School-Based Services Manual
Printing the manual material found at this website for long-term use is not advisable. Department Policy material is updated periodically and it is the responsibility of the users to check and make sure that the policy they are researching or applying has the correct effective date for their circumstances.
If you experience any difficulty opening a section or link from this page, please email the webmaster.
How to Search this manual:
This edition has three search options.
- Search the whole manual. Open the Complete Manual pane. From your keyboard press the Ctrl and F keys at the same time. A search box will appear. Type in a descriptive or key word (for example "Denials". The search box will show all locations where denials discussed in the manual.
- Search by Chapter. Open any Chapter tab (for example the "Billing Procedures" tab). From your keyboard press the Ctrl and F keys at the same time. A search box will appear. Type in a descriptive or key word (for example "Denials". The search box will show where denials discussed in just that chapter.
- Site Search. Search the manual as well as other documents related to a particular search term on the Montana Healthcare Programs Site Specific Search page.
Prior manuals may be located through the provider website archives.
Updated 04/14/2022
School-Based Services Manual
To print this manual, right click your mouse and choose "print". Printing the manual material found at this website for long-term use is not advisable. Department Policy material is updated periodically and it is the responsibility of the users to check and make sure that the policy they are researching or applying has the correct effective date for their circumstances.
Update Log
Publication History
This publication supersedes all previous School-Based Services handbooks. Published by the Montana Department of Public Health & Human Services, August 2003.
Updated October 2003, December 2003, January 2004, April 2004, August 2004, April 2005, May 2005, August 2005, January 2006, April 2006, February 2007, April 2008, June 2011, April 2012, March 2013, May 2013, October 2017, November 2017, December 2017, January 2020, March 2020, March 2022, and April 2022.
CPT codes, descriptions and other data only are copyright 1999 American Medical Association (or such other date of publication of CPT). All Rights Reserved. Applicable FARS/DFARS Apply.
Update Log
04/14/2022
- Removed Nurse First Advice Line references.
- Updated Index to Search Options.
03/25/2022
- Removed CSCT references where no longer applicable.
03/26/2020
- Added language that services may be performed by a therapy assistant or therapy aide within their scope of practice but must be billed to Montana Healthcare Programs under the school’s supervising licensed therapist’s NPI.
- Clarified that Telehealth services are available for Physical Therapy, Occupational Therapy and Speech Therapy.
- Removed levels of supervision for speech, occupational, and physical therapy aides and assistants as these requirements fall under the purview of the Board of Speech-Language Pathologists and Audiologists, Montana Board of Occupational Therapy Practice and Montana Board of Physical Therapy Examiners respectively.
- Under Billing for Specific Services, Therapy Services, removed the discussion regarding supervision for aides/assistants for the reason noted above.
01/01/2020
- Cost Share references removed from the Billing Procedures, Submitting A Claim, Remittance and Advices, How Payment is Calculated, Definitions and Acronyms Chapters.
- Term "Medicaid" replaced with "Montana Healthcare Programs" throughout the manual.
- Terms "client" and "patient" replaced with "member".
- Health Improvement Program (HIP) references removed.
12/11/2017
Code changes were made in the Billing Procedures Chapter
11/02/2017
Code changes were made in the Billing Procedures Chapter.
10/20/2017
School-Based Services Manual converted to an HTML format and adapted to 508 Accessibility Standards.
07/10/2013
School-Based Services, May 2013: Entire Manual
These replacement pages includes a terminology change (client to member); however, unless a paragraph also included content changes, it is not marked as a change.
04/27/2012
School-Based Services, April 2012: Covered Services
06/09/2011
School-Based Services, June 2011: Covered Services
09/16/2008
School-Based Services, April 2008: Key Contacts, Covered Services, Billing Procedures, and Claim Instructions
02/14/2007
School-Based Services, February 2007: Revised Physician Order Information, New Private Duty Nursing Request Form
04/25/2006
School-Based Services, April 2006: Coordination of Benefits Information
01/17/2006
School-Based Services, January 2006: Documentation Requirements, Restricted CSCT Services, Private-Duty Nursing Review Requirements, and School-Based Services Codes
10/06/2005
School-Based Services, August 2005: Covered Services and Billing Information for CSCT and Therapy
05/12/2005
School-Based Services, May 2005: Key Contacts and Place of Service
04/11/2005
School-Based Services, April 2005: Key Contacts
08/30/2004
School-Based Services, August 2004: Audiology Services Defined
04/26/2004
School-Based Services, April 2004: Key Contacts and Websites, Covered Services, COB, Billing Procedures, Claim Forms, RAs and Adjustments, Forms and Definitions
01/14/2004
School-Based Services, January 2004: Covered Services Error Correction
12/23/2003
School-Based Services, December 2003:CSCT Changes
End of Update Log Chapter
Table of Contents
Key Contacts
Key Websites
Introduction
Covered Services
General Coverage Principles
Services for Children (ARM 37.86.2201–2221)
Services within Scope of Practice (ARM 37.85.401)
Provider Requirements
IEP Requirements
Member Qualifications
School Qualifications
Physician Order/Referral
Documentation Requirements
Noncovered Services (ARM 37.85.207 and 37.86.3002)
Importance of Fee Schedules
Coverage of Specific Services
Assessment to Initiate an IEP
Therapy Services
Private Duty Nursing Services
School Psychologists and Mental Health Services
Personal Care Paraprofessional Services
Special Needs Transportation
Audiology
Orientation and Mobility Specialist Services
Authorization Requirements Summary
Other Programs
Passport to Health Program
What Is Passport to Health? (ARM 37.86.5101–5120, 37.86.5303, and 37.86.5201–5206)
Passport to Health Primary Care Case Management (ARM 37.86.5101–5120)
Team Care (ARM 37.86.5303)
Other Programs
Prior Authorization
What Is Prior Authorization (ARM 37.86.5101–5120)
Getting Questions Answered
Other Programs
Coordination of Benefits
When Members Have Other Coverage
Identifying Other Sources of Coverage
When a Member Has Medicare
Medicare Part B Crossover Claims
When Medicare Pays or Denies a Service
When Montana Healthcare Programs Does Not Respond to Crossover Claims
Submitting Medicare Claims to Montana Healthcare Programs
When a Member Has TPL (ARM 37.85.407)
Billing for Montana Healthcare Programs Covered Services When No IEP Exists
Billing for Montana Healthcare Programs Covered Services under an IEP
Exceptions to Billing Third Party First
Requesting an Exemption
When the Third Party Pays or Denies a Service
When the Third Party Does Not Respond
Billing Procedures
Claim Forms
Timely Filing Limits (ARM 37.85.406)
Tips to Avoid Timely Filing Denials
When Providers Cannot Bill Montana Healthcare Programs Members (ARM 37.85.406)
Member Co-Payment (ARM 37.85.204 and 37.85.402)
Billing for Members with Other Insurance
Billing for Retroactively Eligible Members
Service Fees
Coding Tips
Using Modifiers
Multiple Services on the Same Date
Time and Units
Place of Service
Billing for Specific Services
Assessment to Initiate an IEP
Therapy Services
Private Duty Nursing Services
School Psychologists and Mental Health Services
Personal Care Paraprofessional Services
Special Needs Transportation
Audiology
Submitting Electronic Claims
Billing Electronically with Paper Attachments
Submitting Paper Claims
Claim Inquiries
The Most Common Billing Errors and How to Avoid Them
Other Programs
Submitting a Claim
CMS-1500 Agreement
Avoiding Claim Errors
Other Programs
Remittance Advices and Adjustments
The Remittance Advice
Sample Remittance Notice
Credit Balances
Rebilling and Adjustments
How Long Do I Have to Rebill or Adjust a Claim?
Rebilling Montana Healthcare Programs
Adjustments
Mass Adjustments
Payment and the RA
How Payment Is Calculated
Overview
Payment for School-Based Services
Speech, Occupational and Physical Therapy Services
Private Duty Nursing
School Psychologist
Personal Care Paraprofessionals
How Payment Is Calculated on TPL Claims
How Payment Is Calculated on Medicare Crossover Claims
Appendix A: Forms
Individual Adjustment
Audit Preparation Checklist
Private Duty Nursing Services Request
Paperwork Attachment Cover Sheet
Appendix B: Personal Care Paraprofessional Services Documentation
Personal Care Paraprofessional Services Provided in Schools – Child Profile
Purpose
Procedure
Instructions
Task/Hour Guide Instructions
Purpose
Specific Tasks
Task/Hour Guide
Definitions and Acronyms
Index
End of Table of Contents Chapter
Key Contacts
Hours for Key Contacts are 8:00 a.m. to 5:00 p.m. Monday through Friday (Mountain Time), unless otherwise stated. The phone numbers designated “In state” will not work outside Montana.
Chemical Dependency
For coverage information and other details regarding chemical dependency treatment, write or call:
(406) 444-3964 Phone
Send written inquiries to:
Chemical Dependency Bureau
Addictive and Mental Disorders Division
DPHHS
P.O. Box 202905
Helena, MT 59620-2905
Claims
Send paper claims and adjustment requests to:
Claims Processing Unit
P.O. Box 8000
Helena, MT 59604
Direct Deposit Arrangements
Providers who would like to receive their electronic remittance advices and electronic funds transfer should fax their information to Provider Relations:
(406) 442-4402 Fax
EDI Technical Help Desk
(800) 987-6719 In/Out of state
(406) 442-1837 Helena
(406) 442-4402 Fax
Montana EDI
P.O. Box 4936
Helena, MT 59604
Healthy Montana Kids (HMK)
(877) 543-7669 Phone (toll-free)
(877) 418-4533 Fax (toll-free)
(406) 444-6971 Phone (Helena)
(406) 444-4533 Fax (Helena)
Send email inquires to: hmk@mt.gov
HMK Program Officer
P.O. Box 202951
Helena, MT 59620-2951
Member Eligibility
There are several methods for verifying member eligibility. For details on each, see Verifying Member Eligibility in the Member Eligibility and Responsibilities chapter of the General Information for Providers manual.
FaxBack
(800) 714-0075 (24 hours)
Voice Response System
(800) 362-8312 (24 hours)
https://mtaccesstohealth.portal.conduent.com/mt/general/home.do
Medifax EDI
(800) 444-4336, X 2072 (24 hours)
Member Help Line
Members who have general Montana Healthcare Programs or Passport
questions may call the Help Line:
(800) 362-8312 Phone
Send written inquiries to:
Passport to Health
P.O. Box 254
Helena, MT 59624-0254
Prior Authorization
The following are some of the Department’s prior authorization contractors. Providers are expected to refer to their specific provider manual for prior authorization instructions.
Mountain-Pacific Quality Health
For prior authorization for school-based private duty nursing services and for prior authorization continued stay reviews for selected behavioral health services:
(406) 443-4020 X150 Helena
(800) 262-1545 X150 Outside Helena
(406) 443-4585 Fax
Send written inquiries to:
Medicaid Utilization Review
Mountain-Pacific Quality Health
Helena, MT 59602
For questions regarding prior authorization for medical necessity therapy reviews:
(406) 457-3060 Local
(877) 443-4021 Toll-free
(877) 443-2580 Fax local/long distance
Send written inquiries to:
Mountain Pacific Quality Health
3404 Cooney Drive
Helena, MT 59602
Provider Policy Questions
For policy questions, contact the appropriate division of the Department of Public Health and Human Services; see the Introduction chapter in the General Information for Providers manual. For inquiries related to licensure/endorsement, contact the Quality Assurance Division, Licensing Bureau:
(406) 444-2676 Phone
(406) 444-1742 Fax
Send written inquiries to:
Quality Assurance Division
Licensing Bureau
2401 Colonial Drive, Third Floor
Helena, MT 59602-2693
Provider Relations
For general claims questions, questions about eligibility, Passport to Health, payments, and denials:
(800) 624-3958 In/Out of state
(406) 442-1837 Helena
(406) 442-4402 Fax
Send e-mail inquiries to MTPRHelpdesk@conduent.com
Send written inquiries to:
Provider Relations Unit
P.O. Box 4936
Helena, MT 59604
Secretary of State
The Secretary of State’s office publishes the most current version of the Administrative Rules of Montana (ARM):
(406) 444-2055 Phone
Secretary of State
P.O. Box 202801
Helena, MT 59620-2801
Surveillance/Utilization Review
To report suspected provider fraud/abuse:
(406) 444-4586
(800) 376-1115
To report suspected member fraud/abuse:
(800) 201-6308
Send written inquiries to:
Fraud and Abuse
SURS
2401 Colonial Drive
P.O. Box 202953
Helena, MT 59620-2953
Team Care Program
For questions regarding Team Care:
(406) 444-9673 Phone
(406) 444-1861 Fax
Team Care Program Officer
Managed Care Bureau
DPHHS
P.O. Box 202951
Helena, MT 59620-2951
Third Party Liability
For questions about private insurance, Medicare, or other third-party liability:
(800) 624-3958 In/Out of state
(406) 442-1837 In/Out of state
Send written inquiries to:
Third Party Liability Unit
P.O. Box 5838
Helena, MT 59604
End of Key Contacts Chapter
Key Websites
EDI Gateway - https://edisolutionsmmis.portal.conduent.com/gcro/
Information Available:
EDI Gateway is Montana’s HIPAA clearinghouse. Visit this website for more information on:
- EDI enrollment
- EDI support
- FAQs
- Manuals
- Provider services
- Related links
- Software
Information Available:
- Information on Healthy Montana Kids (HMK)
https://mtaccesstohealth.portal.conduent.com/mt/general/home.do
Provider Information Website - medicaidprovider.mt.gov
Information Available:
- FAQs
- Fee schedules
- HIPAA update
- Key contacts
- Links to other websites
- Montana Healthcare Programs forms
- Montana Healthcare Programs news
- Newsletters
- Notices and manual replacement pages
- Passport to Health information
- Provider enrollment
- Provider manuals
- Remittance advice notices
- Training resources
- Upcoming events
Washington Publishing Company - www.wpc-edi.com
A fee is charged for documents; however, code lists are viewable online at no charge.
Information Available:
- HIPAA guides
- HIPAA tools
End of Key Websites Chapter
Introduction
Thank you for your willingness to serve members of the Montana Healthcare Programs and other medical assistance programs administered by the Department of Public Health and Human Services.
Manual Organization
This manual provides information specifically for the School-Based Services Program.
Most chapters have a section titled Other Programs that includes information about other Department programs such as the Mental Health Services Plan (MHSP) and Healthy Montana Kids (HMK). Other essential information for providers is contained in the separate General Information for Providers manual. Each provider is asked to review both the general manual and the specific manual for his/her provider type.
A table of contents and an index allow you to quickly find answers to most questions. The margins contain important notes with extra space for writing notes. There is a list of Key Contacts at the beginning of each manual. We have also included a space on the inside front cover to record your NPI for quick reference when calling Provider Relations.
Manual Maintenance
Manuals must be kept current. Changes to manuals are provided through provider notices and replacement pages. When replacing a page in a paper manual, file the old pages and notices in the back of the manual for use with claims that originated under the old policy. Provider notices and replacement pages are available on the Provider Information website. See Key Websites.
Providers are responsible for knowing and following current laws and regulations.
Rule References
Providers must be familiar with all current rules and regulations governing the Montana Healthcare Programs. Provider manuals are to assist providers in billing Montana Healthcare Programs; they do not contain all Montana Healthcare Programs rules and regulations. Rule citations in the text are a reference tool; they are not a summary of the entire rule. In the event that a manual conflicts with a rule, the rule prevails. Links to rule references are available on the Provider Information website. Paper copies of rules are available through the Secretary of State’s office. (See Key Contacts.)
The following rules and regulations are specific to the school-based services program. Additional Montana Healthcare Programs rule references are available in the General Information for Providers manual.
- Administrative Rules of Montana (ARM)
- ARM 37.86.2201 EPSDT Purpose, Eligibility and Scope
- ARM 37.86.2206–2207 EPSDT Medical and Other Services; Reimbursement
- ARM 37.86.2217 EPSDT Private Duty Nursing
- ARM 37.86.2230–2235 EPSDT, School-Based Health Related Services
Getting Questions Answered
The provider manuals are designed to answer most questions; however, questions may arise that require a call to a specific group (such as a program officer, Provider Relations, or a prior authorization unit). The list of Key Contacts at the front of this manual has important phone numbers and addresses pertaining to this manual. The Introduction chapter in the General Information for Providers manual also has a list of contacts for specific program policy information. Montana Healthcare Programs manuals, provider notices, replacement pages, fee schedules, forms, and much more are available on the Provider Information website. (See Key Websites.)
Claims Review (MCA 53-6-111, ARM 37.85.406)
The Department is committed to paying Montana Healthcare Programs providers’ claims as quickly as possible. Montana Healthcare Programs claims are electronically processed and usually are not reviewed by medical experts prior to payment to determine if the services provided were appropriately billed. Although the computerized system can detect and deny some erroneous claims, there are many erroneous claims it cannot detect. For this reason, payment of a claim does not mean the service was correctly billed or the payment made to the provider was correct. Periodic retrospective reviews are performed that may lead to the discovery of incorrect billing or incorrect payment. If a claim is paid and the Department later discovers the service was incorrectly billed or paid or the claim was erroneous in some other way, the Department is required by federal regulation to recover any overpayment, regardless of whether the incorrect payment was the result of Department or provider error or other cause (42 CFR 456.3).
Program Overview
Title XIX of the Social Security Act provides for a program of medical assistance to certain individuals and families with low income. This program, known as Montana Healthcare Programs, became law in 1965 as a jointly funded cooperative venture between the federal and state governments. Federal oversight for the Montana Healthcare Programs lies with the Centers for Medicare and Montana Healthcare Programs Services (CMS) in the Department of Public Health and Human Services (DPHHS).
The Early and Periodic Screening, Diagnosis, and Treatment (EPSDT) program is a special program for Montana Healthcare Programs beneficiaries under 21 years of age. The purpose of EPSDT is to ensure that through periodic checkups and early detection, children’s health problems are prevented and/or ameliorated. The EPSDT program allows states to provide services even if these services are not covered under the Montana Healthcare Programs state plan for other beneficiaries.
The Medicare Catastrophic Coverage Act, enacted in 1988, contained provisions which permit state Montana Healthcare Programs to provide reimbursement for health-related services provided as part of a child’s Individualized Education Plan (IEP). This reversed a previous policy that Montana Healthcare Programs could not reimburse for services provided by schools. As a result of this act, the State of Montana allows schools and cooperatives to bill for Montana Healthcare Programs services provided to Montana Healthcare Programs members pursuant to an IEP.
Montana Healthcare Programs reimburses health-related services provided by schools that are written into an IEP, if the services are covered under the Montana Healthcare Programs state plan or are covered under EPSDT. Services billed to Montana Healthcare Programs must be provided by qualified practitioners with credentials meeting state and federal Montana Healthcare Programs requirements. Montana Healthcare Programs provides reimbursement for health-related services and does not reimburse for services that are educational or instructional in nature.
Montana Healthcare Programs can be an important source of funding for schools, particularly because the cost of providing special education can greatly exceed the federal assistance provided under the Individuals with Disabilities Education Act (IDEA). Children who qualify for IDEA are frequently eligible for Montana Healthcare Programs services. Although Montana Healthcare Programs is traditionally the “payer of last resort” for health care services, it is required to reimburse for IDEA related medically necessary services for eligible children before IDEA funds are used.
In Montana, the Department of Public Health & Human Services, Montana Healthcare Programs Services Bureau, administers the Montana Healthcare Programs School-Based Services Program. This guide contains specific technical information about program requirements associated with seeking payment for covered services rendered in a school setting. The purpose of this guide is to inform schools on the appropriate methods for claiming reimbursement for the costs of health-related services provided.
End of Introduction Chapter
Covered Services
General Coverage Principles
Montana Healthcare Programs covers health-related services provided to children in a school setting when all of the following are met:
- The child qualifies for Individuals with Disabilities Education Act (IDEA).
- The services are written into an Individual Education Plan (IEP).
- The services are not free. Providers may not bill Montana Healthcare Programs for any services that are generally offered to all members without charge.
Refer to the IEP requirements in this chapter and the Coordination of Benefits chapter regarding billing services included/not included in a child’s IEP.
This chapter provides covered services information that applies specifically to school-based services. School-based services providers must meet the Montana Healthcare Programs
provider qualifications established by the state and have a provider agreement with the state. These providers must also meet the requirements specified in this manual and the General Information for Providers manual. School-based services provided to Montana Healthcare Programs members include the following:
- Therapy services (physical therapy, occupational therapy, speech language pathology)
- Audiology
- Private duty nursing
- School psychology and mental health services (including clinical social work and clinical professional counseling)
- Personal care (provided by paraprofessionals)
- Other diagnostic, preventative and rehabilitative services
- Specialized transportation
- Orientation and Mobility Specialist services (for blind and low vision)
Services for Children (ARM 37.86.2201–2221)
The Early and Periodic Screening, Diagnosis, and Treatment (EPSDT) Program is a comprehensive approach to health care for Montana Healthcare Programs members ages 20 and under. It is designed to prevent, identify, and then treat health problems before they become disabling. Under EPSDT, Montana Healthcare Programs eligible children may receive any medically necessary covered service, including all school-based services described in this manual. All applicable prior authorization requirements apply. (See the Prior Authorization chapter in this manual.)
Services within Scope of Practice (ARM 37.85.401)
Services provided under the School-Based Services Program are covered only when they are within the scope of the provider’s license.
Provider Requirements
Most school-based services must be provided by licensed health care providers. The exception is that activities of daily living services may be provided by personal care paraprofessionals. Montana Healthcare Programs does not cover services provided by a teacher or teacher’s aide; however, teachers or teacher aides may be used to assist in the development of child care planning. School-based services must be provided by only those providers listed in the table below.
Provider Requirements
Provider Type:
Private duty nursing services provided by:
- Licensed registered nurse
- Licensed practical nurse
Provider Requirements:
Nurses must have a valid certificate of registration issued by the Board of Nurse Examiners of the State of Montana or the Montana Board of Nursing Education and Nurse Registration.
Provider Type:
Mental health services provided by:
- Credentialed school psychologist
- Licensed psychologist
- Licensed clinical professional counselor
- Licensed clinical social worker
Provider Requirements:
Mental health providers must be licensed according to Montana’s state requirements. School psychologist services are provided by a professional with a Class 6 specialist license with a school psychologist endorsement.
Provider Type:
Therapy services provided by:
- Licensed occupational therapist
- Licensed physical therapist
- Licensed speech language pathologists
Provider Requirements:
These therapists are required to meet appropriate credentialing requirements as defined by the Montana Licensing Board.
Provider Type:
Audiology
Provider Requirements:
Must meet credentialing requirements as defined by the Montana Licensing Board.
Provider Type:
Personal care paraprofessional
Provider Requirements:
No licensing requirements.
Provider Type:
Orientation and Mobility Specialist
Provider Requirements:
Must have certification of the Academy for Certification of Vision Rehabilitation & Education Professionals (ACVREP) or a National Blindness Professional Certification (NOMC) from the National Blindness Professional Certification Board (NBPCB).
It is the responsibility of the school district to assure appropriately licensed providers perform all Montana Healthcare Programs covered services. Each school district must maintain documentation of each rendering practitioner’s license, certification, registration, or credential to practice in Montana. Montana Healthcare Programs providers who have had their license suspended by a state or federal government entity may not provide school-based services.
Services provided to Montana Healthcare Programs members must be documented in the member’s IEP.
IEP Requirements
Services provided to Montana Healthcare Programs members must be covered by Montana Healthcare Programs and documented in the member’s Individualized Education Plan (IEP), unless otherwise specified. School-based providers may bill Montana Healthcare Programs for Montana Healthcare Programs-covered health-related services provided to children with those services written into the IEP, even though the services may be provided to non-Montana Healthcare Programs children for free. However, if a child is covered by both Montana Healthcare Programs and private insurance, the private insurance must be billed prior to Montana Healthcare Programs. Exception to billing other insurance: Blue Cross and Blue Shield of Montana and HMK. Montana Healthcare Programs does not cover health-related services that are not included in an IEP unless all of the following requirements are met:
- Youth is enrolled in Montana Healthcare Programs.
- Services are medically necessary.
- A fee schedule is established for health-related services (can be a sliding scale to adjust for individuals with low incomes).
- The provider determines if each individual who receives services has insurance coverage or will be billed on a private-pay basis.
- The provider bills all individuals and/or the insurance carrier for the medical service provided.
Member Qualifications
To qualify for Montana Healthcare Programs school-based services, the member must be a Montana Healthcare Programs member and meet all the following criteria:
- Be Montana Healthcare Programs-eligible on the date of service.
- Be between the ages 3 and 20.
- Be entitled to school district services under the Individuals with Disabilities Education Act (IDEA).
- Have Montana Healthcare Programs reimbursable services referenced in his or her Individual Educational Plan (IEP). This shows that Montana Healthcare Programs covered services are recommended by the school district.
Cooperatives, joint boards, and non-public schools that do not receive state general funds for special education can not participate in the Montana Healthcare Programs as a school-based provider.
School Qualifications
Only public school districts, full-service education cooperatives and joint boards of trustees may enroll in the Montana Healthcare Programs School-Based Services Program. To qualify, the district, cooperative or joint board must receive special education funding from the state’s Office of Public Instruction general fund for public education. School districts include elementary, high school and K–12 districts that provide public educational services. Full-service education cooperatives and joint boards include those cooperatives eligible to receive direct state aid payments from the Superintendent of Public Instruction for special education services.
Schools That Employ Medical Service Providers:
- Schools that employ all or most of their medical service providers for whom the school submits bills can be enrolled with a single NPI for all services.
- Schools may use this single NPI to bill for any Montana Healthcare Programs covered service provided by a licensed provider.
- Schools that wish to have separate NPIs for each provider type (e.g., speech therapists, occupational therapists, and physical therapists) can request separate NPIs from the National Plan and Provider Enumeration System (NPPES).
Schools That Contract with External Medical Service Providers:
- Schools that contract with all or most of their providers must have the provider of service bill for each service they provide with their own individual NPI.
- Providers and schools can arrange with the Department for payments to be made to the school. If payments are assigned to the school, the school will also have the responsibility to collect third party liability payments on behalf of the service providers.
For more information on enrollment, visit the Provider Information website or contact Provider Enrollment. (See Key Contacts.)
