manual. Open the Complete Manual pane. From your keyboard press the Ctrl and F keys at the same time. A search box will appear. Type in a descriptive or key word (for example "Denials". The search box will show all locations where denials discussed in the manual.
- Search by Chapter. Open any Chapter tab (for example the "Billing Procedures" tab). From your keyboard press the Ctrl and F keys at the same time. A search box will appear. Type in a descriptive or key word (for example "Denials". The search box will show where denials discussed in just that chapter.
- Site Search. Search the manual as well as other documents related to a particular search term on the Montana Healthcare Programs Site Specific Search page.
End of Index Chapter
End of General Information for Providers Manual