Physician Order/Referral
Montana Healthcare Programs does not require physician orders or referrals for health-related services that are documented in the member’s IEP. The exception is private duty nursing services and personal care assistant services, which require a written order for private-duty nursing or physician signature for personal care assistance services. Other health-related services can be authorized by a licensed school practitioner meeting the State of Montana provider requirements to secure health-related services under an IEP.
Documentation Requirements
School-based service providers must maintain appropriate records. All case records must be current and available upon request. Records can be stored in any readily accessible format and location, and must be kept for six years and three months from the date of service. For more information on record keeping requirements, see the Surveillance/Utilization Review chapter in the General Information for Providers manual.
Medical documentation must include the following:
- Keep legible records.
- Date of service and the child’s name.
- The services provided during the course of each treatment and how the child responded.
- If the service is based on time units, (i.e., 15 minutes per unit), the provider of service should indicate begin and end times or the amount of time spent for each service. A service must take at least 8 minutes to bill one unit of service if the procedure has “per 15 minutes” in its description.
- Providers must sign and date each record documented on the day the medical service was rendered. Provider initials on daily records are acceptable providing their signature is included in other medical documentation within the child’s record.
- Documentation must, at least quarterly, include notes on member progress toward their goals. This is for the support of medical necessity and reviewing of the progress to maintain the rehabilitative nature of the service.
- The service provider must keep sufficient documentation to support the procedures billed to Montana Healthcare Programs. If a service is not documented, it did not happen.
- Documentation must not be created retroactively. Providers are responsible for maintaining records at the time of service.
The Montana Healthcare Programs School-Based Services Program is subject to both state and federal audits. As the Montana Healthcare Programs provider, the school certifies that the services being claimed for Montana Healthcare Programs reimbursement are medically necessary and furnished under the provider’s direction. Both fiscal and clinical compliance are monitored. In the event of adverse findings, the district/cooperative (not the mental health provider) will be held responsible for any paybacks to Montana Healthcare Programs. To assist in document retention for audit purposes, see the Audit Preparation Checklist on the Montana Healthcare Programs Provider Information website.
Noncovered Services (ARM 37.85.207)
The following is a list of services not covered by Montana Healthcare Programs.
- A provider’s time while attending member care meetings, Individual Educational Plan (IEP) meetings, individual treatment plan meetings, or member-related meetings with other medical professionals or family members.
- Services considered experimental or investigational.
- Services that are educational or instructional in nature.
- Services that are not medically necessary. The Department may review for medical necessity at any time before or after payment.
Use the current fee schedule for your provider type to verify coverage for specific services.
Importance of Fee Schedules
The easiest way to verify coverage for a specific service is to check the Department’s school-based services fee schedule. In addition to being listed on the fee schedule, all services provided must also meet the coverage criteria listed in the Provider Requirements chapter of the General Information for Providers manual and in this chapter. Use the fee schedule in conjunction with the more detailed coding descriptions listed in the CPT and HCPCS coding books. Take care to use the fee schedule and coding books that pertain to the date of service. Fee schedules are available on the Provider Information website. (See Key Websites.)
Coverage of Specific Services
The following are coverage rules for specific school-based services.
Assessment to Initiate an IEP
Montana Healthcare Programs covers medical evaluations (assessments) to develop an IEP as long as an IEP is subsequently established and health-related needs are identified.
Therapy Services
Therapy includes speech, occupational and physical therapy services. Services may be performed by a therapy assistant or therapy aide within their scope of practice but must be billed to Montana Healthcare Programs under the school’s supervising licensed therapist’s NPI. (See the Billing Procedures chapter in this manual.)
- Telehealth services are allowed for Physical Therapy, Occupational Therapy and Speech Therapy. All Montana Medicaid covered services delivered via telemedicine/telehealth are reimbursable so long as such services are medically necessary and clinically appropriate for delivery via telemedicine/telehealth.
Services Included
Covered therapy services include the following:
- Restorative therapy services when the particular services are reasonable and necessary to the treatment of the member’s condition and subsequent improvement of function. The amount and frequency of services provided must be indicated on the member’s IEP.
- Assessment services to determine member medical needs and/or to establish an IEP, as long as the assessment results in health-related services documented in the IEP.
Service Requirements
For all therapies being billed, they must be included in the student’s IEP.
Services Restricted
- Montana Healthcare Programs does not cover therapy services that are intended to maintain a member’s current condition but only covers services to improve member functions.
Private Duty Nursing Services
Private duty nursing services are skilled nursing services provided by a registered or licensed practical nurse.
Service Requirements
Montana Healthcare Programs covers private duty nursing services when all of the following requirements are met:
- When the member’s attending physician or mid-level practitioner orders these services in writing
- When prior authorization (PA) is obtained. (See the Prior Authorization chapter in this manual for PA requirements.)
School Psychologists and Mental Health Services
Psychological services in schools are based on determining eligibility for inclusion in special education programming and not necessarily to determine a medical diagnosis outside of the guidelines of the Individuals with Disabilities Education Act.
Services Included
Psychological and mental health services include the following:
- Individual psychological therapy.
- Psychological tests and other assessment procedures when the assessment results in health-related services being written into the IEP.
- Interpreting assessment results.
- Obtaining, integrating, and interpreting information about child behavior and conditions as it affects learning, if it results in an IEP. This only includes direct face-to-face service.
- Mental health and counseling services that are documented on the member’s IEP.
- Consultation with the child’s parent as part of the child’s treatment.
Service Requirements
Montana Healthcare Programs covers psychological counseling services when the following two criteria are met:
- The member’s IEP includes a behavior management plan that documents the need for the services.
- Service is not provided concurrently with CSCT services (unless prior authorization has been obtained).
Services Restricted
Montana Healthcare Programs does not cover the following psychological services:
- Testing for educational purposes
- Psychological evaluation, if provided to a child when an IEP is not subsequently established
- Review of educational records
- Classroom observation
- Scoring tests
Personal Care Paraprofessional Services
Personal care paraprofessional services are medically necessary in-school services provided to members whose health conditions cause them to be limited in performing activities of daily living. That is, these services are provided for members with functional limitations.
The school district must maintain documentation of each service provided, which may take the form of a trip log.
Services Included
These activities of daily living services include:
- Dressing
- Eating
- Escorting on bus
- Exercising (ROM)
- Grooming
- Toileting
- Transferring
- Walking
Service Requirements
- These services must be listed on the member’s IEP.
- Approval must be given by the member’s primary care provider prior to billing for Montana Healthcare Programs covered services. Billing for these services cannot be claimed until the primary care provider signs and dates the Child Profile form. Claiming can start on the date of the signature. This is done by use of the Child Profile Form located in Appendix B.
Services Restricted
Montana Healthcare Programs does not cover the following services provided by a personal care paraprofessional:
- Skilled care services that require professional medical personnel
- Instruction, tutoring or guidance in academics
- Behavioral management
See the Personal Care Paraprofessional Services Documentation, which includes the child profile and service delivery record. The child profile provides detailed examples of activities of daily living.
Montana Healthcare Programs does not cover special transportation services on a day that the member does not receive a Montana Healthcare Programs covered service that is written into the IEP.
Special Needs Transportation
Special needs transportation includes transportation services for members with special needs for the purpose of obtaining non-emergency medical services that are outside of traditional transportation services provided for members without disabilities.
Services Include
Special needs transportation services are covered when all of the following criteria are met:
- Transportation is provided to and/or from a Montana Healthcare Programs-covered service on the day the service was provided.
- The Montana Healthcare Programs-covered service is included in the member’s IEP.
- The member must be in need of a specialized wheelchair or subject to transport by stretcher.
Specialized transportation services are covered if one of the following conditions exists :
- A member requires transportation in a vehicle adapted to service the needs of students with disabilities, including a specially adapted school bus.
- A member resides in an area that does not have school bus transportation (such as those in close proximity to a school).
- The school incurs the expense of the service regardless of the type of transportation rendered.
Services Included
Special needs transportation includes the following:
- Transportation from the member’s place of residence to school (where the member receives health-related services covered by the Montana School-Based Services Program, provided by school), and/or return to the residence.
- Transportation from the school to a medical provider’s office who has a contract with the school to provide health-related services covered by the Montana School-Based Services Program, and return to school.
Services Restricted
Members with special education needs who ride the regular school bus to school with other non-disabled children in most cases will not have a medical need for transportation services and will not have transportation listed in their IEP. In this case, the bus ride should not be billed to the Montana School-Based Services Program. The fact that members may receive a medical service on a given day does not necessarily mean that special transportation also would be reimbursed for that day.
Audiology
Audiology assessments are performed by individuals possessing the state of Montana credentials for performing audiology services.
Services Included
Covered audiology services include the following:
- Assessment to determine member’s medical needs and/or to establish an IEP, as long as the assessment results in health-related services documented in the IEP.
- Services provided must be documented in the member’s IEP.
Service Requirements
Montana Healthcare Programs covers audiology services when the services to be provided during a school year are written into the child’s IEP.
Services Restricted
Montana Healthcare Programs does not cover the following audiology services:
- Testing for educational purposes.
- Services provided during Child Find assessments.
Orientation and Mobility Specialist Services
Orientation and Mobility Specialist services are medically necessary in-school services provided to students to alleviate movement deficiencies resulting from a lack of vision.
Orientation and Mobility Specialists need to have a certification by the Academy for Certification of Vision Rehabilitation and Education Professionals (ACVREP) or a National Orientation & Mobility Certification (NOMC) offered by the National Blindness Professional Certification Board (NBPCB). The credential is valid for a period of 5 years and is renewable by documenting work and/or participation in professional activities.
Services Included
Orientation & Mobility Specialist service include the following:
- Sensory integrative techniques to enhance sensory processing and promote adaptive responses to environmental demands, direct one-on-one member contact by provider. This includes assessment type services.
- Self-care/home management training (e.g., ADLs and compensatory training, instruction in use of assistive technology devices/adaptive equipment) direct one-on-one contact by provider.
- See School-Based fee schedule online for the correct CPT codes to use when billing.
Authorization Requirements Summary
The following table is a summary of authorization requirements for school-based services that were described in each section above. For more information on how to obtain prior authorization and Passport provider approval, see the Prior Authorization and Passport to Health chapters in this manual.
Authorization Requirements
Service: Therapy
Prior Authorization: No
Passport Provider Approval: No
Written Physician Order/Referral: No
Service: Private Duty Nursing
Prior Authorization: Yes
Passport Provider Approval: No
Written Physician Order/Referral: Yes
Service: School Psychologist and Mental Health
Prior Authorization: No
Passport Provider Approval: No
Written Physician Order/Referral: No
Service: Personal Care Paraprofessional
Prior Authorization: No
Passport Provider Approval: No
Written Physician Order/Referral: Yes (Child Profile Form is signed by child’s physician.)
Service: Specialized Transportation
Prior Authorization: No
Passport Provider Approval: No
Written Physician Order/Referral: No
Service: Audiology
Prior Authorization: No
Passport Provider Approval: No
Written Physician Order/Referral: No
Service: Orientation & Mobility
Prior Authorization: No
Passport Provider Approval: No
Written Physician Order/Referral: No
Other Programs
This is how the information in this chapter applies to Department programs other than School-Based Services outlined within this manual.
Children’s Mental Health Services
In addition to the school-based services outlined in this manual, the Children’s Mental Health Bureau (CMHB) offers Comprehensive School and Community treatment (CSCT) and other mental health services. Please contact CMHB at (406) 444-4545 for more information or click the following links:
Children's Mental Health Medicaid Services Provider Manual
Medicaid Mental Health for Youth Fee Schedule
Administrative Rules of Montana:
- 37.87: CHILDREN'S MENTAL HEALTH SERVICES
- 37.106: HEALTH CARE FACILITIES/Subchapter 19 Minimum Standards for Mental Health Centers
Healthy Montana Kids (HMK)
The school-based services in this manual are not covered benefits of Healthy Montana Kids (HMK). Additional information regarding HMK benefits is available by contacting Blue Cross and Blue Shield of Montana (BCBSMT) at 1-800-447-7828 (toll-free) or 406-447-7828 (Helena).
End of Covered Services Chapter
Passport to Health Program
What Is Passport to Health? (ARM 37.86.5101–5120, ARM 37.86.5303, and ARM 37.86.5201–5206)
Passport to Health is the managed care program for Montana Healthcare Programs and
Healthy Montana Kids (HMK) Plus members. The four Passport programs encourage
and support Montana Healthcare Programs and HM Plus members and providers in establishing a
medical home and in ensuring the appropriate use of Montana Healthcare Programs and HMK Plus services:
- Passport to Health Primary Care Case Management
- Team Care
Montana Healthcare Programs and HMK Plus members who are eligible for Passport must enroll in the program (about 70% of Montana Healthcare Programs and HMK Plus members are eligible) Each enrollee has a designated Passport provider who is typically a physician, mid-level practitioner, or primary care clinic.
Montana Healthcare Programs does not pay for services when prior authorization or Passport requirements are not met.
Passport to Health Primary Care Case Management (ARM 37.86.5101–5120)
The Passport provider provides primary care case management (PCCM) services to their members. This means he/she provides or coordinates the member’s care and makes referrals to other Montana Healthcare Programs and HMK Plus providers when necessary. Under Passport, Montana Healthcare Programs, and HMK Plus members choose one primary care provider (PCP) and develop an ongoing relationship that provides a medical home. The medical home is a concept that encourages a strong doctor–member relationship. An effective medical home is accessible, continuous, comprehensive, coordinated, and operates within the context of family and community.
With some exceptions, all services to Passport members must be provided or approved by the member’s Passport provider or Montana Healthcare Programs/HMK Plus will not reimburse for those services. The member’s Passport provider is also referred to as the PCP. (See the section titled Services That Do Not Require Passport Provider Approval in this chapter.)
Different codes are issued for Passport approval and prior authorization, and both must be recorded on the claim form, if appropriate.
Team Care (ARM 37.86.5303)
Team Care is designed to educate members to effectively access medical care. Members with a history of using services at an amount or frequency that is not medically necessary are enrolled in Team Care. Members enrolled in Team Care are also enrolled in Passport. Team Care follows the same Passport rules and guidelines for referrals, enrollment/disenrollment, prior authorization, and billing processes. However, while Passport members can change providers without cause, as often as once a month, Team Care members are locked in to one provider and one pharmacy. Providers are encouraged to make a referral to the Team Care Program Officer if they feel one of their members is appropriate for the program. A Passport provider receives an enhanced case management fee of $6 per member per month for Team Care members. When checking Montana Healthcare Programs or HMK Plus eligibility on the MATH web portal, a Team Care member’s provider and pharmacy will be listed. (See Key Websites.) Write all Montana Healthcare Programs and HMK Plus prescriptions to the designated pharmacy.
In practice, providers will most often encounter Montana Healthcare Programs and HMK Plus members who are enrolled in Passport. Specific services may also require prior authorization (PA) even if the member is a Passport enrollee. Specific PA requirements can be found in the provider fee schedules. For more information on Passport to Health, see the General Information for Providers manual.
Other Programs
Members who are enrolled in the Mental Health Services Plan (MHSP) or Healthy Montana Kids (HMK) are not enrolled in Passport, so the Passport requirements in this chapter do not apply.
For more HMK information, contact Blue Cross and Blue Shield of Montana at 1-800-447-7828 (toll-free) or 447-7828 (Helena) Additional HMK information is available on the HMK website. (See Key Websites.)
End of Passport to Health Program Chapter
Prior Authorization
Prior authorization refers to a list of services that require approval from the Montana Healthcare Program prior to the service being rendered. If a service requires prior authorization, the requirement exists for all Montana Healthcare Programs members. When prior authorization is granted, a prior authorization number is issued and must be on the claim.
Different codes are issued for Passport approval and prior authorization; when necessary, both must be on the claim form. Montana Healthcare Programs does not pay for services when prior authorization requirements are not met.
Prior Authorization for Retroactively Eligible Members
When a member is determined retroactively eligible for Montana Healthcare Programs, the member should give the provider a Notice of Retroactive Eligibility (160-M). The provider has 12 months from the date retroactive eligibility was determined to bill for those services. When a member becomes retroactively eligible for Montana Healthcare Programs the provider may:
- Accept the member as a Montana Healthcare Programs member from the current date.
- Accept the member as a Montana Healthcare Programs member from the date retroactive eligibility was effective.
- Require the member to continue as a private-pay member.
Providers may choose whether to accept retroactive eligibility. All prior authorization requirements must be met to receive Montana Healthcare Programs payment. When requesting prior authorization, attach a copy of the 160-M to the prior authorization request. It is the member’s responsibility to ensure his/her caseworker prepares a 160-M for each provider who participates in the member’s healthcare during this retroactive period. See the Billing Procedures chapter in this manual for retroactive eligibility billing requirements. When seeking prior authorization, keep in mind the following:
- The referring provider should initiate all authorization requests.
- Always refer to the current Montana Healthcare Programs fee schedule to verify if prior authorization is required for specific services.
- For a list of services that require prior authorization, who to contact, and documentation requirements, see the Contact Us link in site index in the Provider Information website menu. The Contact Us can be located in the site index in the left menu of the Provider Website.
- Prior authorization criteria forms for most services are available on the Forms page of the Provider Information website .
- When prior authorization is granted from Mountain-Pacific Quality Health (MPQH), providers receive notification from both MPQH and Conduent Claims Processing. The Prior Authorization Notice from Claims Processing has a prior authorization number which must be included on the claim.
End of Prior Authorization Chapter
Coordination of Benefits
When Members Have Other Coverage
Montana Healthcare Programs members often have coverage through Medicare, workers’ compensation, employment-based coverage, individually purchased coverage, etc. Coordination of benefits is the process of determining which source of coverage is the primary payer in a particular situation. In general, providers must bill other carriers before billing Montana Healthcare Programs, but there are some exceptions. (See Exceptions to Billing Third Party First later in this chapter.) Medicare coverage is processed differently than other sources of coverage.
Identifying Other Sources of Coverage
The member’s Montana Healthcare Programs eligibility verification may identify other payers such as Medicare or other third-party payers. (See Member Eligibility and Responsibilities in the General Information for Providers manual.) If a member has Medicare, the Medicare ID number is provided. If a member has other coverage (excluding Medicare), it will be shown under the TPL section.
Some examples of third-party payers include:
- Private health insurance
- Employment-related health insurance
- Workers’ compensation insurance*
- Health insurance from an absent parent
- Automobile insurance*
- Court judgments and settlements*
- Long-term care insurance
*These third-party payers (and others) may not be listed on the member’s Montana Healthcare Programs eligibility verification.
Providers must use the same procedures for locating third party sources for Montana Healthcare Programs members as for their non-Montana Healthcare Programs members. Providers cannot refuse service because of a third party payer or potential third-party payer.
When a Member Has Medicare
Medicare claims are processed and paid differently than claims involving other payers. The other sources of coverage are referred to as third-party liability (TPL), but Medicare is not.
Medicare Part B Crossover Claims
Medicare Part B covers outpatient hospital care, physician care, and other services including those provided in a school setting. The Department has an agreement with Medicare Part B carrier for Montana (Noridian) and the Durable Medical Equipment Regional Carrier [DMERC]). Under this agreement, the carrier provide the Department with a magnetic tape of claims for members who have both Medicare and Montana Healthcare Programs coverage. Providers must tell Medicare that they want their claims sent to Montana Healthcare Programs automatically and must have their NPI on file with Montana Healthcare Programs.
To avoid confusion and paperwork, submit Medicare Part B crossover claims to Montana Healthcare Programs only when necessary.
In these situations, providers need not submit Medicare Part B crossover claims to Montana Healthcare Programs. Medicare will process the claim, submit it to Montana Healthcare Programs, and send the provider an Explanation of Medicare Benefits (EOMB). Providers must check the EOMB for the statement indicating that the claim has been referred to Montana Healthcare Programs for further processing. It is the provider’s responsibility to follow up on crossover claims and make sure they are correctly billed to Montana Healthcare Programs within the timely filing limit. (See Billing Procedures.)
When Medicare Pays or Denies a Service
- When Medicare automatic crossover claims are paid or denied, they should automatically cross over to Montana Healthcare Programs for processing, so the provider does not need to submit the claim to Montana Healthcare Programs.
- When Medicare crossover claims are billed on paper and are paid or denied, the provider must submit the claim to Montana Healthcare Programs with the Medicare EOMB (and the explanation of denial codes).
When submitting electronic claims with paper attachments, see the Billing Electronically with Paper Attachments section of the Billing Procedures chapter in this manual.
When Montana Healthcare Programs Does Not Respond to Crossover Claims
When Montana Healthcare Programs does not respond within 45 days of the provider receiving the Medicare EOMB, submit a claim with a copy of the Medicare EOMB to Montana Healthcare Programs for processing.
Submitting Medicare Claims to Montana Healthcare Programs
When submitting a paper claim to Montana Healthcare Programs, use Montana Healthcare Programs billing instructions and codes. Medicare’s instructions, codes, and modifiers may not be the same as Montana Healthcare Programs’s. The claim must include the provider’s NPI and Montana Healthcare Programs member ID number. The Medicare EOMB and explanation of denial codes are required only if the claim was denied.
Remember to submit Medicare crossover claims to Montana Healthcare Programs only when:
- The referral to Montana Healthcare Programs statement is missing from the provider’s EOMB.
- The provider does not hear from Montana Healthcare Programs within 45 days of receiving the Medicare EOMB.
- Medicare denies the claim.
All Part B crossover claims submitted to Montana Healthcare Programs before Medicare’s 45-day response time will be returned to the provider.
When a Member Has TPL (ARM 37.85.407)
When a Montana Healthcare Programs member has additional medical coverage (other than Medicare), it is often referred to as third party liability (or TPL). In most cases, providers must bill other insurance carriers before billing Montana Healthcare Programs.
If a parent determines that billing their insurance would cause a financial hardship (e.g., decrease lifetime coverage or increase premiums), and refuses to let the school bill the insurance plan, the school cannot bill Montana Healthcare Programs for these services based on requirements of IDEA.
Providers are required to notify their members that any funds the member receives from third party payers equal to what Montana Healthcare Programs paid (when the services were billed to Montana Healthcare Programs) must be turned over to the Department. Amounts in excess of what Montana Healthcare Programs paid must be returned to the provider. The following words printed on the member’s statement will fulfill this requirement: “When services are covered by Montana Healthcare Programs and another source, any payment the member receives from the other source must be turned over to Montana Healthcare Programs.”
If a parent refuses to let the school bill their insurance plan, Montana Healthcare Programs cannot be billed either.
Billing for Montana Healthcare Programs Covered Services When No IEP Exists
In order to bill for Montana Healthcare Programs covered services that are not in the member’s IEP, the school must meet all the following requirements:
- A fee schedule is established for health-related services (can be a sliding scale to adjust for individuals with low incomes)
- The provider determines if each individual who receives services has insurance coverage or will be billed on a private-pay basis
- The provider bills all individuals and/or the insurance carrier for the medical service provided
If the school bills private pay members, then they must bill as follows for the services provided:
Member Insurance Status: Montana Healthcare Programs only*
Billing Process: Bill Montana Healthcare Programs
Member Insurance Status: Private pay, no Montana Healthcare Programs
Billing Process: Bill family
Member Insurance Status: Private insurance/Montana Healthcare Programs*
Billing Process: Bill private insurance before Montana Healthcare Programs
Member Insurance Status: Private insurance, no Montana Healthcare Programs*
Billing Process: Bill private insurance
*Note: Under FERPA, schools must have written parental permission for release of information before billing Montana Healthcare Programs. For billing third party insurances, schools must have written permission for billing and written permission for release of information.
Billing for Montana Healthcare Programs Covered Services under an IEP
If a child is covered by both Montana Healthcare Programs and private insurance, and the services are provided under an IEP, providers must bill as follows:
Member Insurance Status: Montana Healthcare Programs only*
Billing Process: Bill Montana Healthcare Programs
Member Insurance Status: Private pay, no Montana Healthcare Programs
Billing Process: Not required to bill family
Member Insurance Status: Private insurance/Montana Healthcare Programs*
Billing Process: Bill private insurance before Montana Healthcare Programs
Member Insurance Status: Private insurance, no Montana Healthcare Programs
Billing Process: Not required to bill private insurance
*Note: Under FERPA, schools must have written parental permission for release of information before billing Montana Healthcare Programs. For billing third party insurances, schools must have written permission for billing and written permission for release of information.
Exceptions to Billing Third Party First
In a few cases, providers may bill Montana Healthcare Programs first.
- When a Montana Healthcare Programs member is also covered by Indian Health Service (IHS) or the Montana Crime Victims Compensation Fund, providers must bill Montana Healthcare Programs before IHS or Crime Victims. These are not considered third party liability.
- When a child is covered under BCBSMT or HMK, providers may bill Montana Healthcare Programs first since these insurances do not cover services provided in a school setting.
- Montana Healthcare Programs must be billed before IDEA funds are used.
- Effective April 1, 2013, when a child is also covered by another insurance, and the service is provided by a school-based provider, no blanket denial form is required nor is any information from the third-party liability.
Requesting an Exemption
Providers may request to bill Montana Healthcare Programs first under certain circumstances. In each of these cases, the claim and required information must be sent directly to the TPL Unit. (See Key Contacts.)
- If another insurance has been billed, and 90 days have passed with no response, include a note with the claim explaining that the insurance company has been billed, or include a copy of the letter sent to the insurance company. Include the date the claim was submitted to the insurance company and certification that there has been no response.
- When the provider has billed the third-party insurance and has received a non-specific denial (e.g., no member name, date of service, amount billed), submit the claim with a copy of the denial and a letter of explanation directly to Montana Healthcare Programs in order to avoid missing the timely filing deadline.
- When the Child Support Enforcement Division has required an absent parent to have insurance on a child, the claim can be submitted to Montana Healthcare Programs when the following requirements are met:
- The third-party carrier has been billed, and 30 days or more have passed since the date of service.
- The claim is accompanied by a certification that the claim was billed to the third-party carrier, and payment or denial has not been received.
When the Third-Party Pays or Denies a Service
When a third-party payer is involved (excluding Medicare) and the other payer:
- Pays the claim, indicate the amount paid in the “prior payments” form locator of the claim when submitting to Montana Healthcare Programs for processing.
- Allows the claim, and the allowed amount went toward member’s deductible, include the insurance EOB when billing Montana Healthcare Programs.
- Denies the claim, include a copy of the denial (including the denial reason codes) with the claim and submit to Montana Healthcare Programs. If a blanket denial is provided, the Department will accept and allow this denial for a period of no more than two years. The school must include a copy of this blanket denial with each submission for health-related services for each member. The blanket denial must be specific to the provider, member, and health related services provided to the member. Blanket denials issued to schools without a member’s name will not be accepted.
- Denies a line on the claim, bill the denied lines together on a separate claim and submit to Montana Healthcare Programs. Include the explanation of benefits (EOB) from the other payer as well as an explanation of the reason for denial (e.g., definition of denial codes).
If the provider receives a payment from a third party after the Department has paid the provider, the provider must return the lower of the two payments to the Department within 60 days.
When the Third Party Does Not Respond
If another insurance has been billed and 90 days have passed with no response, bill Montana Healthcare Programs as follows:
- Include a note with the claim explaining that the insurance company has been billed, or include a copy of the letter sent to the insurance company.
- Include the date the claim was submitted to the insurance company.
- Send this information to the Third-Party Liability Unit. (See Key Contacts.)
End of Coordination of Benefits Chapter
Billing Procedures
Claim Forms
Services provided by the health care professionals covered in this manual must be billed either electronically on a Professional claim or on a CMS-1500 paper claim form. CMS-1500 forms are available from various publishing companies; they are not available from the Department or Provider Relations.
Timely Filing Limits (ARM 37.85.406)
Providers must submit clean claims to Montana Healthcare Programs within:
Twelve months from whichever is later:
- the date of service
- the date retroactive eligibility or disability is determined
For claims involving Medicare or TPL, if the 12-month time limit has passed, providers must submit clean claims to Montana Healthcare Programs.
- Medicare Crossover Claims: Six months from the date on the Medicare explanation of benefits approving the service (if the Medicare claim was timely filed and the member was eligible for Medicare at the time the Medicare claim was filed).
- Claims Involving Other Third-Party Payers (excluding Medicare): Six months from the date on an adjustment notice from a third party payer who has previously processed the claim for the same service, and the adjustment notice is dated after the periods described above.
Clean claims are claims that can be processed without additional information or action from the provider. The submission date is defined as the date that the claim was received by the Department or the claims processing contractor. All problems with claims must be resolved within this 12-month period.
Tips to Avoid Timely Filing Denials
- Correct and resubmit denied claims promptly (see the Remittance Advices and Adjustments chapter in this manual).
- If a claim submitted to Montana Healthcare Programs does not appear on the remittance advice within 45 days, contact Provider Relations for claim status. (See Key Contacts.)
- If another insurer has been billed and 90 days have passed with no response, you can bill Montana Healthcare Programs. (See the Coordination of Benefits chapter in this manual for more information.)
- To meet timely filing requirements for Medicare/Montana Healthcare Programs crossover claims, see the Coordination of Benefits chapter in this manual.
When Providers Cannot Bill Montana Healthcare Programs Members (ARM 37.85.406)
In most circumstances, providers may not bill Montana Healthcare Programs members for services covered under Montana Healthcare Programs.
More specifically, providers cannot bill members directly:
- For the difference between charges and the amount Montana Healthcare Programs paid.
- For a covered service provided to a Montana Healthcare Programs-enrolled member who was accepted as a Montana Healthcare Programs member by the provider, even if the claim was denied.
- When the provider bills Montana Healthcare Programs for a covered service, and Montana Healthcare Programs denies the claim because of billing errors.
- When a third-party payer does not respond.
- When a member fails to arrive for a scheduled appointment.
- When services are free to the member and free to non-Montana Healthcare Programs covered individuals.
If a provider bills Montana Healthcare Programs and the claim is denied because the member is not eligible, the provider may bill the member directly.
Member Co-Payment (ARM 37.85.204 and 37.85.402)
Effective for all claims paid on or after January 1, 2020 co-payment will not be assessed.
Billing for Members with Other Insurance
If a Montana Healthcare Programs member is also covered by Medicare, has other insurance, or some other third party is responsible for the cost of the member’s health care, see the Coordination of Benefits chapter in this manual.
Billing for Retroactively Eligible Members
When a member becomes retroactively eligible for Montana Healthcare Programs, the provider may:
- Accept the member as a Montana Healthcare Programs member from the current date.
- Accept the member as a Montana Healthcare Programs member from the date retroactive eligibility was effective.
- Require the member to continue as private pay.
When the provider accepts the member’s retroactive eligibility, the provider has 12 months from the date retroactive eligibility was determined to bill for those services. When submitting claims for retroactively eligible members, attach a copy of the FA-455 (eligibility determination letter) to the claim if the date of service is more than 12 months earlier than the date the claim is submitted. Providers may need to contact the member’s local office of public assistance. (See the General Information for Providers manual.)
When a provider chooses to accept the member from the date retroactive eligibility was effective, and the member has made a full or partial payment for services, the provider must refund the member’s payment for the services before billing Montana Healthcare Programs for the services.
Service Fees
The Office of Management and Budget (OMB A-87) federal regulation specifies one government entity may not bill another government entity more than their cost. Schools should bill Montana Healthcare Programs their cost of providing a service, not the fee published by Montana Healthcare Programs for the service. The Montana Healthcare Programs fee schedule is to inform provider of the maximum fee Montana Healthcare Programs pays for each procedure.
Coding Tips
The procedure codes listed in the following table are valid procedures for schools to use for billing Montana Healthcare Programs.
School-Based Services Codes
Occupational Therapist
Service: Occupational therapy – individual therapeutic activities
CPT Code: 97530
Unit Measurement: 15-minute unit
Service: Occupational therapy – group therapeutic procedures
CPT Code: 97150
Unit Measurement: Per visit
Service: Occupational therapy evaluation - low 20 minutes
CPT Code: 97165
Unit Measurement: Per visit
Service: Occupational therapy evaluation - moderate - 30 minutes
CPT Code: 97166
Unit Measurement: Per visit
Service: Occupational therapy evaluation - high - 45minutes
CPT Code: 97167
Unit Measurement: Per visit
Service: Occupational therapy re-evaluation
CPT Code: 97168
Unit Measurement: Per visit
Physical Therapist
Service: Physical therapy – individual therapeutic activities
CPT Code: 97530
Unit Measurement: 15-minute unit
Service: Physical therapy – group therapeutic procedures
CPT Code: 97150
Unit Measurement: Per visit
Service: Physical therapy evaluation - low - 20 minutes
CPT Code: 97161
Unit Measurement: Per visit
Service: Physical therapy evaluation - moderate - 30 minutes
CPT Code: 97162
Unit Measurement: Per visit
Service: Physical therapy evaluation - high 45 minutes
CPT Code: 97163
Unit Measurement: Per visit
Service: Physical therapy re-evaluation
CPT Code: 97164
Unit Measurement: Per visit
Speech Therapists
Service: Treatment of Speech Disorder; individual
CPT Code: 92507
Unit Measurement: Per visit
Service: Treatment of Speech Disorder; group
CPT Code: 92508
Unit Measurement: Per visit
Service: Evaluation of speech fluency
CPT Code: 92521
Unit Measurement: Per visit
Service: Evaluation of speech sound production
CPT Code: 92522
Unit Measurement: Per visit
Service: Evaluation of speech sound with language comprehension
CPT Code: 92523
Unit Measurement: Per visit
Private Duty Nursing
Service: Private duty nursing services provided in school
CPT Code: T1000
Unit Measurement: 15-minute unit
School Psychologist/Mental Health Services
Service: Psychological therapy – individual
CPT Code: 90832
Unit Measurement: Per 30-minute unit
Service: Psychological therapy – group
CPT Code: 90853
Unit Measurement: Per visit
Service: Psychological testing by Psychologist
CPT Code: 96101
Unit Measurement: Per 1 hour
Personal Care Paraprofessionals
Service: Personal care services
CPT Code: T1019
Unit Measurement: 15-minute unit
Special Needs Transportation
Service: Special needs transportation
CPT Code: T2003
Unit Measurement: Per one-way trip
Audiology
Service: Comprehensive Hearing Test
CPT Code: 92557
Unit Measurement: Per visit
Service: Tympanometry
CPT Code: 92567
Unit Measurement: Per visit
Service: Evoked otoacoustic emission; limited
CPT Code: 92587
Unit Measurement: Per visit
Orientation & Mobility
Service: Sensory integrative techniques
CPT Code: 97533
Unit Measurement: 15-minute unit
Service: Self-care/home management training
CPT Code: 97535
Unit Measurement: 15-minute unit
Using Modifiers
School-based services providers only use modifiers for coding when the service provided to a member is not typical. The modifiers are used in addition to the CPT codes. The following modifiers may be used in schools:
- Modifier 52 is billed with the procedure code when a service is reduced from what the customary service normally entails. For example, a service was not completed in its entirety as a result of extenuating circumstances or the well-being of the individual was threatened.
- Modifier 22 is billed with the procedure code when a service is greater than the customary service normally entails. For example, this modifier may be used when a service is more extensive than usual or there was an increased risk to the individual. Slight extension of the procedure beyond the usual time does not validate the use of this modifier.
- Modifier 59 is billed for therapies in accordance with the Correct Coding Initiative (CCI) and to be used when codes are considered mutually exclusive or a component of one another.
- Modifiers may also be required when providing two services in the same day that use the same code. See the section titled Multiple Services on the Same Date” for more information.
Multiple Services on the Same Date
When a provider bills Montana Healthcare Programs for two services that are provided on the same day that use the same CPT code and are billed under the same NPI and taxonomy, a modifier should be used to prevent the second service from being denied. The modifier GO is used for occupational therapy, and modifier GP is used for physical therapy. One of the codes needs to have modifier 59 also for the CCI edit. For example, a school bills with one NPI and taxonomy for all services. The school provided occupational therapy for a member in the morning, and physical therapy for the same member in the afternoon of October 14, 2003. The claim would be billed like this:
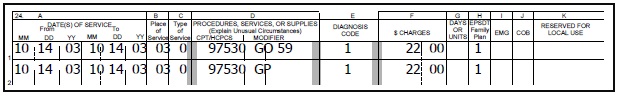
Time and Units
- A provider may bill only time spent directly with a member. Time spent traveling to provide a service and paperwork associated with the direct service cannot be included in the time spent providing a service.
- Some CPT codes are designed to bill in units of 15 minutes (or other time increment) and others are per visit.
- If the service provided is using a per visit code, providers should use one unit of service per visit.
- When using codes that are based on a 15-minute time unit, providers should bill one unit of service for each 15-minute period of service provided. Units round up to the next unit after 8 minutes.
Place of Service
The only place of service code Montana Healthcare Programs will accept is “03” (schools).
Billing for Specific Services
The following are instructions for billing for school-based services. For details on how to complete a CMS-1500 claim form, see the Submitting a Claim chapter in this manual.
School-based providers can only bill services in the amount, scope, and duration listed in the IEP.
Assessment to Initiate an IEP
When billing for assessments (evaluations), use the CPT code for the type of service being billed. When the unit measurement is “per visit,” only one unit may be billed for the assessment/evaluation. If the evaluation is completed over the course of several days, it is considered one evaluation. Bill the date span with 1 unit of service, not multiple units of service. For example, a speech/hearing evaluation completed over a three-day period would be billed like this:
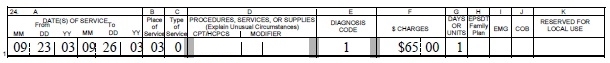
A two-hour psychological assessment (evaluation) would be billed like this (the unit measurement for this code is “per hour”):
Therapy Services
Services may be performed by a therapy assistant or therapy aide but must be billed to Montana Healthcare Programs under the school’s NPI and taxonomy. Remember to use the CCI edit modifier for all three types of therapy: speech, occupational and physical. See the Submitting a Claim chapter in this manual. Thirty minutes of individual physical therapy would be billed like this (the unit measurement for this code is “15-minute unit”):
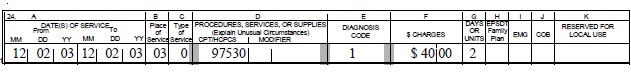
Private Duty Nursing Services
Prior authorization is required for these services, so remember to include the prior authorization number on the claim. (See the Submitting a Claim chapter in this manual.) Private duty nursing services provided for 15 minutes would be billed like this:
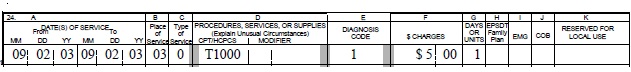
Montana Healthcare Programs covered services provided under an IEP are exempt from the “free care rule.”
School Psychologists and Mental Health Services
A psychological therapy session of 30 minutes would be billed like this (the unit measurement for this code is per 30-minute unit):
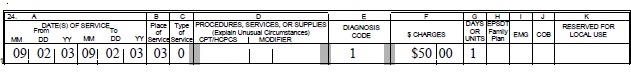
Personal Care Paraprofessional Services
Personal care services provided to a member for 2 hours during a day would be billed like this (the unit measurement for this code is per 15-minute unit):
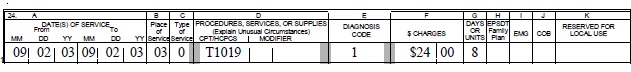
Special Needs Transportation
School districts must maintain documentation of each service provided, which may take the form of a trip log. Schools must bill only for services that were provided. Special transportation should be billed on a per one-way trip basis. For example, if a member was transported from his/her residence to school and received Montana Healthcare Programs covered health-related services that day, and then transported back to his/her residence, it would be billed like this:
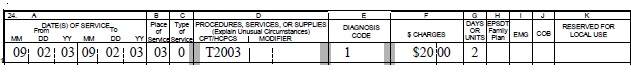
Audiology
An audiology assessment would be billed like this (the unit measurement for this code is per visit):
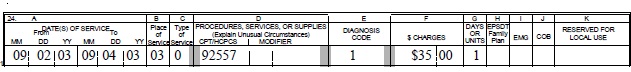
Submitting Electronic Claims
Providers who submit claims electronically experience fewer errors and quicker payment. Claims may be submitted using the methods below. For detailed submission methods, see the electronic submissions manual on the Electronic Billing page of the website.
- WINASAP 5010. This free software provided by Conduent allows for the creation of basic claim submissions. Please note that this software is not compatible with Windows 10 and has limited support as it is free software.
- Utilizes either a dial-up modem or submissions through the Montana Access to Health (MATH) Web Portal.
- Requires completion of the X12N Transaction Packet to allow for claim submissions.
- Clearinghouses/Contracted Claim Submitter. Providers can make arrangements with a clearinghouse/contracted claim submitter for claim submission. Please note that the clearinghouse must be enrolled to submit claims to Montana Healthcare Programs.
- Montana Access to Health (MATH) Web Portal . A secure website that allows providers to verify eligibility, check claim status, and view medical claims history. Valid X12N files can be uploaded through this website.
- MoveIt DMZ. This secure transfer protocol is for providers and clearinghouses that submit large volumes of files (in excess of 20 per day) or are regularly submitting files larger than 2 MB. This utilizes SFTP and an intermediate storage area for the exchange of files.
- A request for this must be made through Conduent Provider Relations for established trading partners.
Providers should be familiar with federal rules and regulations related to electronic claims submission. For more information on electronic claims submission options, contact Provider Relations or the EDI Technical Help Desk. (See the Key Contacts chapter.) Providers should be familiar with federal rules and regulations and Montana-specific information for sending and receiving electronic transactions. They are available on the EDI Gateway website. (See Key Websites.)
Billing Electronically with Paper Attachments
When submitting claims that require additional supporting documentation, the Attachment Control Number field must be populated with an identifier. Identifier formats can be designed by software vendors or clearinghouses, but the preferred method is the provider’s NPI followed by the member’s ID number and the date of service, each separated by a dash:
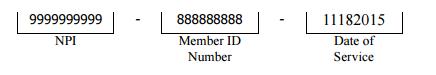
The supporting documentation must be submitted with a paperwork attachment cover sheet. See the Forms page of the Provider Information website. The number in the paper Attachment Control Number field must match the number on the cover sheet.
Submitting Paper Claims
For instructions on completing a paper claim, see the Submitting a Claim chapter in this manual. Unless otherwise stated, all paper claims must be mailed to:
Claims Processing
P.O. Box 8000
Helena, MT 59604
Claim Inquiries
Contact Provider Relations for claim questions, or questions regarding payments, denials, member eligibility.
Provider Relations will respond to the inquiry within 10 days. The response will include the status of the claim, paid (date paid), denied (date denied), or in process. Denied claims will include an explanation of the denial and steps to follow for payment (if the claim is payable).
The Most Common Billing Errors and How to Avoid Them
Paper claims are often returned to the provider before they can be processed, and many other claims (both paper and electronic) are denied.
To avoid unnecessary returns and denials, double check each claim to confirm the following items are included and accurate.
Common Billing Errors
Reasons for Return or Denial: Provider NPI missing or invalid
How to Prevent Returned or Denied Claims: The provider NPI is a 10-digit number assigned to the provider by the National Plan and Provider Enumeration System. Verify the correct provider NPI is on the claim.
Reasons for Return or Denial: Authorized signature missing
How to Prevent Returned or Denied Claims: Each claim must have an authorized signature belonging to the provider, billing clerk, or office personnel. The signature may be typed, stamped, hand-written, or computer generated.
Reasons for Return or Denial: Signature date missing
How to Prevent Returned or Denied Claims: Each claim must have a signature date.
Reasons for Return or Denial: Incorrect claim form used
How to Prevent Returned or Denied Claims: The claim must be the correct form for the provider type. Services covered in this manual require a CMS-1500 claim form (or electronic Professional claim).
Reasons for Return or Denial: Information on claim form not legible
How to Prevent Returned or Denied Claims: Information on the claim form must be legible. Use dark ink and center the information in the form locator. Information must not be obscured by lines.
Reasons for Return or Denial: Member number not on file, or member was not eligible on date of service
How to Prevent Returned or Denied Claims: Before providing services to the member, verify member eligibility by using one of the methods described in the Member Eligibility and Responsibilities chapter of the General Information for Providers manual. Montana Healthcare Programs eligibility may change monthly.
Reasons for Return or Denial: Prior authorization number is missing
How to Prevent Returned or Denied Claims: Prior authorization (PA) is required for certain services, and the PA number must be on the claim. See the Prior Authorization chapters in this manual.
Reasons for Return or Denial: Prior authorization does not match current information
How to Prevent Returned or Denied Claims: Claims must be billed and services performed during the prior authorization span. The claim will be denied if it is not billed according to the spans on the authorization.
Reasons for Return or Denial: Duplicate claim
How to Prevent Returned or Denied Claims: Check all remittance advices (RAs) for previously submitted claims before resubmitting. When making changes to previously paid claims, submit an adjustment form rather than a new claim (see the Remittance Advices and Adjustments chapter in this manual).
Reasons for Return or Denial: TPL on file and no credit amount on claim
How to Prevent Returned or Denied Claims: If the member has any other insurance (or Medicare), bill the other carrier before Montana Healthcare Programs. See the Coordination of Benefits chapter in this manual. If the member’s TPL coverage has changed, providers must notify the TPL unit (see the Key Contacts chapter) before submitting a claim.
Reasons for Return or Denial: Claim past 12-month filing limit
How to Prevent Returned or Denied Claims: The Claims Processing Unit must receive all clean claims and adjustments within the timely filing limits described in this chapter. To ensure timely processing, claims and adjustments must be mailed to Claims Processing at the address shown in the Key Contacts chapter.
Reasons for Return or Denial: Missing Medicare EOMB
How to Prevent Returned or Denied Claims: All denied Medicare crossover claims must have an Explanation of Medicare Benefits (EOMB) with denial reason codes attached, and be billed to Montana Healthcare Programs on paper.
Reasons for Return or Denial: Provider is not eligible during dates of services, enrollment has lapsed due to licensing requirements, or provider NPI terminated
How to Prevent Returned or Denied Claims: Out-of-state providers must update licensure for Montana Healthcare Programs enrollment early to avoid denials. If enrollment has lapsed due to expired licensure, claims submitted with a date of service after the expiration date will be denied until the provider updates his or her enrollment. New providers cannot bill for services provided before Montana Healthcare Programs enrollment begins. If a provider is terminated from the Montana Healthcare Programs, claims submitted with a date of service after the termination date will be denied.
Reasons for Return or Denial: Procedure is not allowed for provider type
How to Prevent Returned or Denied Claims: Provider is not allowed to perform the service. Verify the procedure code is correct using current HCPCS and CPT billing manual. Check the appropriate Montana Healthcare Programs fee schedule to verify the procedure code is valid for your provider type.
Other Programs
The Mental Health Services Plan (MHSP) and Healthy Montana Kids (HMK) do not cover school-based services. For more information on these programs, visit the Provider Information website.
End of Billing Procedures Chapter
Submitting a Claim
The services described in this manual are billed either electronically on a Professional claim or on a CMS-1500 paper claim form. Claims submitted with all of the necessary information are referred to as “clean” and are usually paid in a timely manner (see the Billing Procedures chapter in this manual). When completing a claim, remember the following:
- Required fields are indicated by *. For detailed submission methods, see the electronic submissions manual on the Electronic Billing page of the website
- Fields that are required if the information is applicable to the situation or member are indicated by **.
- Field 24h, EPSDT/Family Planning, is used as an indicator to specify additional details for certain members or services. The following are accepted codes:
EPSDT/Family Planning Indicator
Code: 1 Member/Service: EPSDT
Purpose: Overrides some benefit limits for member under age 21.
Code: 2 Member/Service: Family planning
Purpose: Overrides the Montana Healthcare Programs Passport authorization on the line.
Code: 3 Member/Service: EPSDT and family planning
Purpose: Overrides Montana Healthcare Programs cost sharing and Passport authorization for persons under the age of 21.
Code: 6 Member/Service: Nursing facility member
Purpose: Overrides the Medicare edit for oxygen services on the line.
- Unless otherwise stated, all paper claims must be mailed to the following address:
Claims Processing Unit
P.O. Box 8000
Helena, MT 59604
Sample Claim
Member Information
Field: 2*
Field Title: Member's Name
Instructions: Enter member's name as seen on member’s Montana Health Care Programs information
Field: 10d *
Field Title: Member’s ID
Instructions: Enter the member’s ID number as it appears on the member’s Montana Health Care Programs information.
Field: 1a, 9a, 11**
Field Title: Member’s ID
Instructions: If member’s ID is not located in 10d these three fields are searched for the number.
Field: 24h*
Field Title: EPSDT Family Planning
Instructions: When billing electronically, use “Y.” When billing on paper, use “1.”
Provider Information
Field: 24a shaded area
Field Title: NDC
Instructions: Enter the qualifier, N4, followed by the NDC (NDC should not have punctuation, dashes or spaces), units qualifier and units as described by the qualifier
Field: 24i shaded**
Field Title: ID Qualifier
Instructions: ZZ for the Taxonomy qualifier.
Field: 24j shaded**
Field Title: Taxonomy Code
Instructions: Enter the Taxonomy code for the rendering provider.
Field: 24j **
Field Title: NPI, Rendering Prov
Instructions: Enter NPI Number for the rendering provider.
Field: 31*
Field Title: Signature and Date
Instructions: Enter Signature and Date.
Field: 33*
Field Title: Billing Provider Info
Instructions: Enter Physical Address with a 9 digit ZIP code and phone number.
Field: 33a*
Field Title: NPI #
Instructions: Enter NPI number for billing/pay-to provider.
Field: 33b*
Field Title: Taxonomy #
Instructions: Enter the qualifier (ZZ) and the billing provider's taxonomy code.
Billing Information
Field: 21.1 - 21.4*
Field Title: Diagnosis codes Enter at least one diagnosis.
Field: 24a*
Field Title: Date(s) of Service
Instructions: Enter the dates of service include beginning and ending date even if same.
Field: 24b*
Field Title: Place of Service
Instructions: Enter the code for place of service.
Field: 24c**
Field Title: EMG
Instructions: Emergency Indicator if applicable.
Field: 24d*
Field Title: Procedure Code
Instructions: Enter the procedure code used. Enter modifiers if applicable.
Field: 24e*
Field Title: Diagnosis Pointer
Instructions: Enter the corresponding diagnosis pointer (1,2,3,or 4) that refers to the codes in field 21
Field: 24f*
Field Title: Charges
Instructions: Enter the total charge for this line
Field: 24g*
Field Title: Days/Units
Instructions: Enter the days or units used for the procedure.
Field: 28*
Field Title: Total Charges
Instructions: Enter total charges from all line items.
*Required Field **Required if applicable
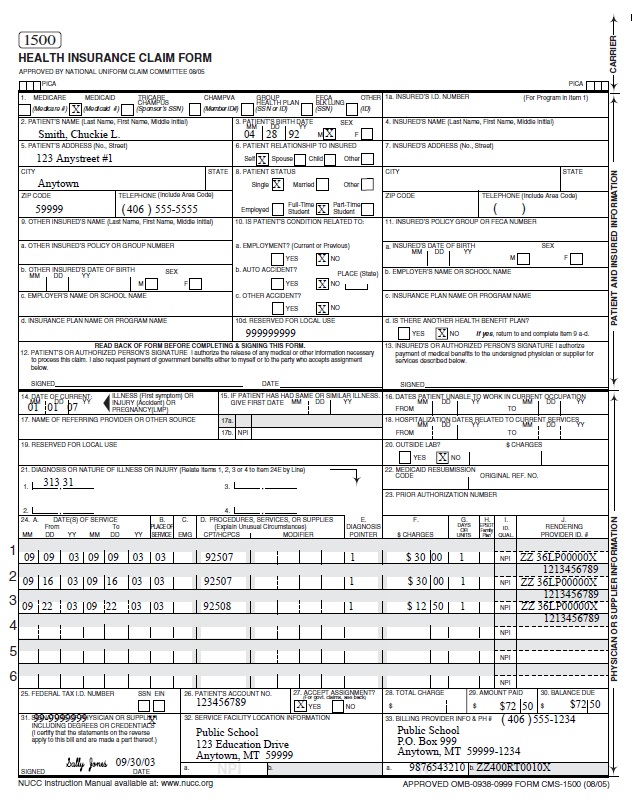
CMS-1500 Agreement
Your signature on the CMS-1500 constitutes your agreement to the terms presented on the back of the form. This form is subject to change by the Centers for Medicare and Montana Healthcare Programs Services (CMS).
Avoiding Claim Errors
Claims are often denied or even returned to the provider before they can be processed. To avoid denials and returns, double-check each claim to confirm the following items are accurate. For more information on returned and denied claims, see the Billing Procedures chapter in this manual.
Common Claim Errors
Claim Error: Required field is blank
Prevention: Check the claim instructions earlier in this chapter for required fields (indicated by * or **). If a required field is blank, the claim may either be returned or denied.
Claim Error: Member ID number missing or invalid
Prevention: This is a required field (field 10d); verify that the member’s Montana Healthcare Programs ID number is listed as it appears on the member’s ID card.
Claim Error: Member name missing
Prevention: This is a required field (field 2); check that it is correct.
Claim Error: Provider NPI missing or invalid
Prevention: The provider NPI is a 10-digit number assigned to the provider by the National Plan and Provider Enumeration System. Verify the correct provider NPI is on the claim.
Claim Error: Prior authorization number missing
Prevention: When prior authorization (PA) is required for a service, the PA number must be listed on the claim in field 23. (See the Prior Authorization chapter in this manual.)
Claim Error: Not enough information regarding other coverage
Prevention: Fields 1a and 11d are required fields when a member has other coverage. (Refer to the examples earlier in this chapter.)
Claim Error: Authorized signature missing
Prevention: Each claim must have an authorized signature belonging to the provider, billing clerk, or office personnel. The signature may be typed, stamped, or hand-written.
Claim Error: Signature date missing
Prevention: Each claim must have a signature date. Incorrect claim form used Services covered in this manual require a CMS-1500 claim form (or electronic Professional claim).
Claim Error: Information on claim form not legible
Prevention: Information on the claim form must be legible. Use dark ink and center the information in the field. Information must not be obscured by lines.
Claim Error: Medicare EOMB not attached
Prevention: When Medicare is involved in payment on a claim, the Medicare EOMB must be attached to the claim or it will be denied.
Other Programs
This chapter also applies to claims forms completed for MHSP services and Healthy Montana Kids (HMK) eyeglass services.
End of Submitting a Claim Chapter
Remittance Advices and Adjustments
The Remittance Advice
The Remittance Advice (RA) is the best tool providers have to determine the status of a claim. RAs accompany payment for services rendered. The RA provides details of all transactions that have occurred during the previous RA cycle. Each line of the RA represents all or part of a claim, and explains whether the claim or service has been paid, denied, or suspended (also referred to as pending).
The pending claims section of the RA is informational only. Do not take any action on claims displayed here.
If the claim was suspended or denied, the RA also shows the reason.
To access the MATH web portal, you must first complete a Provider Enrollment Form and an Trading Partner Agreement (see the following table). To receive an electronic RA, the provider must complete a Trading Partner Agreement and register for the Montana Access to Health (MATH) web portal. You can access your electronic RA through the MATH web portal by going to the Provider Information website and selecting Log in to Montana Access to Health.
After these forms have been processed, you will receive a user ID and password that you can use to log on to the web portal. The verification process also requires a provider ID, a submitter ID, and a tax ID number. Each provider must complete an EDI Trading Partner Agreement, but if there are several providers in one location who are under one tax ID number, they can use one submitter number. These providers should enter the submitter ID in both the provider number and submitter ID fields. Otherwise, enter the provider number in the provider number field.
If a claim was denied, read the description of the EOB before taking any action on the claim.
RAs are available in PDF format. You can read, print, or download PDF files using Adobe Acrobat Reader, which is available on the Provider Information website. Due to space limitations, each RA is only available for 90 days.
Electronic RAs are available for only 90 days on the web portal.
The RA is divided into the following sections:
Sections of the Paper RA
Section: RA Notice
Description: The RA Notice is on the first page of the remittance advice. This section contains important messages about rate changes, revised billing procedures, and many other items that may affect providers and claims.
Section: Paid Claims
Description: This section shows claims paid during the previous cycle. It is the provider’s responsibility to verify that claims were paid correctly. If Montana Healthcare Programs overpays a claim and the problem is not corrected, it may result in an audit requiring the provider to return the overpayment plus interest. If a claim was paid at the wrong amount or with incorrect information, the claim must be adjusted. (See Adjustments later in this chapter.)
Section: Denied Claims
Description: This section shows claims denied during the previous cycle. If a claim has been denied, refer to the Reason/Remark column (Field 18). The Reason and Remark Code Description located at the end of the RA explains why the claim was denied. See the section titled The Most Common Billing Errors and How to Avoid Them in the Billing Procedures chapter.
Section: Pending Claims
Description: All claims that have not reached final disposition will appear in this area of the paper RA (pended claims are not available on X12N 835 transactions). The RA uses suspended and pending interchangeably. They both mean that the claim has not reached final disposition. If a claim is pending, refer to the Reason/Remark Code section (Field 18) located at the end of the RA will explain why the claim is suspended. This section is informational only. Do not take any action on claims displayed here. Processing will continue until each claim is paid or denied.
Claims shown as pending with Reason Code 133 require additional review before a decision to pay or deny is made. If a claim is being held while waiting for member eligibility information, it may be suspended for a maximum of 30 days. If Montana Healthcare Programs receives eligibility information within the 30-day period, the claim will continue processing. If no eligibility information is received within 30 days, the claim will be denied. When a claim is denied for lack of eligibility, the provider should verify that the correct Montana Healthcare Programs ID number was billed. If the ID number was incorrect, resubmit the claim with the correct ID number.
Section: Credit Balance Claims
Description: Credit balance claims are shown here until the credit has been satisfied.
Section: Gross Adjustments
Description: Any gross adjustments performed during the previous cycle are shown here.
Section: Reason and Remark Code Description
Description: This section lists the reason and remark codes that appear throughout the RA with a brief description of each.
Sample Remittance Notice
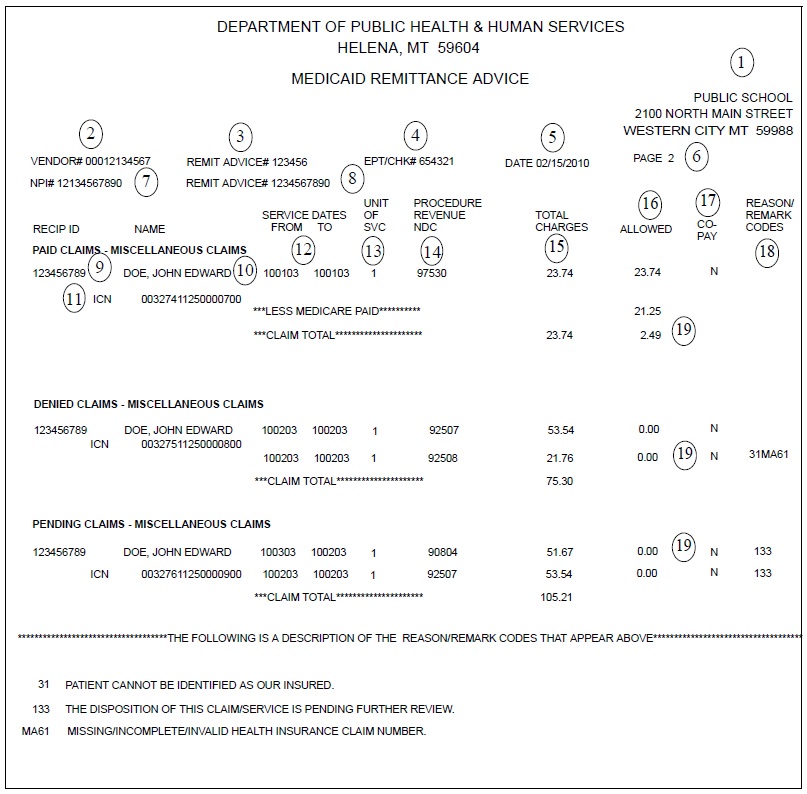
Key Fields on the Remittance Advice
Field: 1. Provider name and address
Description: Provider’s business name and address as recorded with the Department.
Field: 2. Vendor #
Description: The 7-digit number assigned to the provider.
Field: 3. Remittance advice number
Description: The remittance advice number.
Field: 4. EFT/Check number
Description: The EFT or check number of payment
Field: 5. Date
Description: The date the RA was issued.
Field: 6. Page number
Description: The page number of the RA.
Field: 7. NPI
Description: A unique 10-digit identification number required by HIPAA for all U.S. health care providers. Providers must use their NPI to identify themselves in all HIPAA transactions.
Field: 8. Taxonomy
Description: Alphanumeric code that indicates the provider’s specialty.
Field: 9. Member ID
Description: The member’s Montana Healthcare Programs ID number.
Field: 10. Name
Description: The member’s name.
Field: 11. Internal control number (ICN)
Description: Each claim is assigned a unique 17-digit number (ICN). Use this number when you have any questions concerning your claim. The claim number represents the following information:
0 00111 11 123 000123
A B C D E
A = Claim medium
0 = Paper claim
2 = Electronic claim
3 = Encounter claim
4 = System generated claim (mass adjustment, nursing home turn-around
document, or point-of-sale (POS) pharmacy claim)
6 = Pharmacy
B = Julian date (e.g. April 20, 2000 was the 111th day of 2000)
C = Microfilm number
00 = Electronic claim
11 = Paper claim
D = Batch number
E = Claim number
If the first number is:
0 = Regular claim
1 = Negative side adjustment claim (Montana Healthcare Programs recovers payment)
2 = Positive side adjustment claim (Montana Healthcare Programs reprocesses)
Field: 12. Service dates
Description: Dates services were provided. If services were performed in a single day, the same date will appear in both columns.
Field: 13. Unit of service
Description: The units of service rendered under this procedure or NDC code.
Field: 14. Procedure/Revenue/NDC
Description: The procedure code (CPT or HCPCS), National Drug Code (NDC), or revenue code will appear in this column. If a modifier was used, it will also appear in this column.
Field: 15. Total charges
Description: The amount a provider billed for this service.
Field: 16. Allowed
Description: The Montana Healthcare Programs allowed amount.
Field: 18. Reason and remark codes
Description: A code which explains why the specific service was denied or pended. Descriptions of these codes are listed at the end of the RA.
Field: 19. Deductions, billed amount, and paid amount
Description: Any deductions, such as third-party liability are listed first. The amount the provider billed is next, followed by the amount of Montana Healthcare Programs reimbursement.
Credit Balances
Credit balances occur when claim adjustments reduce original payments causing the provider to owe money to the Department. These claims are considered in process and continue to appear on the RA until the credit has been satisfied.
The credit balance section is informational only. Do not post from credit balance statements.
Credit balances can be resolved in two ways:
- By working off the credit balance. Remaining credit balances can be deducted from future claims. These claims will continue to appear on consecutive RAs until the credit has been paid.
- By sending a check payable to DPHHS for the amount owed. This method is required for providers who no longer submit claims to Montana Healthcare Programs. Attach a note stating that the check is to pay off a credit balance and include your NPI. Send the check to the attention of the Third-Party Liability Unit at the address in Key Contacts.
Rebilling and Adjustments
Rebillings and adjustments are important steps in correcting any billing problems you may experience. Knowing when to use the rebilling process versus the adjustment process is important.
Montana Healthcare Programs does not accept any claim for resubmission or adjustment after 12 months from the date of service (see Timely Filing Limits in Billing Procedures chapter).
How Long Do I Have to Rebill or Adjust a Claim?
- Providers may resubmit or adjust any initial claim within the timely filing limits described in the Billings Procedure chapter of this manual.
- These time periods do not apply to overpayments that the provider must refund to the Department. After the 12-month time period, a provider may not refund overpayments to the Department by completing a claim adjustment. The provider may refund overpayments by issuing a check or asking the TPL unit to complete a gross adjustment.
Rebilling Montana Healthcare Programs
Rebilling is when a provider submits a claim to Montana Healthcare Programs that was previously submitted for payment but was either returned or denied. Claims are often returned to the provider before processing because key information such as NPI and taxonomy or authorized signature and date are missing or unreadable. For tips on preventing returned or denied claims, see the Billing Procedures and Submitting a Claim chapters.
When to Rebill Montana Healthcare Programs
- Claim Denied. Providers can rebill Montana Healthcare Programs when a claim is denied in full, as long as the claim was denied for reasons that can be corrected. When the entire claim is denied, check the Reason and Remark Code/Description, make the appropriate corrections, and resubmit the claim (not an adjustment).
Rebill denied claims only after appropriate corrections have been made.
- Line Denied. When an individual line is denied on a multiple-line claim, correct any errors and rebill Montana Healthcare Programs. Do not use an adjustment form.
- Claim Returned. Rebill Montana Healthcare Programs when the claim is returned under separate cover. Occasionally, Montana Healthcare Programs is unable to process the claim and will return it to the provider with a letter stating that additional information is needed to process the claim. Correct the information as directed and resubmit your claim.
How to Rebill
- Check any Reason and Remark Code listed and make your corrections on a copy of the claim, or produce a new claim with the correct information.
- When making corrections on a copy of the claim, remember to cross out or omit all lines that have already been paid. The claim must be neat and legible for processing.
- Enter any insurance (TPL) information on the corrected claim, or include insurance denial information, and submit to Montana Healthcare Programs.
Adjustments
If a provider believes that a claim has been paid incorrectly, the provider may call Provider Relations or submit a claim inquiry for review. (See the Billing Procedures chapter, Claim Inquiries.) Once an incorrect payment has been verified, the provider may submit an Individual Adjustment Request to Provider Relations. If incorrect payment was the result of a Conduent keying error, contact Provider Relations.
When adjustments are made to previously paid claims, the Department recovers the original payment and issues appropriate repayment. The result of the adjustment appears on the provider’s RA as two transactions. The original payment will appear as a credit transaction. The replacement claim reflecting the corrections will be listed as a separate transaction and may or may not appear on the same RA as the credit transaction. The replacement transaction will have nearly the same ICN number as the credit transaction, except the 12th digit will be a 2, indicating an adjustment. See Key Fields on the Remittance Advice earlier in this chapter. Adjustments are processed in the same time frame as claims.
Adjustments can only be made to paid claims.
When to request an adjustment
- Request an adjustment when a claim was overpaid or underpaid.
- Request an adjustment when a claim was paid but the information on the claim was incorrect (e.g., member ID, provider NPI, date of service, procedure code, diagnoses, units).
How to Request an Adjustment
To request an adjustment, use the Individual Adjustment Request form. The requirements for adjusting a claim are as follows:
- Claims Processing must receive individual claim adjustment requests within 12 months from the date of service (see Timely Filing Limits in the Billing Procedures chapter).After this time, gross adjustments are required (see Definitions).
- Use a separate adjustment request form for each ICN.
- If you are correcting more than one error per ICN, use only one adjustment request form, and include each error on the form.
- If more than one line of the claim needs to be adjusted, indicate which lines and items need to be adjusted in the Remarks section of the adjustment form.
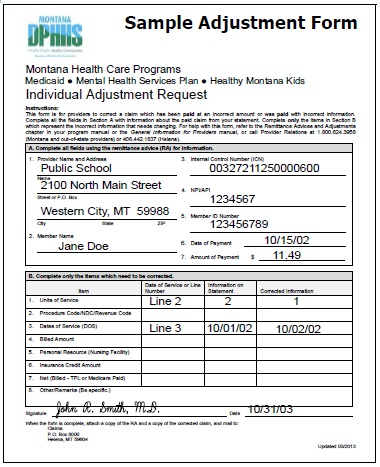
Completing an Adjustment Request Form
- Download the Individual Adjustment Request from the Provider Information website. (See Key Websites.) Complete Section A with provider and member information and the claim’s ICN number.
- Complete Section B with information about the claim. Fill in only the items that need to be corrected:
- Enter the date of service or the line number in the Date of Service or Line Number column.
- Enter the information from the claim that was incorrect in the Information on Statement column.
- Enter the correct information in the Corrected Information column.
- Attach copies of the RA and a corrected claim if necessary.
- If the original claim was billed electronically, a copy of the RA will suffice.
- If the RA is electronic, attach a screen print of the RA.
- Verify the adjustment request has been signed and dated.
- Send the adjustment request to Claims Processing. (See Key Contacts.)
- If an original payment was an underpayment by Montana Healthcare Programs, the adjustment will result in the provider receiving the additional payment amount allowed.
- If an original payment was an overpayment by Montana Healthcare Programs, the adjustment will result in recovery of the overpaid amount through a credit. If the result is a credit balance, it can be worked off or the provider can pay off the balance by check. (See Credit Balances earlier in this chapter.)
- Any questions regarding claims or adjustments must be directed to Provider Relations. (See Key Contacts.)
Completing an Individual Adjustment Request Form
Section A
Field: 1. Provider name and address
Description: Provider’s name and address (and mailing address if different).
Field: 2. Member name
Description: The member’s name is here.
Field: 3.* Internal control number (ICN)
Description: There can be only one ICN per adjustment request form. When adjusting a claim that has been previously adjusted, use the ICN of the most recent claim.
Field: 4.* Provider NPI
Description: The provider’s NPI.
Field: 5.* Member Montana Healthcare Programs number
Description: Member’s Montana Healthcare Programs ID number.
Field: 6. Date of payment
Description: Date claim was paid is found on remittance advice field 5 (see the sample RA earlier in this chapter).
Field: 7. Amount of payment
Description: The amount of payment from the remittance advice field 17 (see the sample RA earlier in this chapter.).
Section B
Field: 1. Units of service
Description: If a payment error was caused by an incorrect number of units, complete this line.
Field: 2. Procedure code/NDC/Revenue code
Description: If the procedure code, NDC, or revenue code is incorrect, complete this line.
Field: 3. Dates of service (DOS)
Description: If the date of service is incorrect, complete this line.
Field: 4. Billed amount
Description: If the billed amount is incorrect, complete this line.
Field: 5. Personal resource (nursing facility)
Description: If the member’s personal resource amount is incorrect, complete this line.
Field: 6. Insurance credit amount
Description: If the member’s insurance credit amount is incorrect, complete this line.
Field: 7. Net (Billed – TPL or Medicare paid)
Description: If the payment error was caused by a missing or incorrect insurance credit, complete this line. Net is billed amount minus the amount third party liability or Medicare paid.
Field: 8. Other/Remarks
Description: If none of the above items apply, or if you are unsure what caused the payment error, complete this line.
*Indicates a required field.
Mass Adjustments
Mass adjustments are done when it is necessary to reprocess multiple claims.
They generally occur when:
- Montana Healthcare Programs has a change of policy or fees that is retroactive. In this case federal laws require claims affected by the changes to be mass adjusted.
- A system error that affected claims processing is identified.
Providers are informed of mass adjustments on the first page of the RA in the RA Notice section. Mass adjustment claims shown on the RA have an ICN that begins with a 4. (See Key Fields on the Remittance Advice earlier in this chapter.)
Electronic RAs are available for only 90 days on the web portal.
Payment and the RA
Providers receive their Montana Healthcare Programs payment and remittance advice weekly. Payment can be via check or electronic funds transfer (EFT). Direct deposit is another name for EFT.
With EFT, the Department deposits the funds directly to the provider’s bank account. If the scheduled deposit day is a holiday, funds will be available on the next business day. This process does not affect the delivery of the remittance advice that providers currently receive with payments. RAs will continue to be mailed to providers unless they specifically request an electronic RA.
To participate in EFT, providers must complete a Direct Deposit Sign-Up Form (Standard Form 1199A). One form must be completed for each provider NPI. See the following table, Required Forms for EFT and/or Electronic RA.
Once electronic transfer testing shows payment to the provider’s account, all Montana Healthcare Programs payments will be made through EFT. See Direct Deposit Arrangements under Key Contacts for questions or changes regarding EFT.
Required Forms for EFT and/or Electronic RA
Form:
- EDI Provider Enrollment Form
- EDI Trading Partner Agreement
Purpose:
Allows providers to access their RAs on the Montana Access to Health (MATH) web portal.
Must also include:
- EDI Provider Enrollment Form
- EDI Trading Partner Agreement
Where to Get:
- Provider Information website
- Provider Relations (See Key Contacts.)
Where to Send:
Fax to number on form.
Form:
- Direct Deposit Sign-Up Form (Standard Form 1199A)
Purpose:
Allows the Department to automatically deposit Montana Healthcare Programs payment into provider’s bank account
Where to Get:
- Provider Information website (Forms)
- Provider’s bank Provider Relations (See Key Contacts.)
End of Remittance Advices and Adjustments Chapter
How Payment Is Calculated
Overview
Though providers do not need the information in this chapter in order to submit claims to the Department, the information allows providers to understand how payment is calculated and to predict approximate payment for particular claims. The payment methods described do not apply to services provided under Healthy Montana Kids (HMK)/Children’s Health Insurance Program (CHIP).
Payment for School-Based Services
Federal regulations specify that one government entity may not bill another government entity more than their cost (OMB A-87). The following describes payment methods for various services that can be provided in the school setting. Payment for these services is limited to the lower of the calculated fee or the billed amount.
Speech, Occupational and Physical Therapy Services
Speech and language therapy services, occupational therapy services and physical therapy services are paid by the Resource Based Relative Value Scale (RBRVS) method of reimbursement. As noted above, only the federal portion will be paid. For more detail on the RBRVS system, see the How Payment Is Calculated chapter of the Physician-Related Services provider manual, which is available on the Provider Information website. (See Key Websites.)
Each RBRVS fee is the product of a relative value times a conversion factor. This total is always multiplied by the current Federal Matching Assistance Percentage (FMAP).
The Department publishes relative weights, the current conversion factor, and the current FMAP figure. The conversion factor is determined by the Department and set at a level intended to achieve legislatively set budget targets.
Private Duty Nursing
The only code available for this service is T1000. Payment for this code is based on the Montana Healthcare Programs fee schedule, and is calculated as follows:
Fee x number of 15-minute units = payment
The current FMAP is then calculated against this total for final reimbursement
School Psychologist
Both codes available for billing school psychologist services are paid by the RBRVS method.
Each RBRVS fee is the product of a relative value times a conversion factor. This total is always multiplied by the current FMAP for a total reimbursement.
The Department publishes relative weights, the current conversion factor, and the current FMAP figure. The conversion factor is determined by the Department and set at a level intended to achieve legislatively set budget targets.
Personal Care Paraprofessionals
The only code available for this service is T1019. Payment for this code is based on the Montana Healthcare Programs fee schedule, and is calculated as follows:
Fee x number of 15-minute units = payment
The current FMAP is then calculated against this total for final reimbursement.
How Payment Is Calculated on TPL Claims
When a member has coverage from both Montana Healthcare Programs and another insurance company, the other insurance company is referred to as Third Party Liability (TPL). In these cases, the other insurance is the primary payer (as described in the Coordination of Benefits chapter of this manual), and Montana Healthcare Programs makes a payment as the secondary payer. Montana Healthcare Programs will make a payment only when the TPL payment is less than the Montana Healthcare Programs allowed amount.
How Payment Is Calculated on Medicare Crossover Claims
When a member has coverage from both Medicare and Montana Healthcare Programs, Medicare is the primary payer. Montana Healthcare Programs will pay the coinsurance and deductible amounts for these dually eligible individuals. See the How Payment is Calculated chapter in the Physician-Related Services manual for examples on how payment is calculated on Medicare crossover claims.
End of How Payment is Calculated Chapter
Appendix A: Forms
- Individual Adjustment Request
- Audit Preparation Checklist
- Request for Private Duty Nursing Services
- Paperwork Attachment Cover Sheet
End of Appendix A: Forms Chapter
Appendix B: Personal Care Paraprofessional Services Documentation
Personal Care Paraprofessional Services Provided in Schools – Child Profile
Purpose
The Child Profile is intended to:
- To provide an instrument for collecting and documenting essential information needed to establish the Montana Healthcare Programs child’s functional limitations and ability to perform activities of daily living.
- To document information on service planning issues for personal care services.
- To provide a worksheet for determining the daily units per week needed by the child.
Procedure
The Profile must be completed by the Individualized Education Plan (IEP) team at the initial meeting for services, at the annual review, and whenever a significant change in the child’s condition occurs causing the service need to change.
Instructions
- Child Name: Enter the child's full name.
- Child ID: Enter child's Montana Healthcare Programs ID number.
- DOB: Child’s date of birth.
- Date Span: The time period the child will receive personal care services, up to one year.
- Level of Impairment: Rate the child's impairment level according to the following scale for each task listed:
0 = Independent: No functional impairment. The child is able to conduct the activities without difficulty and has no need for assistance. Need is met with adaptive equipment or service animal.
1 = Standby/Cuing: Mild functional impairment. The child is able to conduct the activity but does require standby assist or cuing.
2 = Limited Assist: Moderate functional impairment. The child is able to conduct the activity with moderate difficulty and requires minimal assistance.
3 = Extensive Assist: Severe functional impairment. The child has considerable difficulty completing the activity and requires extensive assistance.
4 = Total Dependence: Total functional impairment. The child is completely unable to carry out any part of the activity.
An IEP team member must decide which of the five impairment levels best describes the child reviewed. An impairment in this context is a functional limitation (i.e., a limitation in the ability to carry out an activity or function). A member is considered to have an impairment with respect to a particular activity if he/she is limited, either physically or mentally, in his/her ability to carry out that activity.
The “0” and “4” rating is absolute in the sense that they indicate no functional impairment or total dependency. For example, if a child can perform any of the dressing tasks for themselves, a “4” is not appropriate. If he/she can perform the dressing task without difficulty, a “0” is appropriate.
If a child is able to conduct an activity only with difficulty, and the difficulty is such that the child frequently cannot complete some part of the activity, then the child is impaired, even if the child at other times can complete the entire activity. In addition, if the degree of difficulty is such that the child should have at least minimal assistance with that activity, then the child is impaired, even if the child can (with difficulty) conduct the activity without assistance. If the child can complete the activity but needs cuing to do so, or, because of safety considerations needs someone there while completing the task, they would require standby assistance. If the difficulty with an activity does not affect the child's conduct of the activity or does not cause any problems for the child, the child is not impaired.
Enter a Level for Each Task
The Personal Care Paraprofessional Services Profile is designed to rate a child's capacity for self-care. Determine the level for each task according to the capacity for self-care and not according to the child's access to a resource to assist with the task. In rating each item, use the child's response, your own observations of activity, and any knowledge provided about the child from other sources. To determine the severity of the child's impairment, consider the following factors:
- Child Perception of the Impairment: Does the child view the impairment as a major or minor problem?
- Congruence: Is the child's response to a particular question consistent with the child's response to other questions and, also, consistent with what you have observed?
- Child History: Probe for an understanding of the child's history as it relates to the current situation and of the child's attitude about the severity of the impairment. How has the impairment changed the child's lifestyle?
- Adaptation: If the child has adapted his physical environment or clothing to the extent that he is able to function without assistance, the degree of impairment will be lessened, but the child will still have an impairment. This includes the use of adaptive equipment.
Use the following examples for each item to help you differentiate between scores of 2 or 3.
ADL: Grooming
2 = Limited Assist: Child may set out supplies. Child may accomplish tasks an adaptive device for assistance.
3 = Extensive: Child needs to have help with shaving or shampooing, etc., because of inability to see well, to reach, or to successfully use equipment. Child needs someone to put lotion on body or to comb or brush hair.
ADL: Toileting
2 = Limited Assist: Child has instances of urinary incontinence, and needs help because of this from time to time. Fecal incontinence does not occur unless child has a specific illness episode. Child may have catheter or colostomy bag, and occasionally needs assistance with management.
3 = Extensive: Child often is unable to get to the bathroom on time to urinate. Child has occasional episodes of fecal incontinence. Child may wear diapers to manage the problem and needs some assistance with them. Child usually needs assistance with catheter or colostomy bag.
ADL: Dressing
2 = Limited Assist: Child needs occasional help with zippers, buttons, or putting on shoes and socks. Child may need help laying out and selecting clothes.
3 = Extensive: Child needs help with zippers, buttons, or shoes and socks. Child needs help getting into garments, including putting arms in sleeves, legs in pants, or pulling up pants. Child may dress totally inappropriately without help or would not finish dressing without physical assistance.
ADL: Transferring
2 = Limited Assist: Child usually can get out of bed or chair with minimal assistance.
3 = Extensive: Child needs hands-on assistance when rising to a standing position or moving into a wheelchair to prevent losing balance or falling. Child is able to help with the transfer by holding on, pivoting, and/or supporting himself.
ADL: Ambulation
2 = Limited Assist: Child walks alone without assistance for only short distances. Child can walk with minimal difficulty using an assistive device or by holding onto walls or furniture.
3 = Extensive: Child has considerable difficulty walking even with an assistive device. Child can walk only with assistance from another person. Child never walks alone outdoors without assistance. Child may use a wheelchair periodically.
ADL: Eating
2 = Limited Assist: Child may need occasional physical help. Child eats with adaptive devices but requires help with their positioning.
3 = Extensive: Child usually needs extensive hands-on assistance with eating. Child may hold eating utensils but needs continuous assistance during meals. Child would not complete meal without continual help. Spoon-feeding of most foods is required, but child can eat some finger foods.
ADL: Exercise
2 = Limited Assist: Child may need occasional assistance in completing exercise routine. Child may need occasional support or guidance.
3 = Extensive: Child needs some assistance in completing exercise routine. Child needs support or guidance.
ADL: Bus Escort
2 = Limited Assist: Child requires minimal assistance on bus en route to or from school. Child does not have family or caregiver to assist. Child receives a medical service at school on this date.
3 = Extensive: Child requires assistance on bus en route to or from school. Child does not have family or caregiver to assist. Child receives a medical service at school on this date.
Check the appropriate column that indicates the degree to which the child's need for help in the completion of each task is met. Check one column for each task:
M = Met: The child's needs are met. The child may be independent in this task or someone other than the Personal Care Paraprofessional is meeting the child’s need for help. Other sources for meeting the need include family or friends. No time can be authorized for any task coded with an “M”.
P = Partially Met: The child requires help with the task. Someone other than the personal care paraprofessional is providing that help part of the time, or the child may participate
in the task.
U = Unmet: The child requires help with the task and the need is currently unmet.
- Notes: Enter any appropriate notes.
- Minutes Per Day: For each task to be provided, enter the daily number of minutes needed to conduct that task.
- Days Per Week: For each task to be provided, enter the number of days per week the child will require assistance with the task.
- Total Minutes: Multiply the minutes per day times the days per week to obtain the total minutes per week for each task.
The amount of time allowed for any particular task should be determined by taking into account:
- The amount of assistance the child will usually need.
- Which specific activities need to be accomplished.
- Environmental/housing factors that may hinder (or facilitate) service delivery.
- Child’s unique circumstances.
Personal Care Paraprofessional Services Provided In Schools Child Profile - Form
Task/Hour Guide Instructions
Purpose
The purpose of this form is to record the amount of time that is spent providing Personal Care services. This form is a sample and can be recreated by district personnel to meet specific needs.
Specific Tasks
Each task has one or more activities or sub-tasks that forms the overall task. When calculating time, carefully consider which activities were provided.
- Dressing:
- Dressing member
- Undressing member
- Cuing assistance
- Exercise:
- Range of motion
- Grooming:
- Brushing teeth
- Laying out supplies
- Combing/brushing hair
- Applying nonprescription lotion to skin
- Washing hands and face
- Cuing assistance
- Toileting:
- Changing diapers
- Changing colostomy bag/emptying catheter bag
- Assisting on/off bed pan
- Assisting with use of urinal
- Assisting with feminine hygiene needs
- Assisting with clothing during toileting
- Assisting with toilet hygiene; includes use of toilet paper & washing hands
- Set-up supplies and equipment (Does NOT include preparing catheter equipment)
- Standby assistance
- Transfer:
- Non-ambulatory movement from one stationary position to another (transfer)
- Adjusting/changing member’s position in bed or chair (positioning)
- Ambulation (Walking):
- Assisting child in rising from a sitting to a standing position and/or position for use of walking apparatus
- Assisting with putting on and removing leg braces and prostheses for ambulation
- Assisting with ambulation/using steps
- Standby assistance with ambulation
- Assistance with wheelchair ambulation
NOTE: Do not include exercise as ambulation.
- Eating:
- Spoon feeding
- Bottle feeding
- Set up of utensils/adaptive devices
- Assistance with using eating or drinking utensils/adaptive devices
- Cutting up foods
- Standby assistance/encouragement
NOTE: Tube feeding is not an allowable service.
- Bus Escort:
- Accompanying a child on the bus when the child is functionally limited and receives medical service at the school on that date. Not for purposes of behavioral management.
End of Appendix B: Personal Care Paraprofessional Services Documentation Chapter
Definitions and Acronyms
This section contains definitions, abbreviations, and acronyms used in this manual.
270/271 Transactions
The ASC X12N eligibility inquiry (270) and response (271) transactions.
276/277 Transactions
The ASC X12N claim status request (276) and response (277) transactions.
278 Transactions
The ASC X12N request for services review and response used for prior authorization.
835 Transactions
The ASC X12N payment and remittance advice (explanation of benefits) transaction.
837 Transactions
The ASC X12N professional, institutional, and dental claim transactions (each with its own separate Implementation Guide).
Accredited Standards Committee X12, Insurance Subcommittee (ASC X12N)
The ANSI-accredited standards development organization, and one of the six Designated Standards Maintenance Organizations (DSMO), that created and is tasked with maintaining the administrative and financial transactions standards adopted under HIPAA for all health plans, clearinghouses, and providers who use electronic transactions.
Administrative Rules of Montana (ARM)
The rules published by the executive departments and agencies of the state government.
Allowed Amount
The maximum amount reimbursed to a provider for a health care service as determined by Montana Healthcare Programs/MHSP/HMK or another payer. Other cost factors, (such as TPL, or incurment) are often deducted from the allowed amount before final payment. Montana Healthcare Programs’ allowed amount for each covered service is listed on the Department fee schedule.
Ancillary Provider
Any provider that is subordinate to the member’s primary provider, or providing services in the facility or institution that has accepted the member as a Montana Healthcare Programs member.
Assignment of Benefits
A voluntary decision by the member to have insurance benefits paid directly to the provider rather than to the member. The act requires the signing of a form for the purpose. The provider is not obligated to accept an assignment of benefits. However, the provider may require assignment in order to protect the provider’s revenue.
Authorization
An official approval for action taken for, or on behalf of, a Montana Healthcare Programs member. This approval is only valid if the member is eligible on the date of service.
Basic Montana Healthcare Programs
members with Basic Montana Healthcare Programs have limited Montana Healthcare Programs services. See the Montana Healthcare Programs Covered Services chapter General Information for Providers manual.
Bundled
Items or services that are deemed integral to performing a procedure or visit are not paid separately in the APC system. They are packaged (also called bundled) into the payment for the procedure or visit. Medicare developed the relative weights for surgical, medical, and other types of visits so that the weights reflect the packaging rules used in the APC method. Items or services that are packaged receive a status code of “N”.
Cash Option
Cash option allows the member to pay a monthly premium to Montana Healthcare Programs and have Montana Healthcare Programs coverage for the entire month rather than a partial month.
Centers for Medicare and Medicaid Services (CMS)
Administers the Medicare program and oversees the state Montana Healthcare Programs.
Children’s Health Insurance Program (CHIP)
The Montana plan is now known as Healthy Montana Kids (HMK).
Children’s Special Health Services (CSHS)
CSHS assists children with special health care needs who are not eligible for Montana Healthcare Programs by paying medical costs, finding resources, and conducting clinics.
Clean Claim
A claim that can be processed without additional information from or action by the provider of the service.
Code of Federal Regulations (CFR)
Rules published by executive departments and agencies of the federal government.
Coinsurance
The member’s financial responsibility for a medical bill as assigned by Montana Healthcare Programs or Medicare (usually a percentage). Montana Healthcare Programs coinsurance is usually 5% of the Montana Healthcare Programs allowed amount, and Medicare coinsurance is usually 20% of the Medicare allowed amount.
Conversion Factor
A state specific dollar amount that converts relative values into an actual fee. This calculation allows each payer to adopt the RBRVS to its own economy.
Copayment
The member’s financial responsibility for a medical bill as assigned by Montana Healthcare Programs (usually a flat fee).
Cosmetic
Serving to modify or improve the appearance of a physical feature, defect, or irregularity.
CPT
Physicians’ Current Procedural Terminology contains procedure codes which are used by medical practitioners in billing for services rendered. The book is published by the American Medical Association.
Credit Balance Claims
Adjusted claims that reduce original payments, causing the provider to owe money to the Department. These claims are considered in process and continue to appear on the remittance advice until the credit has been satisfied.
Crossovers
Claims for members who have both Medicare and Montana Healthcare Programs. These claims may come electronically from Medicare or directly from the provider.
DPHHS, State Agency
The Montana Department of Public Health and Human Services (DPHHS or the Department) is the designated State Agency that administers the Montana Healthcare Program. The Department's legal authority is contained in Title 53, Chapter 6 MCA. At the federal level, the legal basis for the program is contained in Title XIX of the Social Security Act and Title 42 of the Code of Federal Regulations (CFR). The program is administered in accordance with the Administrative Rules of Montana (ARM), Title 37, Chapter 86.
Dual Eligibles
Members who are covered by Medicare and Montana Healthcare Programs.
Early and Periodic Screening, Diagnosis, and Treatment (EPSDT)
This program provides Montana Healthcare Programs-covered children with comprehensive health screenings, diagnostic services, and treatment of health problems.
Electronic Funds Transfer (EFT)
Payment of medical claims that are deposited directly to the provider’s bank account.
Emergency Services
A service is reimbursed as an emergency if one of the following criteria is met:
- The service is billed with CPT Code 99284 or 99285
- The member has a qualifying emergency diagnosis code. A list of emergency diagnosis codes is available on the Provider Information website.
- The services did not meet one of the previous two requirements, but the hospital believes an emergency existed. In this case, the claim and documentation supporting the emergent nature of the service must be mailed to the emergency department review contractor.
Experimental
A noncovered item or service that researchers are studying to investigate how it affects health.
Explanation of Medicare Benefits (EOMB)
A notice sent to providers informing them of the services which have been paid by Medicare.
Fiscal Agent
Conduent State Healthcare, LLC, is the fiscal agent for the State of Montana and processes claims at the Department's direction and in accordance with ARM 37.86 et seq.
Full Montana Healthcare Programs
members with Full Montana Healthcare Programs have a full scope of Montana Healthcare Programs benefits. See the General Information for Providers manual, Montana Healthcare Programs Covered Services.
Gross Adjustment
A lump sum debit or credit that is not claim specific made to a provider.
HCPCS
Acronym for the Healthcare Common Procedure Coding System, and is pronounced “hickpicks.” There are two types of HCPCS codes:
- Level 1 includes the CPT codes.
- Level 2 includes the alphanumeric codes A–V which CMS maintains for a wide range of services from ambulance trips to hearing aids which are not addressed by CPT coding.
Health Improvement Program (HIP)
A service provided under the Passport to Health program for members who have one or more chronic health conditions. Care management focuses on helping members improve their health outcomes through education, help with social services, and coordination with the member's medical providers.
Health Insurance Portability and Accountability Act (HIPAA)
A federal plan designed to improve efficiency of the health care system by establishing standards for transmission, storage, and handling of data.
Healthy Montana Kids (HMK)
HMK offers low-cost or free health insurance for low-income children younger than 19. Children must be uninsured U.S. citizens or qualified aliens, Montana residents who are not eligible for Montana Healthcare Programs. DPHHS administers the program and purchases health insurance from Blue Cross and Blue Shield of Montana (BCBSMT). Benefits for dental services and eyeglasses are provided by DPHHS through the same contractor (Conduent State Healthcare, LLC) that handles Montana Healthcare Programs provider relations and claims processing.
International Classification of Disease (ICD)
The International Classification of Diseases contains the diagnosis codes used in coding claims and the procedure codes used in billing for services performed in a hospital setting.
Indian Health Service (IHS)
IHS provides health services to American Indians and Alaska Natives.
Individual Adjustment
A request for a correction to a specific paid claim.
Internal Control Number (ICN)
The unique number assigned to each claim transaction that is used for tracking.
Investigational
A noncovered item or service that researchers are studying to investigate how it affects health.
Mass Adjustment
Adjustments made to multiple claims at the same time. They generally occur when the Department has a change of policy or fees that is retroactive, or when a system error that affected claims processing is identified.
Member
An individual enrolled in a Department medical assistance program.
Medically Necessary
A term describing a requested service which is reasonably calculated to prevent, diagnose, correct, cure, alleviate or prevent worsening of conditions in the member. These conditions must be classified as one of the following: endanger life, cause suffering or pain, result in an illness or infirmity, threaten to cause or aggravate a handicap, or cause physical deformity or malfunction. There must be no other equally effective, more conservative, or substantially less costly course of treatment available or suitable for the member requesting the service. For the purpose of this definition, course of treatment may include mere observation or, when appropriate, no treatment at all.
Medicare
The federal health insurance program for certain aged or disabled members.
Mental Health Services Plan (MHSP)
This plan is for individuals who have a severe and disabling mental illness (SDMI), are ineligible for Montana Healthcare Programs, and have a family income that does not exceed an amount established by the Department.
Mentally Incompetent
According to CFR 441.251, a mentally incompetent individual means an individual who has been declared mentally incompetent by a federal, state, or local court of competent jurisdiction for any purpose, unless the individual has been declared competent for purposes which include the ability to consent to sterilization.
Montana Access to Health (MATH) Web Portal
A secure website on which providers may view members’ medical history, verify member eligibility, submit claims to Montana Healthcare Programs, check the status of a claim, verify the status of a warrant, and download remittance advice reports.
Montana Breast and Cervical Cancer Treatment Program
This program provides Full Montana Healthcare Programs coverage for women who have been screened through the Montana Breast and Cervical Health Program (MBCHP) and diagnosed with breast and/or cervical cancer or a pre-cancerous condition.
Montana Healthcare Programs/HMK Plus
A program that provides health care coverage to specific populations, especially low-income families with children, pregnant women, disabled individuals, and the elderly. Montana Healthcare Programs is administered by state governments under broad federal guidelines.
Passport Referral Number
This is a 7-digit number assigned to Passport providers. When a Passport provider refers a member to another provider for services, this number is given to the other provider and is required when processing the claim.
Passport to Health
A Montana Healthcare Programs medical home program where the member selects a primary care provider who manages the member’s health care needs.
Pay-and-Chase
Montana Healthcare Programs pays a claim and then recovers payment from the third-party carrier that is financially responsible for all or part of the claim.
Pending Claim
These claims have been entered into the system but have not reached final disposition. They require either additional review or are waiting for member eligibility information.
Potential Third-Party Liability
Any entity that may be liable to pay all or part of the medical cost of care for a Montana Healthcare Programs, MHSP or HMK member.
Prior Authorization (PA)
The approval process required before certain services or supplies are paid by Montana Healthcare Programs. Prior authorization must be obtained before providing the service or supply.
Private-Pay
When a member chooses to pay for medical services out of his or her own pocket.
Protocols
Written plans developed by a public health clinic in collaboration with physician and nursing staff. Protocols specify nursing procedures to be followed in giving a specific exam, or providing care for particular conditions. Protocols must by updated and approved by a physician at least annually.
Provider or Provider of Service
An institution, agency, or person:
- • Having a signed agreement with the Department to furnish medical care and goods and/or services to members; and
- Eligible to receive payment from the Department.
Qualified Medicare Beneficiary (QMB)
QMB members are members for whom Montana Healthcare Programs pays their Medicare premiums and some or all of their Medicare coinsurance and deductibles.
Reason and Remark Code
A code which prints on the Montana Healthcare Programs remittance advice (RA) that explains why a claim was denied or suspended. The explanation of the Reason/Remark codes is found at the end of the RA (formerly called EOB code).
Referral
When providers refer members to other Montana Healthcare Programs providers for medically necessary services that they cannot provide.
Remittance Advice (RA)
The results of claims processing (including paid, denied, and pending claims) are listed on the RA.
Relative Value Scale (RVS)
A numerical scale designed to permit comparisons of appropriate prices for various services. The RVS is made up of the relative value units (RVUs) for all the objects in the class for which it is developed.
Relative Value Unit (RVU)
The numerical value given to each service in a relative value scale.
Resource-Based Relative Value Scale (RBRVS)
A method of determining physicians’ fees based on the time, training, skill, and other factors required to deliver various services.
Retroactive Eligibility
When a member is determined to be eligible for Montana Healthcare Programs effective prior to the current date.
Sanction
The penalty for noncompliance with laws, rules, and policies regarding Montana Healthcare Programs. A sanction may include withholding payment from a provider or terminating Montana Healthcare Programs enrollment.
School-Based Services
Medically necessary health-related services provided to Montana Healthcare Programs eligible children up to and including age 20. These services are provided in a school setting by licensed medical professionals.
Specified Low-Income Medicare Beneficiaries (SLMB)
For these members, Montana Healthcare Programs pays the Medicare premium only. They are not eligible for other Montana Healthcare Programs benefits and must pay their own Medicare coinsurance and deductibles.
Spending Down
Members with high medical expenses relative to their income can become eligible for Montana Healthcare Programs by “spending down” their income to specified levels. The member is responsible to pay for services received before eligibility begins, and Montana Healthcare Programs pays for remaining covered services.
Team Care
A restricted services program that is part of Passport to Health. Restricted services programs are designed to assist members in making better health care decisions so that they can avoid overutilizing health services. Team Care members are joined by a team assembled to assist them in accessing health care. The team consists of the member, the PCP, a pharmacy, the Department, and the Department’s quality improvement organization. The team may also include a community-based care manager from the Department's Health Improvement Program.
Third Party Liability (TPL)
Any entity that is, or may be, liable to pay all or part of the medical cost of care for a Montana Healthcare Programs, MHSP or HMK member.
Timely Filing
Providers must submit clean claims (claims that can be processed without additional information or documentation from or action by the provider) to Montana Healthcare Programs within:
- Twelve months from whichever is later:
- the date of service;
- the date retroactive eligibility or disability is determined;
- Six months from the date on the Medicare explanation of benefits approving the service; or
- Six months from the date on an adjustment notice from a third-party payer who has previously processed the claim for the same service, and the adjustment notice is dated after the periods described above.
Usual and Customary
The fee that the provider most frequently charges the general public for a service or item.
WINASAP 5010
WINASAP 5010 is a Windows-based electronic claims entry application for Montana Healthcare Programs. This software was developed as an alternative to submitting claims on paper. For more information, contact the EDI Technical Help Desk. (See Key Contacts.)
End of Definitions and Acronyms Chapter
Search Options
Previous editions of this manual contained an index.
This edition has three search options.
1. Search the whole manual. Open the Complete Manual pane. From your keyboard press the Ctrl and F keys at the same time. A search box will appear. Type in a descriptive or key word (for example "Denials". The search box will show all locations where denials discussed in the manual.
2. Search by Chapter. Open any Chapter tab (for example the "Billing Procedures" tab). From your keyboard press the Ctrl and F keys at the same time. A search box will appear. Type in a descriptive or key word (for example "Denials". The search box will show where denials discussed in just that chapter.
3. Site Search. Search the manual as well as other documents related to a particular search term on the Montana Healthcare Programs Site Specific Search page.
End of Search Options Chapter
End of School-Based Services Manual
Update Log
Publication History
This publication supersedes all previous School-Based Services handbooks. Published by the Montana Department of Public Health & Human Services, August 2003.
Updated October 2003, December 2003, January 2004, April 2004, August 2004, April 2005, May 2005, August 2005, January 2006, April 2006, February 2007, April 2008, June 2011, April 2012, March 2013, May 2013, October 2017, November 2017, December 2017, January 2020, March 2020, March 2022, and April 2022.
CPT codes, descriptions and other data only are copyright 1999 American Medical Association (or such other date of publication of CPT). All Rights Reserved. Applicable FARS/DFARS Apply.
Update Log
04/14/2022
- Removed Nurse First Advice Line references.
- Updated Index to Search Options.
03/25/2022
- Removed CSCT references where no longer applicable.
03/26/2020
- Added language that services may be performed by a therapy assistant or therapy aide within their scope of practice but must be billed to Montana Healthcare Programs under the school’s supervising licensed therapist’s NPI.
- Clarified that Telehealth services are available for Physical Therapy, Occupational Therapy and Speech Therapy.
- Removed levels of supervision for speech, occupational, and physical therapy aides and assistants as these requirements fall under the purview of the Board of Speech-Language Pathologists and Audiologists, Montana Board of Occupational Therapy Practice and Montana Board of Physical Therapy Examiners respectively.
- Under Billing for Specific Services, Therapy Services, removed the discussion regarding supervision for aides/assistants for the reason noted above.
01/01/2020
- Cost Share references removed from the Billing Procedures, Submitting A Claim, Remittance and Advices, How Payment is Calculated, Definitions and Acronyms Chapters.
- Term "Medicaid" replaced with "Montana Healthcare Programs" throughout the manual.
- Terms "client" and "patient" replaced with "member".
- Health Improvement Program (HIP) references removed.
12/11/2017
Code changes were made in the Billing Procedures Chapter
11/02/2017
Code changes were made in the Billing Procedures Chapter.
10/20/2017
School-Based Services Manual converted to an HTML format and adapted to 508 Accessibility Standards.
07/10/2013
School-Based Services, May 2013: Entire Manual
These replacement pages includes a terminology change (client to member); however, unless a paragraph also included content changes, it is not marked as a change.
04/27/2012
School-Based Services, April 2012: Covered Services
06/09/2011
School-Based Services, June 2011: Covered Services
09/16/2008
School-Based Services, April 2008: Key Contacts, Covered Services, Billing Procedures, and Claim Instructions
02/14/2007
School-Based Services, February 2007: Revised Physician Order Information, New Private Duty Nursing Request Form
04/25/2006
School-Based Services, April 2006: Coordination of Benefits Information
01/17/2006
School-Based Services, January 2006: Documentation Requirements, Restricted CSCT Services, Private-Duty Nursing Review Requirements, and School-Based Services Codes
10/06/2005
School-Based Services, August 2005: Covered Services and Billing Information for CSCT and Therapy
05/12/2005
School-Based Services, May 2005: Key Contacts and Place of Service
04/11/2005
School-Based Services, April 2005: Key Contacts
08/30/2004
School-Based Services, August 2004: Audiology Services Defined
04/26/2004
School-Based Services, April 2004: Key Contacts and Websites, Covered Services, COB, Billing Procedures, Claim Forms, RAs and Adjustments, Forms and Definitions
01/14/2004
School-Based Services, January 2004: Covered Services Error Correction
12/23/2003
School-Based Services, December 2003:CSCT Changes
End of Update Log Chapter
Table of Contents
Key Contacts
Key Websites
Introduction
Covered Services
General Coverage Principles
Services for Children (ARM 37.86.2201–2221)
Services within Scope of Practice (ARM 37.85.401)
Provider Requirements
IEP Requirements
Member Qualifications
School Qualifications
Physician Order/Referral
Documentation Requirements
Noncovered Services (ARM 37.85.207 and 37.86.3002)
Importance of Fee Schedules
Coverage of Specific Services
Assessment to Initiate an IEP
Therapy Services
Private Duty Nursing Services
School Psychologists and Mental Health Services
Personal Care Paraprofessional Services
Special Needs Transportation
Audiology
Orientation and Mobility Specialist Services
Authorization Requirements Summary
Other Programs
Passport to Health Program
What Is Passport to Health? (ARM 37.86.5101–5120, 37.86.5303, and 37.86.5201–5206)
Passport to Health Primary Care Case Management (ARM 37.86.5101–5120)
Team Care (ARM 37.86.5303)
Other Programs
Prior Authorization
What Is Prior Authorization (ARM 37.86.5101–5120)
Getting Questions Answered
Other Programs
Coordination of Benefits
When Members Have Other Coverage
Identifying Other Sources of Coverage
When a Member Has Medicare
Medicare Part B Crossover Claims
When Medicare Pays or Denies a Service
When Montana Healthcare Programs Does Not Respond to Crossover Claims
Submitting Medicare Claims to Montana Healthcare Programs
When a Member Has TPL (ARM 37.85.407)
Billing for Montana Healthcare Programs Covered Services When No IEP Exists
Billing for Montana Healthcare Programs Covered Services under an IEP
Exceptions to Billing Third Party First
Requesting an Exemption
When the Third Party Pays or Denies a Service
When the Third Party Does Not Respond
Billing Procedures
Claim Forms
Timely Filing Limits (ARM 37.85.406)
Tips to Avoid Timely Filing Denials
When Providers Cannot Bill Montana Healthcare Programs Members (ARM 37.85.406)
Member Co-Payment (ARM 37.85.204 and 37.85.402)
Billing for Members with Other Insurance
Billing for Retroactively Eligible Members
Service Fees
Coding Tips
Using Modifiers
Multiple Services on the Same Date
Time and Units
Place of Service
Billing for Specific Services
Assessment to Initiate an IEP
Therapy Services
Private Duty Nursing Services
School Psychologists and Mental Health Services
Personal Care Paraprofessional Services
Special Needs Transportation
Audiology
Submitting Electronic Claims
Billing Electronically with Paper Attachments
Submitting Paper Claims
Claim Inquiries
The Most Common Billing Errors and How to Avoid Them
Other Programs
Submitting a Claim
CMS-1500 Agreement
Avoiding Claim Errors
Other Programs
Remittance Advices and Adjustments
The Remittance Advice
Sample Remittance Notice
Credit Balances
Rebilling and Adjustments
How Long Do I Have to Rebill or Adjust a Claim?
Rebilling Montana Healthcare Programs
Adjustments
Mass Adjustments
Payment and the RA
How Payment Is Calculated
Overview
Payment for School-Based Services
Speech, Occupational and Physical Therapy Services
Private Duty Nursing
School Psychologist
Personal Care Paraprofessionals
How Payment Is Calculated on TPL Claims
How Payment Is Calculated on Medicare Crossover Claims
Appendix A: Forms
Individual Adjustment
Audit Preparation Checklist
Private Duty Nursing Services Request
Paperwork Attachment Cover Sheet
Appendix B: Personal Care Paraprofessional Services Documentation
Personal Care Paraprofessional Services Provided in Schools – Child Profile
Purpose
Procedure
Instructions
Task/Hour Guide Instructions
Purpose
Specific Tasks
Task/Hour Guide
Definitions and Acronyms
Index
End of Table of Contents Chapter
Key Contacts
Hours for Key Contacts are 8:00 a.m. to 5:00 p.m. Monday through Friday (Mountain Time), unless otherwise stated. The phone numbers designated “In state” will not work outside Montana.
Chemical Dependency
For coverage information and other details regarding chemical dependency treatment, write or call:
(406) 444-3964 Phone
Send written inquiries to:
Chemical Dependency Bureau
Addictive and Mental Disorders Division
DPHHS
P.O. Box 202905
Helena, MT 59620-2905
Claims
Send paper claims and adjustment requests to:
Claims Processing Unit
P.O. Box 8000
Helena, MT 59604
Direct Deposit Arrangements
Providers who would like to receive their electronic remittance advices and electronic funds transfer should fax their information to Provider Relations:
(406) 442-4402 Fax
EDI Technical Help Desk
(800) 987-6719 In/Out of state
(406) 442-1837 Helena
(406) 442-4402 Fax
Montana EDI
P.O. Box 4936
Helena, MT 59604
Healthy Montana Kids (HMK)
(877) 543-7669 Phone (toll-free)
(877) 418-4533 Fax (toll-free)
(406) 444-6971 Phone (Helena)
(406) 444-4533 Fax (Helena)
Send email inquires to: hmk@mt.gov
HMK Program Officer
P.O. Box 202951
Helena, MT 59620-2951
Member Eligibility
There are several methods for verifying member eligibility. For details on each, see Verifying Member Eligibility in the Member Eligibility and Responsibilities chapter of the General Information for Providers manual.
FaxBack
(800) 714-0075 (24 hours)
Voice Response System
(800) 362-8312 (24 hours)
https://mtaccesstohealth.portal.conduent.com/mt/general/home.do
Medifax EDI
(800) 444-4336, X 2072 (24 hours)
Member Help Line
Members who have general Montana Healthcare Programs or Passport
questions may call the Help Line:
(800) 362-8312 Phone
Send written inquiries to:
Passport to Health
P.O. Box 254
Helena, MT 59624-0254
Prior Authorization
The following are some of the Department’s prior authorization contractors. Providers are expected to refer to their specific provider manual for prior authorization instructions.
Mountain-Pacific Quality Health
For prior authorization for school-based private duty nursing services and for prior authorization continued stay reviews for selected behavioral health services:
(406) 443-4020 X150 Helena
(800) 262-1545 X150 Outside Helena
(406) 443-4585 Fax
Send written inquiries to:
Medicaid Utilization Review
Mountain-Pacific Quality Health
Helena, MT 59602
For questions regarding prior authorization for medical necessity therapy reviews:
(406) 457-3060 Local
(877) 443-4021 Toll-free
(877) 443-2580 Fax local/long distance
Send written inquiries to:
Mountain Pacific Quality Health
3404 Cooney Drive
Helena, MT 59602
Provider Policy Questions
For policy questions, contact the appropriate division of the Department of Public Health and Human Services; see the Introduction chapter in the General Information for Providers manual. For inquiries related to licensure/endorsement, contact the Quality Assurance Division, Licensing Bureau:
(406) 444-2676 Phone
(406) 444-1742 Fax
Send written inquiries to:
Quality Assurance Division
Licensing Bureau
2401 Colonial Drive, Third Floor
Helena, MT 59602-2693
Provider Relations
For general claims questions, questions about eligibility, Passport to Health, payments, and denials:
(800) 624-3958 In/Out of state
(406) 442-1837 Helena
(406) 442-4402 Fax
Send e-mail inquiries to MTPRHelpdesk@conduent.com
Send written inquiries to:
Provider Relations Unit
P.O. Box 4936
Helena, MT 59604
Secretary of State
The Secretary of State’s office publishes the most current version of the Administrative Rules of Montana (ARM):
(406) 444-2055 Phone
Secretary of State
P.O. Box 202801
Helena, MT 59620-2801
Surveillance/Utilization Review
To report suspected provider fraud/abuse:
(406) 444-4586
(800) 376-1115
To report suspected member fraud/abuse:
(800) 201-6308
Send written inquiries to:
Fraud and Abuse
SURS
2401 Colonial Drive
P.O. Box 202953
Helena, MT 59620-2953
Team Care Program
For questions regarding Team Care:
(406) 444-9673 Phone
(406) 444-1861 Fax
Team Care Program Officer
Managed Care Bureau
DPHHS
P.O. Box 202951
Helena, MT 59620-2951
Third Party Liability
For questions about private insurance, Medicare, or other third-party liability:
(800) 624-3958 In/Out of state
(406) 442-1837 In/Out of state
Send written inquiries to:
Third Party Liability Unit
P.O. Box 5838
Helena, MT 59604
End of Key Contacts Chapter
Key Websites
EDI Gateway - https://edisolutionsmmis.portal.conduent.com/gcro/
Information Available:
EDI Gateway is Montana’s HIPAA clearinghouse. Visit this website for more information on:
- EDI enrollment
- EDI support
- FAQs
- Manuals
- Provider services
- Related links
- Software
Information Available:
- Information on Healthy Montana Kids (HMK)
https://mtaccesstohealth.portal.conduent.com/mt/general/home.do
Provider Information Website - medicaidprovider.mt.gov
Information Available:
- FAQs
- Fee schedules
- HIPAA update
- Key contacts
- Links to other websites
- Montana Healthcare Programs forms
- Montana Healthcare Programs news
- Newsletters
- Notices and manual replacement pages
- Passport to Health information
- Provider enrollment
- Provider manuals
- Remittance advice notices
- Training resources
- Upcoming events
Washington Publishing Company - www.wpc-edi.com
A fee is charged for documents; however, code lists are viewable online at no charge.
Information Available:
- HIPAA guides
- HIPAA tools
End of Key Websites Chapter
Introduction
Thank you for your willingness to serve members of the Montana Healthcare Programs and other medical assistance programs administered by the Department of Public Health and Human Services.
Manual Organization
This manual provides information specifically for the School-Based Services Program.
Most chapters have a section titled Other Programs that includes information about other Department programs such as the Mental Health Services Plan (MHSP) and Healthy Montana Kids (HMK). Other essential information for providers is contained in the separate General Information for Providers manual. Each provider is asked to review both the general manual and the specific manual for his/her provider type.
A table of contents and an index allow you to quickly find answers to most questions. The margins contain important notes with extra space for writing notes. There is a list of Key Contacts at the beginning of each manual. We have also included a space on the inside front cover to record your NPI for quick reference when calling Provider Relations.
Manual Maintenance
Manuals must be kept current. Changes to manuals are provided through provider notices and replacement pages. When replacing a page in a paper manual, file the old pages and notices in the back of the manual for use with claims that originated under the old policy. Provider notices and replacement pages are available on the Provider Information website. See Key Websites.
Providers are responsible for knowing and following current laws and regulations.
Rule References
Providers must be familiar with all current rules and regulations governing the Montana Healthcare Programs. Provider manuals are to assist providers in billing Montana Healthcare Programs; they do not contain all Montana Healthcare Programs rules and regulations. Rule citations in the text are a reference tool; they are not a summary of the entire rule. In the event that a manual conflicts with a rule, the rule prevails. Links to rule references are available on the Provider Information website. Paper copies of rules are available through the Secretary of State’s office. (See Key Contacts.)
The following rules and regulations are specific to the school-based services program. Additional Montana Healthcare Programs rule references are available in the General Information for Providers manual.
- Administrative Rules of Montana (ARM)
- ARM 37.86.2201 EPSDT Purpose, Eligibility and Scope
- ARM 37.86.2206–2207 EPSDT Medical and Other Services; Reimbursement
- ARM 37.86.2217 EPSDT Private Duty Nursing
- ARM 37.86.2230–2235 EPSDT, School-Based Health Related Services
Getting Questions Answered
The provider manuals are designed to answer most questions; however, questions may arise that require a call to a specific group (such as a program officer, Provider Relations, or a prior authorization unit). The list of Key Contacts at the front of this manual has important phone numbers and addresses pertaining to this manual. The Introduction chapter in the General Information for Providers manual also has a list of contacts for specific program policy information. Montana Healthcare Programs manuals, provider notices, replacement pages, fee schedules, forms, and much more are available on the Provider Information website. (See Key Websites.)
Claims Review (MCA 53-6-111, ARM 37.85.406)
The Department is committed to paying Montana Healthcare Programs providers’ claims as quickly as possible. Montana Healthcare Programs claims are electronically processed and usually are not reviewed by medical experts prior to payment to determine if the services provided were appropriately billed. Although the computerized system can detect and deny some erroneous claims, there are many erroneous claims it cannot detect. For this reason, payment of a claim does not mean the service was correctly billed or the payment made to the provider was correct. Periodic retrospective reviews are performed that may lead to the discovery of incorrect billing or incorrect payment. If a claim is paid and the Department later discovers the service was incorrectly billed or paid or the claim was erroneous in some other way, the Department is required by federal regulation to recover any overpayment, regardless of whether the incorrect payment was the result of Department or provider error or other cause (42 CFR 456.3).
Program Overview
Title XIX of the Social Security Act provides for a program of medical assistance to certain individuals and families with low income. This program, known as Montana Healthcare Programs, became law in 1965 as a jointly funded cooperative venture between the federal and state governments. Federal oversight for the Montana Healthcare Programs lies with the Centers for Medicare and Montana Healthcare Programs Services (CMS) in the Department of Public Health and Human Services (DPHHS).
The Early and Periodic Screening, Diagnosis, and Treatment (EPSDT) program is a special program for Montana Healthcare Programs beneficiaries under 21 years of age. The purpose of EPSDT is to ensure that through periodic checkups and early detection, children’s health problems are prevented and/or ameliorated. The EPSDT program allows states to provide services even if these services are not covered under the Montana Healthcare Programs state plan for other beneficiaries.
The Medicare Catastrophic Coverage Act, enacted in 1988, contained provisions which permit state Montana Healthcare Programs to provide reimbursement for health-related services provided as part of a child’s Individualized Education Plan (IEP). This reversed a previous policy that Montana Healthcare Programs could not reimburse for services provided by schools. As a result of this act, the State of Montana allows schools and cooperatives to bill for Montana Healthcare Programs services provided to Montana Healthcare Programs members pursuant to an IEP.
Montana Healthcare Programs reimburses health-related services provided by schools that are written into an IEP, if the services are covered under the Montana Healthcare Programs state plan or are covered under EPSDT. Services billed to Montana Healthcare Programs must be provided by qualified practitioners with credentials meeting state and federal Montana Healthcare Programs requirements. Montana Healthcare Programs provides reimbursement for health-related services and does not reimburse for services that are educational or instructional in nature.
Montana Healthcare Programs can be an important source of funding for schools, particularly because the cost of providing special education can greatly exceed the federal assistance provided under the Individuals with Disabilities Education Act (IDEA). Children who qualify for IDEA are frequently eligible for Montana Healthcare Programs services. Although Montana Healthcare Programs is traditionally the “payer of last resort” for health care services, it is required to reimburse for IDEA related medically necessary services for eligible children before IDEA funds are used.
In Montana, the Department of Public Health & Human Services, Montana Healthcare Programs Services Bureau, administers the Montana Healthcare Programs School-Based Services Program. This guide contains specific technical information about program requirements associated with seeking payment for covered services rendered in a school setting. The purpose of this guide is to inform schools on the appropriate methods for claiming reimbursement for the costs of health-related services provided.
End of Introduction Chapter
Covered Services
General Coverage Principles
Montana Healthcare Programs covers health-related services provided to children in a school setting when all of the following are met:
- The child qualifies for Individuals with Disabilities Education Act (IDEA).
- The services are written into an Individual Education Plan (IEP).
- The services are not free. Providers may not bill Montana Healthcare Programs for any services that are generally offered to all members without charge.
Refer to the IEP requirements in this chapter and the Coordination of Benefits chapter regarding billing services included/not included in a child’s IEP.
This chapter provides covered services information that applies specifically to school-based services. School-based services providers must meet the Montana Healthcare Programs
provider qualifications established by the state and have a provider agreement with the state. These providers must also meet the requirements specified in this manual and the General Information for Providers manual. School-based services provided to Montana Healthcare Programs members include the following:
- Therapy services (physical therapy, occupational therapy, speech language pathology)
- Audiology
- Private duty nursing
- School psychology and mental health services (including clinical social work and clinical professional counseling)
- Personal care (provided by paraprofessionals)
- Other diagnostic, preventative and rehabilitative services
- Specialized transportation
- Orientation and Mobility Specialist services (for blind and low vision)
Services for Children (ARM 37.86.2201–2221)
The Early and Periodic Screening, Diagnosis, and Treatment (EPSDT) Program is a comprehensive approach to health care for Montana Healthcare Programs members ages 20 and under. It is designed to prevent, identify, and then treat health problems before they become disabling. Under EPSDT, Montana Healthcare Programs eligible children may receive any medically necessary covered service, including all school-based services described in this manual. All applicable prior authorization requirements apply. (See the Prior Authorization chapter in this manual.)
Services within Scope of Practice (ARM 37.85.401)
Services provided under the School-Based Services Program are covered only when they are within the scope of the provider’s license.
Provider Requirements
Most school-based services must be provided by licensed health care providers. The exception is that activities of daily living services may be provided by personal care paraprofessionals. Montana Healthcare Programs does not cover services provided by a teacher or teacher’s aide; however, teachers or teacher aides may be used to assist in the development of child care planning. School-based services must be provided by only those providers listed in the table below.
Provider Requirements
Provider Type:
Private duty nursing services provided by:
- Licensed registered nurse
- Licensed practical nurse
Provider Requirements:
Nurses must have a valid certificate of registration issued by the Board of Nurse Examiners of the State of Montana or the Montana Board of Nursing Education and Nurse Registration.
Provider Type:
Mental health services provided by:
- Credentialed school psychologist
- Licensed psychologist
- Licensed clinical professional counselor
- Licensed clinical social worker
Provider Requirements:
Mental health providers must be licensed according to Montana’s state requirements. School psychologist services are provided by a professional with a Class 6 specialist license with a school psychologist endorsement.
Provider Type:
Therapy services provided by:
- Licensed occupational therapist
- Licensed physical therapist
- Licensed speech language pathologists
Provider Requirements:
These therapists are required to meet appropriate credentialing requirements as defined by the Montana Licensing Board.
Provider Type:
Audiology
Provider Requirements:
Must meet credentialing requirements as defined by the Montana Licensing Board.
Provider Type:
Personal care paraprofessional
Provider Requirements:
No licensing requirements.
Provider Type:
Orientation and Mobility Specialist
Provider Requirements:
Must have certification of the Academy for Certification of Vision Rehabilitation & Education Professionals (ACVREP) or a National Blindness Professional Certification (NOMC) from the National Blindness Professional Certification Board (NBPCB).
It is the responsibility of the school district to assure appropriately licensed providers perform all Montana Healthcare Programs covered services. Each school district must maintain documentation of each rendering practitioner’s license, certification, registration, or credential to practice in Montana. Montana Healthcare Programs providers who have had their license suspended by a state or federal government entity may not provide school-based services.
Services provided to Montana Healthcare Programs members must be documented in the member’s IEP.
IEP Requirements
Services provided to Montana Healthcare Programs members must be covered by Montana Healthcare Programs and documented in the member’s Individualized Education Plan (IEP), unless otherwise specified. School-based providers may bill Montana Healthcare Programs for Montana Healthcare Programs-covered health-related services provided to children with those services written into the IEP, even though the services may be provided to non-Montana Healthcare Programs children for free. However, if a child is covered by both Montana Healthcare Programs and private insurance, the private insurance must be billed prior to Montana Healthcare Programs. Exception to billing other insurance: Blue Cross and Blue Shield of Montana and HMK. Montana Healthcare Programs does not cover health-related services that are not included in an IEP unless all of the following requirements are met:
- Youth is enrolled in Montana Healthcare Programs.
- Services are medically necessary.
- A fee schedule is established for health-related services (can be a sliding scale to adjust for individuals with low incomes).
- The provider determines if each individual who receives services has insurance coverage or will be billed on a private-pay basis.
- The provider bills all individuals and/or the insurance carrier for the medical service provided.
Member Qualifications
To qualify for Montana Healthcare Programs school-based services, the member must be a Montana Healthcare Programs member and meet all the following criteria:
- Be Montana Healthcare Programs-eligible on the date of service.
- Be between the ages 3 and 20.
- Be entitled to school district services under the Individuals with Disabilities Education Act (IDEA).
- Have Montana Healthcare Programs reimbursable services referenced in his or her Individual Educational Plan (IEP). This shows that Montana Healthcare Programs covered services are recommended by the school district.
Cooperatives, joint boards, and non-public schools that do not receive state general funds for special education can not participate in the Montana Healthcare Programs as a school-based provider.
School Qualifications
Only public school districts, full-service education cooperatives and joint boards of trustees may enroll in the Montana Healthcare Programs School-Based Services Program. To qualify, the district, cooperative or joint board must receive special education funding from the state’s Office of Public Instruction general fund for public education. School districts include elementary, high school and K–12 districts that provide public educational services. Full-service education cooperatives and joint boards include those cooperatives eligible to receive direct state aid payments from the Superintendent of Public Instruction for special education services.
Schools That Employ Medical Service Providers:
- Schools that employ all or most of their medical service providers for whom the school submits bills can be enrolled with a single NPI for all services.
- Schools may use this single NPI to bill for any Montana Healthcare Programs covered service provided by a licensed provider.
- Schools that wish to have separate NPIs for each provider type (e.g., speech therapists, occupational therapists, and physical therapists) can request separate NPIs from the National Plan and Provider Enumeration System (NPPES).
Schools That Contract with External Medical Service Providers:
- Schools that contract with all or most of their providers must have the provider of service bill for each service they provide with their own individual NPI.
- Providers and schools can arrange with the Department for payments to be made to the school. If payments are assigned to the school, the school will also have the responsibility to collect third party liability payments on behalf of the service providers.
For more information on enrollment, visit the Provider Information website or contact Provider Enrollment. (See Key Contacts.)
Physician Order/Referral
Montana Healthcare Programs does not require physician orders or referrals for health-related services that are documented in the member’s IEP. The exception is private duty nursing services and personal care assistant services, which require a written order for private-duty nursing or physician signature for personal care assistance services. Other health-related services can be authorized by a licensed school practitioner meeting the State of Montana provider requirements to secure health-related services under an IEP.
Documentation Requirements
School-based service providers must maintain appropriate records. All case records must be current and available upon request. Records can be stored in any readily accessible format and location, and must be kept for six years and three months from the date of service. For more information on record keeping requirements, see the Surveillance/Utilization Review chapter in the General Information for Providers manual.
Medical documentation must include the following:
- Keep legible records.
- Date of service and the child’s name.
- The services provided during the course of each treatment and how the child responded.
- If the service is based on time units, (i.e., 15 minutes per unit), the provider of service should indicate begin and end times or the amount of time spent for each service. A service must take at least 8 minutes to bill one unit of service if the procedure has “per 15 minutes” in its description.
- Providers must sign and date each record documented on the day the medical service was rendered. Provider initials on daily records are acceptable providing their signature is included in other medical documentation within the child’s record.
- Documentation must, at least quarterly, include notes on member progress toward their goals. This is for the support of medical necessity and reviewing of the progress to maintain the rehabilitative nature of the service.
- The service provider must keep sufficient documentation to support the procedures billed to Montana Healthcare Programs. If a service is not documented, it did not happen.
- Documentation must not be created retroactively. Providers are responsible for maintaining records at the time of service.
The Montana Healthcare Programs School-Based Services Program is subject to both state and federal audits. As the Montana Healthcare Programs provider, the school certifies that the services being claimed for Montana Healthcare Programs reimbursement are medically necessary and furnished under the provider’s direction. Both fiscal and clinical compliance are monitored. In the event of adverse findings, the district/cooperative (not the mental health provider) will be held responsible for any paybacks to Montana Healthcare Programs. To assist in document retention for audit purposes, see the Audit Preparation Checklist on the Montana Healthcare Programs Provider Information website.
Noncovered Services (ARM 37.85.207)
The following is a list of services not covered by Montana Healthcare Programs.
- A provider’s time while attending member care meetings, Individual Educational Plan (IEP) meetings, individual treatment plan meetings, or member-related meetings with other medical professionals or family members.
- Services considered experimental or investigational.
- Services that are educational or instructional in nature.
- Services that are not medically necessary. The Department may review for medical necessity at any time before or after payment.
Use the current fee schedule for your provider type to verify coverage for specific services.
Importance of Fee Schedules
The easiest way to verify coverage for a specific service is to check the Department’s school-based services fee schedule. In addition to being listed on the fee schedule, all services provided must also meet the coverage criteria listed in the Provider Requirements chapter of the General Information for Providers manual and in this chapter. Use the fee schedule in conjunction with the more detailed coding descriptions listed in the CPT and HCPCS coding books. Take care to use the fee schedule and coding books that pertain to the date of service. Fee schedules are available on the Provider Information website. (See Key Websites.)
Coverage of Specific Services
The following are coverage rules for specific school-based services.
Assessment to Initiate an IEP
Montana Healthcare Programs covers medical evaluations (assessments) to develop an IEP as long as an IEP is subsequently established and health-related needs are identified.
Therapy Services
Therapy includes speech, occupational and physical therapy services. Services may be performed by a therapy assistant or therapy aide within their scope of practice but must be billed to Montana Healthcare Programs under the school’s supervising licensed therapist’s NPI. (See the Billing Procedures chapter in this manual.)
- Telehealth services are allowed for Physical Therapy, Occupational Therapy and Speech Therapy. All Montana Medicaid covered services delivered via telemedicine/telehealth are reimbursable so long as such services are medically necessary and clinically appropriate for delivery via telemedicine/telehealth.
Services Included
Covered therapy services include the following:
- Restorative therapy services when the particular services are reasonable and necessary to the treatment of the member’s condition and subsequent improvement of function. The amount and frequency of services provided must be indicated on the member’s IEP.
- Assessment services to determine member medical needs and/or to establish an IEP, as long as the assessment results in health-related services documented in the IEP.
Service Requirements
For all therapies being billed, they must be included in the student’s IEP.
Services Restricted
- Montana Healthcare Programs does not cover therapy services that are intended to maintain a member’s current condition but only covers services to improve member functions.
Private Duty Nursing Services
Private duty nursing services are skilled nursing services provided by a registered or licensed practical nurse.
Service Requirements
Montana Healthcare Programs covers private duty nursing services when all of the following requirements are met:
- When the member’s attending physician or mid-level practitioner orders these services in writing
- When prior authorization (PA) is obtained. (See the Prior Authorization chapter in this manual for PA requirements.)
School Psychologists and Mental Health Services
Psychological services in schools are based on determining eligibility for inclusion in special education programming and not necessarily to determine a medical diagnosis outside of the guidelines of the Individuals with Disabilities Education Act.
Services Included
Psychological and mental health services include the following:
- Individual psychological therapy.
- Psychological tests and other assessment procedures when the assessment results in health-related services being written into the IEP.
- Interpreting assessment results.
- Obtaining, integrating, and interpreting information about child behavior and conditions as it affects learning, if it results in an IEP. This only includes direct face-to-face service.
- Mental health and counseling services that are documented on the member’s IEP.
- Consultation with the child’s parent as part of the child’s treatment.
Service Requirements
Montana Healthcare Programs covers psychological counseling services when the following two criteria are met:
- The member’s IEP includes a behavior management plan that documents the need for the services.
- Service is not provided concurrently with CSCT services (unless prior authorization has been obtained).
Services Restricted
Montana Healthcare Programs does not cover the following psychological services:
- Testing for educational purposes
- Psychological evaluation, if provided to a child when an IEP is not subsequently established
- Review of educational records
- Classroom observation
- Scoring tests
Personal Care Paraprofessional Services
Personal care paraprofessional services are medically necessary in-school services provided to members whose health conditions cause them to be limited in performing activities of daily living. That is, these services are provided for members with functional limitations.
The school district must maintain documentation of each service provided, which may take the form of a trip log.
Services Included
These activities of daily living services include:
- Dressing
- Eating
- Escorting on bus
- Exercising (ROM)
- Grooming
- Toileting
- Transferring
- Walking
Service Requirements
- These services must be listed on the member’s IEP.
- Approval must be given by the member’s primary care provider prior to billing for Montana Healthcare Programs covered services. Billing for these services cannot be claimed until the primary care provider signs and dates the Child Profile form. Claiming can start on the date of the signature. This is done by use of the Child Profile Form located in Appendix B.
Services Restricted
Montana Healthcare Programs does not cover the following services provided by a personal care paraprofessional:
- Skilled care services that require professional medical personnel
- Instruction, tutoring or guidance in academics
- Behavioral management
See the Personal Care Paraprofessional Services Documentation, which includes the child profile and service delivery record. The child profile provides detailed examples of activities of daily living.
Montana Healthcare Programs does not cover special transportation services on a day that the member does not receive a Montana Healthcare Programs covered service that is written into the IEP.
Special Needs Transportation
Special needs transportation includes transportation services for members with special needs for the purpose of obtaining non-emergency medical services that are outside of traditional transportation services provided for members without disabilities.
Services Include
Special needs transportation services are covered when all of the following criteria are met:
- Transportation is provided to and/or from a Montana Healthcare Programs-covered service on the day the service was provided.
- The Montana Healthcare Programs-covered service is included in the member’s IEP.
- The member must be in need of a specialized wheelchair or subject to transport by stretcher.
Specialized transportation services are covered if one of the following conditions exists :
- A member requires transportation in a vehicle adapted to service the needs of students with disabilities, including a specially adapted school bus.
- A member resides in an area that does not have school bus transportation (such as those in close proximity to a school).
- The school incurs the expense of the service regardless of the type of transportation rendered.
Services Included
Special needs transportation includes the following:
- Transportation from the member’s place of residence to school (where the member receives health-related services covered by the Montana School-Based Services Program, provided by school), and/or return to the residence.
- Transportation from the school to a medical provider’s office who has a contract with the school to provide health-related services covered by the Montana School-Based Services Program, and return to school.
Services Restricted
Members with special education needs who ride the regular school bus to school with other non-disabled children in most cases will not have a medical need for transportation services and will not have transportation listed in their IEP. In this case, the bus ride should not be billed to the Montana School-Based Services Program. The fact that members may receive a medical service on a given day does not necessarily mean that special transportation also would be reimbursed for that day.
Audiology
Audiology assessments are performed by individuals possessing the state of Montana credentials for performing audiology services.
Services Included
Covered audiology services include the following:
- Assessment to determine member’s medical needs and/or to establish an IEP, as long as the assessment results in health-related services documented in the IEP.
- Services provided must be documented in the member’s IEP.
Service Requirements
Montana Healthcare Programs covers audiology services when the services to be provided during a school year are written into the child’s IEP.
Services Restricted
Montana Healthcare Programs does not cover the following audiology services:
- Testing for educational purposes.
- Services provided during Child Find assessments.
Orientation and Mobility Specialist Services
Orientation and Mobility Specialist services are medically necessary in-school services provided to students to alleviate movement deficiencies resulting from a lack of vision.
Orientation and Mobility Specialists need to have a certification by the Academy for Certification of Vision Rehabilitation and Education Professionals (ACVREP) or a National Orientation & Mobility Certification (NOMC) offered by the National Blindness Professional Certification Board (NBPCB). The credential is valid for a period of 5 years and is renewable by documenting work and/or participation in professional activities.
Services Included
Orientation & Mobility Specialist service include the following:
- Sensory integrative techniques to enhance sensory processing and promote adaptive responses to environmental demands, direct one-on-one member contact by provider. This includes assessment type services.
- Self-care/home management training (e.g., ADLs and compensatory training, instruction in use of assistive technology devices/adaptive equipment) direct one-on-one contact by provider.
- See School-Based fee schedule online for the correct CPT codes to use when billing.
Authorization Requirements Summary
The following table is a summary of authorization requirements for school-based services that were described in each section above. For more information on how to obtain prior authorization and Passport provider approval, see the Prior Authorization and Passport to Health chapters in this manual.
Authorization Requirements
Service: Therapy
Prior Authorization: No
Passport Provider Approval: No
Written Physician Order/Referral: No
Service: Private Duty Nursing
Prior Authorization: Yes
Passport Provider Approval: No
Written Physician Order/Referral: Yes
Service: School Psychologist and Mental Health
Prior Authorization: No
Passport Provider Approval: No
Written Physician Order/Referral: No
Service: Personal Care Paraprofessional
Prior Authorization: No
Passport Provider Approval: No
Written Physician Order/Referral: Yes (Child Profile Form is signed by child’s physician.)
Service: Specialized Transportation
Prior Authorization: No
Passport Provider Approval: No
Written Physician Order/Referral: No
Service: Audiology
Prior Authorization: No
Passport Provider Approval: No
Written Physician Order/Referral: No
Service: Orientation & Mobility
Prior Authorization: No
Passport Provider Approval: No
Written Physician Order/Referral: No
Other Programs
This is how the information in this chapter applies to Department programs other than School-Based Services outlined within this manual.
Children’s Mental Health Services
In addition to the school-based services outlined in this manual, the Children’s Mental Health Bureau (CMHB) offers Comprehensive School and Community treatment (CSCT) and other mental health services. Please contact CMHB at (406) 444-4545 for more information or click the following links:
Children’s Mental Health Bureau Website
Children's Mental Health Medicaid Services Provider Manual
Medicaid Mental Health for Youth Fee Schedule
Administrative Rules of Montana:
- 37.87: CHILDREN'S MENTAL HEALTH SERVICES
- 37.106: HEALTH CARE FACILITIES/Subchapter 19 Minimum Standards for Mental Health Centers
Healthy Montana Kids (HMK)
The school-based services in this manual are not covered benefits of Healthy Montana Kids (HMK). Additional information regarding HMK benefits is available by contacting Blue Cross and Blue Shield of Montana (BCBSMT) at 1-800-447-7828 (toll-free) or 406-447-7828 (Helena).
End of Covered Services Chapter
Passport to Health Program
What Is Passport to Health? (ARM 37.86.5101–5120, ARM 37.86.5303, and ARM 37.86.5201–5206)
Passport to Health is the managed care program for Montana Healthcare Programs and
Healthy Montana Kids (HMK) Plus members. The four Passport programs encourage
and support Montana Healthcare Programs and HM Plus members and providers in establishing a
medical home and in ensuring the appropriate use of Montana Healthcare Programs and HMK Plus services:
- Passport to Health Primary Care Case Management
- Team Care
Montana Healthcare Programs and HMK Plus members who are eligible for Passport must enroll in the program (about 70% of Montana Healthcare Programs and HMK Plus members are eligible) Each enrollee has a designated Passport provider who is typically a physician, mid-level practitioner, or primary care clinic.
Montana Healthcare Programs does not pay for services when prior authorization or Passport requirements are not met.
Passport to Health Primary Care Case Management (ARM 37.86.5101–5120)
The Passport provider provides primary care case management (PCCM) services to their members. This means he/she provides or coordinates the member’s care and makes referrals to other Montana Healthcare Programs and HMK Plus providers when necessary. Under Passport, Montana Healthcare Programs, and HMK Plus members choose one primary care provider (PCP) and develop an ongoing relationship that provides a medical home. The medical home is a concept that encourages a strong doctor–member relationship. An effective medical home is accessible, continuous, comprehensive, coordinated, and operates within the context of family and community.
With some exceptions, all services to Passport members must be provided or approved by the member’s Passport provider or Montana Healthcare Programs/HMK Plus will not reimburse for those services. The member’s Passport provider is also referred to as the PCP. (See the section titled Services That Do Not Require Passport Provider Approval in this chapter.)
Different codes are issued for Passport approval and prior authorization, and both must be recorded on the claim form, if appropriate.
Team Care (ARM 37.86.5303)
Team Care is designed to educate members to effectively access medical care. Members with a history of using services at an amount or frequency that is not medically necessary are enrolled in Team Care. Members enrolled in Team Care are also enrolled in Passport. Team Care follows the same Passport rules and guidelines for referrals, enrollment/disenrollment, prior authorization, and billing processes. However, while Passport members can change providers without cause, as often as once a month, Team Care members are locked in to one provider and one pharmacy. Providers are encouraged to make a referral to the Team Care Program Officer if they feel one of their members is appropriate for the program. A Passport provider receives an enhanced case management fee of $6 per member per month for Team Care members. When checking Montana Healthcare Programs or HMK Plus eligibility on the MATH web portal, a Team Care member’s provider and pharmacy will be listed. (See Key Websites.) Write all Montana Healthcare Programs and HMK Plus prescriptions to the designated pharmacy.
In practice, providers will most often encounter Montana Healthcare Programs and HMK Plus members who are enrolled in Passport. Specific services may also require prior authorization (PA) even if the member is a Passport enrollee. Specific PA requirements can be found in the provider fee schedules. For more information on Passport to Health, see the General Information for Providers manual.
Other Programs
Members who are enrolled in the Mental Health Services Plan (MHSP) or Healthy Montana Kids (HMK) are not enrolled in Passport, so the Passport requirements in this chapter do not apply.
For more HMK information, contact Blue Cross and Blue Shield of Montana at 1-800-447-7828 (toll-free) or 447-7828 (Helena) Additional HMK information is available on the HMK website. (See Key Websites.)
End of Passport to Health Program Chapter
Prior Authorization
Prior authorization refers to a list of services that require approval from the Montana Healthcare Program prior to the service being rendered. If a service requires prior authorization, the requirement exists for all Montana Healthcare Programs members. When prior authorization is granted, a prior authorization number is issued and must be on the claim.
Different codes are issued for Passport approval and prior authorization; when necessary, both must be on the claim form. Montana Healthcare Programs does not pay for services when prior authorization requirements are not met.
Prior Authorization for Retroactively Eligible Members
When a member is determined retroactively eligible for Montana Healthcare Programs, the member should give the provider a Notice of Retroactive Eligibility (160-M). The provider has 12 months from the date retroactive eligibility was determined to bill for those services. When a member becomes retroactively eligible for Montana Healthcare Programs the provider may:
- Accept the member as a Montana Healthcare Programs member from the current date.
- Accept the member as a Montana Healthcare Programs member from the date retroactive eligibility was effective.
- Require the member to continue as a private-pay member.
Providers may choose whether to accept retroactive eligibility. All prior authorization requirements must be met to receive Montana Healthcare Programs payment. When requesting prior authorization, attach a copy of the 160-M to the prior authorization request. It is the member’s responsibility to ensure his/her caseworker prepares a 160-M for each provider who participates in the member’s healthcare during this retroactive period. See the Billing Procedures chapter in this manual for retroactive eligibility billing requirements. When seeking prior authorization, keep in mind the following:
- The referring provider should initiate all authorization requests.
- Always refer to the current Montana Healthcare Programs fee schedule to verify if prior authorization is required for specific services.
- For a list of services that require prior authorization, who to contact, and documentation requirements, see the Contact Us link in site index in the Provider Information website menu. The Contact Us can be located in the site index in the left menu of the Provider Website.
- Prior authorization criteria forms for most services are available on the Forms page of the Provider Information website .
- When prior authorization is granted from Mountain-Pacific Quality Health (MPQH), providers receive notification from both MPQH and Conduent Claims Processing. The Prior Authorization Notice from Claims Processing has a prior authorization number which must be included on the claim.
End of Prior Authorization Chapter
Coordination of Benefits
When Members Have Other Coverage
Montana Healthcare Programs members often have coverage through Medicare, workers’ compensation, employment-based coverage, individually purchased coverage, etc. Coordination of benefits is the process of determining which source of coverage is the primary payer in a particular situation. In general, providers must bill other carriers before billing Montana Healthcare Programs, but there are some exceptions. (See Exceptions to Billing Third Party First later in this chapter.) Medicare coverage is processed differently than other sources of coverage.
Identifying Other Sources of Coverage
The member’s Montana Healthcare Programs eligibility verification may identify other payers such as Medicare or other third-party payers. (See Member Eligibility and Responsibilities in the General Information for Providers manual.) If a member has Medicare, the Medicare ID number is provided. If a member has other coverage (excluding Medicare), it will be shown under the TPL section.
Some examples of third-party payers include:
- Private health insurance
- Employment-related health insurance
- Workers’ compensation insurance*
- Health insurance from an absent parent
- Automobile insurance*
- Court judgments and settlements*
- Long-term care insurance
*These third-party payers (and others) may not be listed on the member’s Montana Healthcare Programs eligibility verification.
Providers must use the same procedures for locating third party sources for Montana Healthcare Programs members as for their non-Montana Healthcare Programs members. Providers cannot refuse service because of a third party payer or potential third-party payer.
When a Member Has Medicare
Medicare claims are processed and paid differently than claims involving other payers. The other sources of coverage are referred to as third-party liability (TPL), but Medicare is not.
Medicare Part B Crossover Claims
Medicare Part B covers outpatient hospital care, physician care, and other services including those provided in a school setting. The Department has an agreement with Medicare Part B carrier for Montana (Noridian) and the Durable Medical Equipment Regional Carrier [DMERC]). Under this agreement, the carrier provide the Department with a magnetic tape of claims for members who have both Medicare and Montana Healthcare Programs coverage. Providers must tell Medicare that they want their claims sent to Montana Healthcare Programs automatically and must have their NPI on file with Montana Healthcare Programs.
To avoid confusion and paperwork, submit Medicare Part B crossover claims to Montana Healthcare Programs only when necessary.
In these situations, providers need not submit Medicare Part B crossover claims to Montana Healthcare Programs. Medicare will process the claim, submit it to Montana Healthcare Programs, and send the provider an Explanation of Medicare Benefits (EOMB). Providers must check the EOMB for the statement indicating that the claim has been referred to Montana Healthcare Programs for further processing. It is the provider’s responsibility to follow up on crossover claims and make sure they are correctly billed to Montana Healthcare Programs within the timely filing limit. (See Billing Procedures.)
When Medicare Pays or Denies a Service
- When Medicare automatic crossover claims are paid or denied, they should automatically cross over to Montana Healthcare Programs for processing, so the provider does not need to submit the claim to Montana Healthcare Programs.
- When Medicare crossover claims are billed on paper and are paid or denied, the provider must submit the claim to Montana Healthcare Programs with the Medicare EOMB (and the explanation of denial codes).
When submitting electronic claims with paper attachments, see the Billing Electronically with Paper Attachments section of the Billing Procedures chapter in this manual.
When Montana Healthcare Programs Does Not Respond to Crossover Claims
When Montana Healthcare Programs does not respond within 45 days of the provider receiving the Medicare EOMB, submit a claim with a copy of the Medicare EOMB to Montana Healthcare Programs for processing.
Submitting Medicare Claims to Montana Healthcare Programs
When submitting a paper claim to Montana Healthcare Programs, use Montana Healthcare Programs billing instructions and codes. Medicare’s instructions, codes, and modifiers may not be the same as Montana Healthcare Programs’s. The claim must include the provider’s NPI and Montana Healthcare Programs member ID number. The Medicare EOMB and explanation of denial codes are required only if the claim was denied.
Remember to submit Medicare crossover claims to Montana Healthcare Programs only when:
- The referral to Montana Healthcare Programs statement is missing from the provider’s EOMB.
- The provider does not hear from Montana Healthcare Programs within 45 days of receiving the Medicare EOMB.
- Medicare denies the claim.
All Part B crossover claims submitted to Montana Healthcare Programs before Medicare’s 45-day response time will be returned to the provider.
When a Member Has TPL (ARM 37.85.407)
When a Montana Healthcare Programs member has additional medical coverage (other than Medicare), it is often referred to as third party liability (or TPL). In most cases, providers must bill other insurance carriers before billing Montana Healthcare Programs.
If a parent determines that billing their insurance would cause a financial hardship (e.g., decrease lifetime coverage or increase premiums), and refuses to let the school bill the insurance plan, the school cannot bill Montana Healthcare Programs for these services based on requirements of IDEA.
Providers are required to notify their members that any funds the member receives from third party payers equal to what Montana Healthcare Programs paid (when the services were billed to Montana Healthcare Programs) must be turned over to the Department. Amounts in excess of what Montana Healthcare Programs paid must be returned to the provider. The following words printed on the member’s statement will fulfill this requirement: “When services are covered by Montana Healthcare Programs and another source, any payment the member receives from the other source must be turned over to Montana Healthcare Programs.”
If a parent refuses to let the school bill their insurance plan, Montana Healthcare Programs cannot be billed either.
Billing for Montana Healthcare Programs Covered Services When No IEP Exists
In order to bill for Montana Healthcare Programs covered services that are not in the member’s IEP, the school must meet all the following requirements:
- A fee schedule is established for health-related services (can be a sliding scale to adjust for individuals with low incomes)
- The provider determines if each individual who receives services has insurance coverage or will be billed on a private-pay basis
- The provider bills all individuals and/or the insurance carrier for the medical service provided
If the school bills private pay members, then they must bill as follows for the services provided:
Member Insurance Status: Montana Healthcare Programs only*
Billing Process: Bill Montana Healthcare Programs
Member Insurance Status: Private pay, no Montana Healthcare Programs
Billing Process: Bill family
Member Insurance Status: Private insurance/Montana Healthcare Programs*
Billing Process: Bill private insurance before Montana Healthcare Programs
Member Insurance Status: Private insurance, no Montana Healthcare Programs*
Billing Process: Bill private insurance
*Note: Under FERPA, schools must have written parental permission for release of information before billing Montana Healthcare Programs. For billing third party insurances, schools must have written permission for billing and written permission for release of information.
Billing for Montana Healthcare Programs Covered Services under an IEP
If a child is covered by both Montana Healthcare Programs and private insurance, and the services are provided under an IEP, providers must bill as follows:
Member Insurance Status: Montana Healthcare Programs only*
Billing Process: Bill Montana Healthcare Programs
Member Insurance Status: Private pay, no Montana Healthcare Programs
Billing Process: Not required to bill family
Member Insurance Status: Private insurance/Montana Healthcare Programs*
Billing Process: Bill private insurance before Montana Healthcare Programs
Member Insurance Status: Private insurance, no Montana Healthcare Programs
Billing Process: Not required to bill private insurance
*Note: Under FERPA, schools must have written parental permission for release of information before billing Montana Healthcare Programs. For billing third party insurances, schools must have written permission for billing and written permission for release of information.
Exceptions to Billing Third Party First
In a few cases, providers may bill Montana Healthcare Programs first.
- When a Montana Healthcare Programs member is also covered by Indian Health Service (IHS) or the Montana Crime Victims Compensation Fund, providers must bill Montana Healthcare Programs before IHS or Crime Victims. These are not considered third party liability.
- When a child is covered under BCBSMT or HMK, providers may bill Montana Healthcare Programs first since these insurances do not cover services provided in a school setting.
- Montana Healthcare Programs must be billed before IDEA funds are used.
- Effective April 1, 2013, when a child is also covered by another insurance, and the service is provided by a school-based provider, no blanket denial form is required nor is any information from the third-party liability.
Requesting an Exemption
Providers may request to bill Montana Healthcare Programs first under certain circumstances. In each of these cases, the claim and required information must be sent directly to the TPL Unit. (See Key Contacts.)
- If another insurance has been billed, and 90 days have passed with no response, include a note with the claim explaining that the insurance company has been billed, or include a copy of the letter sent to the insurance company. Include the date the claim was submitted to the insurance company and certification that there has been no response.
- When the provider has billed the third-party insurance and has received a non-specific denial (e.g., no member name, date of service, amount billed), submit the claim with a copy of the denial and a letter of explanation directly to Montana Healthcare Programs in order to avoid missing the timely filing deadline.
- When the Child Support Enforcement Division has required an absent parent to have insurance on a child, the claim can be submitted to Montana Healthcare Programs when the following requirements are met:
- The third-party carrier has been billed, and 30 days or more have passed since the date of service.
- The claim is accompanied by a certification that the claim was billed to the third-party carrier, and payment or denial has not been received.
When the Third-Party Pays or Denies a Service
When a third-party payer is involved (excluding Medicare) and the other payer:
- Pays the claim, indicate the amount paid in the “prior payments” form locator of the claim when submitting to Montana Healthcare Programs for processing.
- Allows the claim, and the allowed amount went toward member’s deductible, include the insurance EOB when billing Montana Healthcare Programs.
- Denies the claim, include a copy of the denial (including the denial reason codes) with the claim and submit to Montana Healthcare Programs. If a blanket denial is provided, the Department will accept and allow this denial for a period of no more than two years. The school must include a copy of this blanket denial with each submission for health-related services for each member. The blanket denial must be specific to the provider, member, and health related services provided to the member. Blanket denials issued to schools without a member’s name will not be accepted.
- Denies a line on the claim, bill the denied lines together on a separate claim and submit to Montana Healthcare Programs. Include the explanation of benefits (EOB) from the other payer as well as an explanation of the reason for denial (e.g., definition of denial codes).
If the provider receives a payment from a third party after the Department has paid the provider, the provider must return the lower of the two payments to the Department within 60 days.
When the Third Party Does Not Respond
If another insurance has been billed and 90 days have passed with no response, bill Montana Healthcare Programs as follows:
- Include a note with the claim explaining that the insurance company has been billed, or include a copy of the letter sent to the insurance company.
- Include the date the claim was submitted to the insurance company.
- Send this information to the Third-Party Liability Unit. (See Key Contacts.)
End of Coordination of Benefits Chapter
Billing Procedures
Claim Forms
Services provided by the health care professionals covered in this manual must be billed either electronically on a Professional claim or on a CMS-1500 paper claim form. CMS-1500 forms are available from various publishing companies; they are not available from the Department or Provider Relations.
Timely Filing Limits (ARM 37.85.406)
Providers must submit clean claims to Montana Healthcare Programs within:
Twelve months from whichever is later:
- the date of service
- the date retroactive eligibility or disability is determined
For claims involving Medicare or TPL, if the 12-month time limit has passed, providers must submit clean claims to Montana Healthcare Programs.
- Medicare Crossover Claims: Six months from the date on the Medicare explanation of benefits approving the service (if the Medicare claim was timely filed and the member was eligible for Medicare at the time the Medicare claim was filed).
- Claims Involving Other Third-Party Payers (excluding Medicare): Six months from the date on an adjustment notice from a third party payer who has previously processed the claim for the same service, and the adjustment notice is dated after the periods described above.
Clean claims are claims that can be processed without additional information or action from the provider. The submission date is defined as the date that the claim was received by the Department or the claims processing contractor. All problems with claims must be resolved within this 12-month period.
Tips to Avoid Timely Filing Denials
- Correct and resubmit denied claims promptly (see the Remittance Advices and Adjustments chapter in this manual).
- If a claim submitted to Montana Healthcare Programs does not appear on the remittance advice within 45 days, contact Provider Relations for claim status. (See Key Contacts.)
- If another insurer has been billed and 90 days have passed with no response, you can bill Montana Healthcare Programs. (See the Coordination of Benefits chapter in this manual for more information.)
- To meet timely filing requirements for Medicare/Montana Healthcare Programs crossover claims, see the Coordination of Benefits chapter in this manual.
When Providers Cannot Bill Montana Healthcare Programs Members (ARM 37.85.406)
In most circumstances, providers may not bill Montana Healthcare Programs members for services covered under Montana Healthcare Programs.
More specifically, providers cannot bill members directly:
- For the difference between charges and the amount Montana Healthcare Programs paid.
- For a covered service provided to a Montana Healthcare Programs-enrolled member who was accepted as a Montana Healthcare Programs member by the provider, even if the claim was denied.
- When the provider bills Montana Healthcare Programs for a covered service, and Montana Healthcare Programs denies the claim because of billing errors.
- When a third-party payer does not respond.
- When a member fails to arrive for a scheduled appointment.
- When services are free to the member and free to non-Montana Healthcare Programs covered individuals.
If a provider bills Montana Healthcare Programs and the claim is denied because the member is not eligible, the provider may bill the member directly.
Member Co-Payment (ARM 37.85.204 and 37.85.402)
Effective for all claims paid on or after January 1, 2020 co-payment will not be assessed.
Billing for Members with Other Insurance
If a Montana Healthcare Programs member is also covered by Medicare, has other insurance, or some other third party is responsible for the cost of the member’s health care, see the Coordination of Benefits chapter in this manual.
Billing for Retroactively Eligible Members
When a member becomes retroactively eligible for Montana Healthcare Programs, the provider may:
- Accept the member as a Montana Healthcare Programs member from the current date.
- Accept the member as a Montana Healthcare Programs member from the date retroactive eligibility was effective.
- Require the member to continue as private pay.
When the provider accepts the member’s retroactive eligibility, the provider has 12 months from the date retroactive eligibility was determined to bill for those services. When submitting claims for retroactively eligible members, attach a copy of the FA-455 (eligibility determination letter) to the claim if the date of service is more than 12 months earlier than the date the claim is submitted. Providers may need to contact the member’s local office of public assistance. (See the General Information for Providers manual.)
When a provider chooses to accept the member from the date retroactive eligibility was effective, and the member has made a full or partial payment for services, the provider must refund the member’s payment for the services before billing Montana Healthcare Programs for the services.
Service Fees
The Office of Management and Budget (OMB A-87) federal regulation specifies one government entity may not bill another government entity more than their cost. Schools should bill Montana Healthcare Programs their cost of providing a service, not the fee published by Montana Healthcare Programs for the service. The Montana Healthcare Programs fee schedule is to inform provider of the maximum fee Montana Healthcare Programs pays for each procedure.
Coding Tips
The procedure codes listed in the following table are valid procedures for schools to use for billing Montana Healthcare Programs.
School-Based Services Codes
Occupational Therapist
Service: Occupational therapy – individual therapeutic activities
CPT Code: 97530
Unit Measurement: 15-minute unit
Service: Occupational therapy – group therapeutic procedures
CPT Code: 97150
Unit Measurement: Per visit
Service: Occupational therapy evaluation - low 20 minutes
CPT Code: 97165
Unit Measurement: Per visit
Service: Occupational therapy evaluation - moderate - 30 minutes
CPT Code: 97166
Unit Measurement: Per visit
Service: Occupational therapy evaluation - high - 45minutes
CPT Code: 97167
Unit Measurement: Per visit
Service: Occupational therapy re-evaluation
CPT Code: 97168
Unit Measurement: Per visit
Physical Therapist
Service: Physical therapy – individual therapeutic activities
CPT Code: 97530
Unit Measurement: 15-minute unit
Service: Physical therapy – group therapeutic procedures
CPT Code: 97150
Unit Measurement: Per visit
Service: Physical therapy evaluation - low - 20 minutes
CPT Code: 97161
Unit Measurement: Per visit
Service: Physical therapy evaluation - moderate - 30 minutes
CPT Code: 97162
Unit Measurement: Per visit
Service: Physical therapy evaluation - high 45 minutes
CPT Code: 97163
Unit Measurement: Per visit
Service: Physical therapy re-evaluation
CPT Code: 97164
Unit Measurement: Per visit
Speech Therapists
Service: Treatment of Speech Disorder; individual
CPT Code: 92507
Unit Measurement: Per visit
Service: Treatment of Speech Disorder; group
CPT Code: 92508
Unit Measurement: Per visit
Service: Evaluation of speech fluency
CPT Code: 92521
Unit Measurement: Per visit
Service: Evaluation of speech sound production
CPT Code: 92522
Unit Measurement: Per visit
Service: Evaluation of speech sound with language comprehension
CPT Code: 92523
Unit Measurement: Per visit
Private Duty Nursing
Service: Private duty nursing services provided in school
CPT Code: T1000
Unit Measurement: 15-minute unit
School Psychologist/Mental Health Services
Service: Psychological therapy – individual
CPT Code: 90832
Unit Measurement: Per 30-minute unit
Service: Psychological therapy – group
CPT Code: 90853
Unit Measurement: Per visit
Service: Psychological testing by Psychologist
CPT Code: 96101
Unit Measurement: Per 1 hour
Personal Care Paraprofessionals
Service: Personal care services
CPT Code: T1019
Unit Measurement: 15-minute unit
Special Needs Transportation
Service: Special needs transportation
CPT Code: T2003
Unit Measurement: Per one-way trip
Audiology
Service: Comprehensive Hearing Test
CPT Code: 92557
Unit Measurement: Per visit
Service: Tympanometry
CPT Code: 92567
Unit Measurement: Per visit
Service: Evoked otoacoustic emission; limited
CPT Code: 92587
Unit Measurement: Per visit
Orientation & Mobility
Service: Sensory integrative techniques
CPT Code: 97533
Unit Measurement: 15-minute unit
Service: Self-care/home management training
CPT Code: 97535
Unit Measurement: 15-minute unit
Using Modifiers
School-based services providers only use modifiers for coding when the service provided to a member is not typical. The modifiers are used in addition to the CPT codes. The following modifiers may be used in schools:
- Modifier 52 is billed with the procedure code when a service is reduced from what the customary service normally entails. For example, a service was not completed in its entirety as a result of extenuating circumstances or the well-being of the individual was threatened.
- Modifier 22 is billed with the procedure code when a service is greater than the customary service normally entails. For example, this modifier may be used when a service is more extensive than usual or there was an increased risk to the individual. Slight extension of the procedure beyond the usual time does not validate the use of this modifier.
- Modifier 59 is billed for therapies in accordance with the Correct Coding Initiative (CCI) and to be used when codes are considered mutually exclusive or a component of one another.
- Modifiers may also be required when providing two services in the same day that use the same code. See the section titled Multiple Services on the Same Date” for more information.
Multiple Services on the Same Date
When a provider bills Montana Healthcare Programs for two services that are provided on the same day that use the same CPT code and are billed under the same NPI and taxonomy, a modifier should be used to prevent the second service from being denied. The modifier GO is used for occupational therapy, and modifier GP is used for physical therapy. One of the codes needs to have modifier 59 also for the CCI edit. For example, a school bills with one NPI and taxonomy for all services. The school provided occupational therapy for a member in the morning, and physical therapy for the same member in the afternoon of October 14, 2003. The claim would be billed like this:
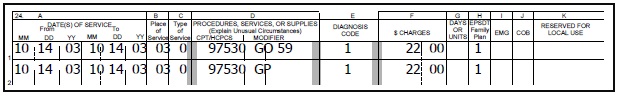
Time and Units
- A provider may bill only time spent directly with a member. Time spent traveling to provide a service and paperwork associated with the direct service cannot be included in the time spent providing a service.
- Some CPT codes are designed to bill in units of 15 minutes (or other time increment) and others are per visit.
- If the service provided is using a per visit code, providers should use one unit of service per visit.
- When using codes that are based on a 15-minute time unit, providers should bill one unit of service for each 15-minute period of service provided. Units round up to the next unit after 8 minutes.
Place of Service
The only place of service code Montana Healthcare Programs will accept is “03” (schools).
Billing for Specific Services
The following are instructions for billing for school-based services. For details on how to complete a CMS-1500 claim form, see the Submitting a Claim chapter in this manual.
School-based providers can only bill services in the amount, scope, and duration listed in the IEP.
Assessment to Initiate an IEP
When billing for assessments (evaluations), use the CPT code for the type of service being billed. When the unit measurement is “per visit,” only one unit may be billed for the assessment/evaluation. If the evaluation is completed over the course of several days, it is considered one evaluation. Bill the date span with 1 unit of service, not multiple units of service. For example, a speech/hearing evaluation completed over a three-day period would be billed like this:
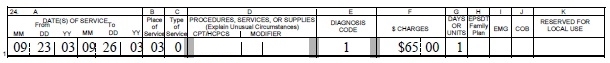
A two-hour psychological assessment (evaluation) would be billed like this (the unit measurement for this code is “per hour”):
Therapy Services
Services may be performed by a therapy assistant or therapy aide but must be billed to Montana Healthcare Programs under the school’s NPI and taxonomy. Remember to use the CCI edit modifier for all three types of therapy: speech, occupational and physical. See the Submitting a Claim chapter in this manual. Thirty minutes of individual physical therapy would be billed like this (the unit measurement for this code is “15-minute unit”):
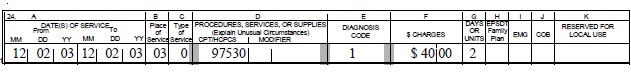
Private Duty Nursing Services
Prior authorization is required for these services, so remember to include the prior authorization number on the claim. (See the Submitting a Claim chapter in this manual.) Private duty nursing services provided for 15 minutes would be billed like this:
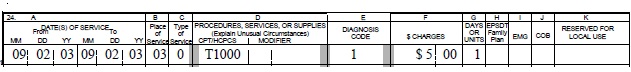
Montana Healthcare Programs covered services provided under an IEP are exempt from the “free care rule.”
School Psychologists and Mental Health Services
A psychological therapy session of 30 minutes would be billed like this (the unit measurement for this code is per 30-minute unit):
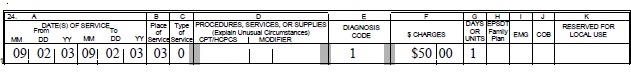
Personal Care Paraprofessional Services
Personal care services provided to a member for 2 hours during a day would be billed like this (the unit measurement for this code is per 15-minute unit):
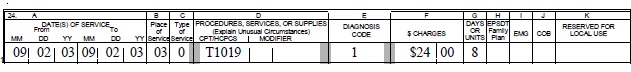
Special Needs Transportation
School districts must maintain documentation of each service provided, which may take the form of a trip log. Schools must bill only for services that were provided. Special transportation should be billed on a per one-way trip basis. For example, if a member was transported from his/her residence to school and received Montana Healthcare Programs covered health-related services that day, and then transported back to his/her residence, it would be billed like this:
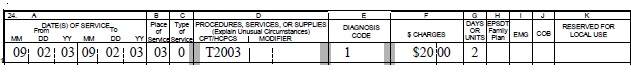
Audiology
An audiology assessment would be billed like this (the unit measurement for this code is per visit):
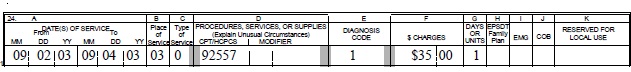
Submitting Electronic Claims
Providers who submit claims electronically experience fewer errors and quicker payment. Claims may be submitted using the methods below. For detailed submission methods, see the electronic submissions manual on the Electronic Billing page of the website.
- WINASAP 5010. This free software provided by Conduent allows for the creation of basic claim submissions. Please note that this software is not compatible with Windows 10 and has limited support as it is free software.
- Utilizes either a dial-up modem or submissions through the Montana Access to Health (MATH) Web Portal.
- Requires completion of the X12N Transaction Packet to allow for claim submissions.
- Clearinghouses/Contracted Claim Submitter. Providers can make arrangements with a clearinghouse/contracted claim submitter for claim submission. Please note that the clearinghouse must be enrolled to submit claims to Montana Healthcare Programs.
- Montana Access to Health (MATH) Web Portal . A secure website that allows providers to verify eligibility, check claim status, and view medical claims history. Valid X12N files can be uploaded through this website.
- MoveIt DMZ. This secure transfer protocol is for providers and clearinghouses that submit large volumes of files (in excess of 20 per day) or are regularly submitting files larger than 2 MB. This utilizes SFTP and an intermediate storage area for the exchange of files.
- A request for this must be made through Conduent Provider Relations for established trading partners.
Providers should be familiar with federal rules and regulations related to electronic claims submission. For more information on electronic claims submission options, contact Provider Relations or the EDI Technical Help Desk. (See the Key Contacts chapter.) Providers should be familiar with federal rules and regulations and Montana-specific information for sending and receiving electronic transactions. They are available on the EDI Gateway website. (See Key Websites.)
Billing Electronically with Paper Attachments
When submitting claims that require additional supporting documentation, the Attachment Control Number field must be populated with an identifier. Identifier formats can be designed by software vendors or clearinghouses, but the preferred method is the provider’s NPI followed by the member’s ID number and the date of service, each separated by a dash:
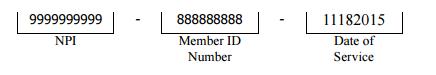
The supporting documentation must be submitted with a paperwork attachment cover sheet. See the Forms page of the Provider Information website. The number in the paper Attachment Control Number field must match the number on the cover sheet.
Submitting Paper Claims
For instructions on completing a paper claim, see the Submitting a Claim chapter in this manual. Unless otherwise stated, all paper claims must be mailed to:
Claims Processing
P.O. Box 8000
Helena, MT 59604
Claim Inquiries
Contact Provider Relations for claim questions, or questions regarding payments, denials, member eligibility.
Provider Relations will respond to the inquiry within 10 days. The response will include the status of the claim, paid (date paid), denied (date denied), or in process. Denied claims will include an explanation of the denial and steps to follow for payment (if the claim is payable).
The Most Common Billing Errors and How to Avoid Them
Paper claims are often returned to the provider before they can be processed, and many other claims (both paper and electronic) are denied.
To avoid unnecessary returns and denials, double check each claim to confirm the following items are included and accurate.
Common Billing Errors
Reasons for Return or Denial: Provider NPI missing or invalid
How to Prevent Returned or Denied Claims: The provider NPI is a 10-digit number assigned to the provider by the National Plan and Provider Enumeration System. Verify the correct provider NPI is on the claim.
Reasons for Return or Denial: Authorized signature missing
How to Prevent Returned or Denied Claims: Each claim must have an authorized signature belonging to the provider, billing clerk, or office personnel. The signature may be typed, stamped, hand-written, or computer generated.
Reasons for Return or Denial: Signature date missing
How to Prevent Returned or Denied Claims: Each claim must have a signature date.
Reasons for Return or Denial: Incorrect claim form used
How to Prevent Returned or Denied Claims: The claim must be the correct form for the provider type. Services covered in this manual require a CMS-1500 claim form (or electronic Professional claim).
Reasons for Return or Denial: Information on claim form not legible
How to Prevent Returned or Denied Claims: Information on the claim form must be legible. Use dark ink and center the information in the form locator. Information must not be obscured by lines.
Reasons for Return or Denial: Member number not on file, or member was not eligible on date of service
How to Prevent Returned or Denied Claims: Before providing services to the member, verify member eligibility by using one of the methods described in the Member Eligibility and Responsibilities chapter of the General Information for Providers manual. Montana Healthcare Programs eligibility may change monthly.
Reasons for Return or Denial: Prior authorization number is missing
How to Prevent Returned or Denied Claims: Prior authorization (PA) is required for certain services, and the PA number must be on the claim. See the Prior Authorization chapters in this manual.
Reasons for Return or Denial: Prior authorization does not match current information
How to Prevent Returned or Denied Claims: Claims must be billed and services performed during the prior authorization span. The claim will be denied if it is not billed according to the spans on the authorization.
Reasons for Return or Denial: Duplicate claim
How to Prevent Returned or Denied Claims: Check all remittance advices (RAs) for previously submitted claims before resubmitting. When making changes to previously paid claims, submit an adjustment form rather than a new claim (see the Remittance Advices and Adjustments chapter in this manual).
Reasons for Return or Denial: TPL on file and no credit amount on claim
How to Prevent Returned or Denied Claims: If the member has any other insurance (or Medicare), bill the other carrier before Montana Healthcare Programs. See the Coordination of Benefits chapter in this manual. If the member’s TPL coverage has changed, providers must notify the TPL unit (see the Key Contacts chapter) before submitting a claim.
Reasons for Return or Denial: Claim past 12-month filing limit
How to Prevent Returned or Denied Claims: The Claims Processing Unit must receive all clean claims and adjustments within the timely filing limits described in this chapter. To ensure timely processing, claims and adjustments must be mailed to Claims Processing at the address shown in the Key Contacts chapter.
Reasons for Return or Denial: Missing Medicare EOMB
How to Prevent Returned or Denied Claims: All denied Medicare crossover claims must have an Explanation of Medicare Benefits (EOMB) with denial reason codes attached, and be billed to Montana Healthcare Programs on paper.
Reasons for Return or Denial: Provider is not eligible during dates of services, enrollment has lapsed due to licensing requirements, or provider NPI terminated
How to Prevent Returned or Denied Claims: Out-of-state providers must update licensure for Montana Healthcare Programs enrollment early to avoid denials. If enrollment has lapsed due to expired licensure, claims submitted with a date of service after the expiration date will be denied until the provider updates his or her enrollment. New providers cannot bill for services provided before Montana Healthcare Programs enrollment begins. If a provider is terminated from the Montana Healthcare Programs, claims submitted with a date of service after the termination date will be denied.
Reasons for Return or Denial: Procedure is not allowed for provider type
How to Prevent Returned or Denied Claims: Provider is not allowed to perform the service. Verify the procedure code is correct using current HCPCS and CPT billing manual. Check the appropriate Montana Healthcare Programs fee schedule to verify the procedure code is valid for your provider type.
Other Programs
The Mental Health Services Plan (MHSP) and Healthy Montana Kids (HMK) do not cover school-based services. For more information on these programs, visit the Provider Information website.
End of Billing Procedures Chapter
Submitting a Claim
The services described in this manual are billed either electronically on a Professional claim or on a CMS-1500 paper claim form. Claims submitted with all of the necessary information are referred to as “clean” and are usually paid in a timely manner (see the Billing Procedures chapter in this manual). When completing a claim, remember the following:
- Required fields are indicated by *. For detailed submission methods, see the electronic submissions manual on the Electronic Billing page of the website
- Fields that are required if the information is applicable to the situation or member are indicated by **.
- Field 24h, EPSDT/Family Planning, is used as an indicator to specify additional details for certain members or services. The following are accepted codes:
EPSDT/Family Planning Indicator
Code: 1 Member/Service: EPSDT
Purpose: Overrides some benefit limits for member under age 21.
Code: 2 Member/Service: Family planning
Purpose: Overrides the Montana Healthcare Programs Passport authorization on the line.
Code: 3 Member/Service: EPSDT and family planning
Purpose: Overrides Montana Healthcare Programs cost sharing and Passport authorization for persons under the age of 21.
Code: 6 Member/Service: Nursing facility member
Purpose: Overrides the Medicare edit for oxygen services on the line.
- Unless otherwise stated, all paper claims must be mailed to the following address:
Claims Processing Unit
P.O. Box 8000
Helena, MT 59604
Sample Claim
Member Information
Field: 2*
Field Title: Member's Name
Instructions: Enter member's name as seen on member’s Montana Health Care Programs information
Field: 10d *
Field Title: Member’s ID
Instructions: Enter the member’s ID number as it appears on the member’s Montana Health Care Programs information.
Field: 1a, 9a, 11**
Field Title: Member’s ID
Instructions: If member’s ID is not located in 10d these three fields are searched for the number.
Field: 24h*
Field Title: EPSDT Family Planning
Instructions: When billing electronically, use “Y.” When billing on paper, use “1.”
Provider Information
Field: 24a shaded area
Field Title: NDC
Instructions: Enter the qualifier, N4, followed by the NDC (NDC should not have punctuation, dashes or spaces), units qualifier and units as described by the qualifier
Field: 24i shaded**
Field Title: ID Qualifier
Instructions: ZZ for the Taxonomy qualifier.
Field: 24j shaded**
Field Title: Taxonomy Code
Instructions: Enter the Taxonomy code for the rendering provider.
Field: 24j **
Field Title: NPI, Rendering Prov
Instructions: Enter NPI Number for the rendering provider.
Field: 31*
Field Title: Signature and Date
Instructions: Enter Signature and Date.
Field: 33*
Field Title: Billing Provider Info
Instructions: Enter Physical Address with a 9 digit ZIP code and phone number.
Field: 33a*
Field Title: NPI #
Instructions: Enter NPI number for billing/pay-to provider.
Field: 33b*
Field Title: Taxonomy #
Instructions: Enter the qualifier (ZZ) and the billing provider's taxonomy code.
Billing Information
Field: 21.1 - 21.4*
Field Title: Diagnosis codes Enter at least one diagnosis.
Field: 24a*
Field Title: Date(s) of Service
Instructions: Enter the dates of service include beginning and ending date even if same.
Field: 24b*
Field Title: Place of Service
Instructions: Enter the code for place of service.
Field: 24c**
Field Title: EMG
Instructions: Emergency Indicator if applicable.
Field: 24d*
Field Title: Procedure Code
Instructions: Enter the procedure code used. Enter modifiers if applicable.
Field: 24e*
Field Title: Diagnosis Pointer
Instructions: Enter the corresponding diagnosis pointer (1,2,3,or 4) that refers to the codes in field 21
Field: 24f*
Field Title: Charges
Instructions: Enter the total charge for this line
Field: 24g*
Field Title: Days/Units
Instructions: Enter the days or units used for the procedure.
Field: 28*
Field Title: Total Charges
Instructions: Enter total charges from all line items.
*Required Field **Required if applicable
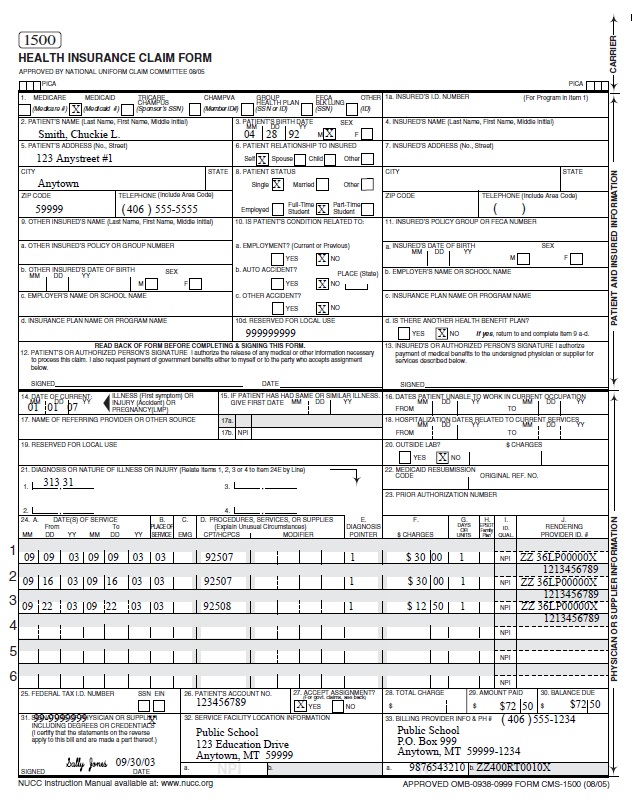
CMS-1500 Agreement
Your signature on the CMS-1500 constitutes your agreement to the terms presented on the back of the form. This form is subject to change by the Centers for Medicare and Montana Healthcare Programs Services (CMS).
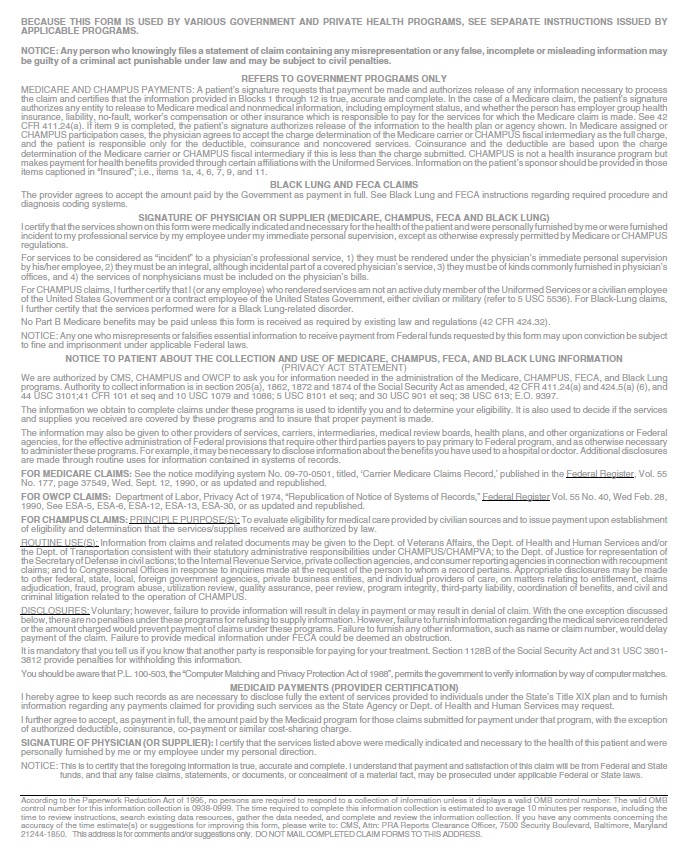
Avoiding Claim Errors
Claims are often denied or even returned to the provider before they can be processed. To avoid denials and returns, double-check each claim to confirm the following items are accurate. For more information on returned and denied claims, see the Billing Procedures chapter in this manual.
Common Claim Errors
Claim Error: Required field is blank
Prevention: Check the claim instructions earlier in this chapter for required fields (indicated by * or **). If a required field is blank, the claim may either be returned or denied.
Claim Error: Member ID number missing or invalid
Prevention: This is a required field (field 10d); verify that the member’s Montana Healthcare Programs ID number is listed as it appears on the member’s ID card.
Claim Error: Member name missing
Prevention: This is a required field (field 2); check that it is correct.
Claim Error: Provider NPI missing or invalid
Prevention: The provider NPI is a 10-digit number assigned to the provider by the National Plan and Provider Enumeration System. Verify the correct provider NPI is on the claim.
Claim Error: Prior authorization number missing
Prevention: When prior authorization (PA) is required for a service, the PA number must be listed on the claim in field 23. (See the Prior Authorization chapter in this manual.)
Claim Error: Not enough information regarding other coverage
Prevention: Fields 1a and 11d are required fields when a member has other coverage. (Refer to the examples earlier in this chapter.)
Claim Error: Authorized signature missing
Prevention: Each claim must have an authorized signature belonging to the provider, billing clerk, or office personnel. The signature may be typed, stamped, or hand-written.
Claim Error: Signature date missing
Prevention: Each claim must have a signature date. Incorrect claim form used Services covered in this manual require a CMS-1500 claim form (or electronic Professional claim).
Claim Error: Information on claim form not legible
Prevention: Information on the claim form must be legible. Use dark ink and center the information in the field. Information must not be obscured by lines.
Claim Error: Medicare EOMB not attached
Prevention: When Medicare is involved in payment on a claim, the Medicare EOMB must be attached to the claim or it will be denied.
Other Programs
This chapter also applies to claims forms completed for MHSP services and Healthy Montana Kids (HMK) eyeglass services.
End of Submitting a Claim Chapter
Remittance Advices and Adjustments
The Remittance Advice
The Remittance Advice (RA) is the best tool providers have to determine the status of a claim. RAs accompany payment for services rendered. The RA provides details of all transactions that have occurred during the previous RA cycle. Each line of the RA represents all or part of a claim, and explains whether the claim or service has been paid, denied, or suspended (also referred to as pending).
The pending claims section of the RA is informational only. Do not take any action on claims displayed here.
If the claim was suspended or denied, the RA also shows the reason.
To access the MATH web portal, you must first complete a Provider Enrollment Form and an Trading Partner Agreement (see the following table). To receive an electronic RA, the provider must complete a Trading Partner Agreement and register for the Montana Access to Health (MATH) web portal. You can access your electronic RA through the MATH web portal by going to the Provider Information website and selecting Log in to Montana Access to Health.
After these forms have been processed, you will receive a user ID and password that you can use to log on to the web portal. The verification process also requires a provider ID, a submitter ID, and a tax ID number. Each provider must complete an EDI Trading Partner Agreement, but if there are several providers in one location who are under one tax ID number, they can use one submitter number. These providers should enter the submitter ID in both the provider number and submitter ID fields. Otherwise, enter the provider number in the provider number field.
If a claim was denied, read the description of the EOB before taking any action on the claim.
RAs are available in PDF format. You can read, print, or download PDF files using Adobe Acrobat Reader, which is available on the Provider Information website. Due to space limitations, each RA is only available for 90 days.
Electronic RAs are available for only 90 days on the web portal.
The RA is divided into the following sections:
Sections of the Paper RA
Section: RA Notice
Description: The RA Notice is on the first page of the remittance advice. This section contains important messages about rate changes, revised billing procedures, and many other items that may affect providers and claims.
Section: Paid Claims
Description: This section shows claims paid during the previous cycle. It is the provider’s responsibility to verify that claims were paid correctly. If Montana Healthcare Programs overpays a claim and the problem is not corrected, it may result in an audit requiring the provider to return the overpayment plus interest. If a claim was paid at the wrong amount or with incorrect information, the claim must be adjusted. (See Adjustments later in this chapter.)
Section: Denied Claims
Description: This section shows claims denied during the previous cycle. If a claim has been denied, refer to the Reason/Remark column (Field 18). The Reason and Remark Code Description located at the end of the RA explains why the claim was denied. See the section titled The Most Common Billing Errors and How to Avoid Them in the Billing Procedures chapter.
Section: Pending Claims
Description: All claims that have not reached final disposition will appear in this area of the paper RA (pended claims are not available on X12N 835 transactions). The RA uses suspended and pending interchangeably. They both mean that the claim has not reached final disposition. If a claim is pending, refer to the Reason/Remark Code section (Field 18) located at the end of the RA will explain why the claim is suspended. This section is informational only. Do not take any action on claims displayed here. Processing will continue until each claim is paid or denied.
Claims shown as pending with Reason Code 133 require additional review before a decision to pay or deny is made. If a claim is being held while waiting for member eligibility information, it may be suspended for a maximum of 30 days. If Montana Healthcare Programs receives eligibility information within the 30-day period, the claim will continue processing. If no eligibility information is received within 30 days, the claim will be denied. When a claim is denied for lack of eligibility, the provider should verify that the correct Montana Healthcare Programs ID number was billed. If the ID number was incorrect, resubmit the claim with the correct ID number.
Section: Credit Balance Claims
Description: Credit balance claims are shown here until the credit has been satisfied.
Section: Gross Adjustments
Description: Any gross adjustments performed during the previous cycle are shown here.
Section: Reason and Remark Code Description
Description: This section lists the reason and remark codes that appear throughout the RA with a brief description of each.
Sample Remittance Notice
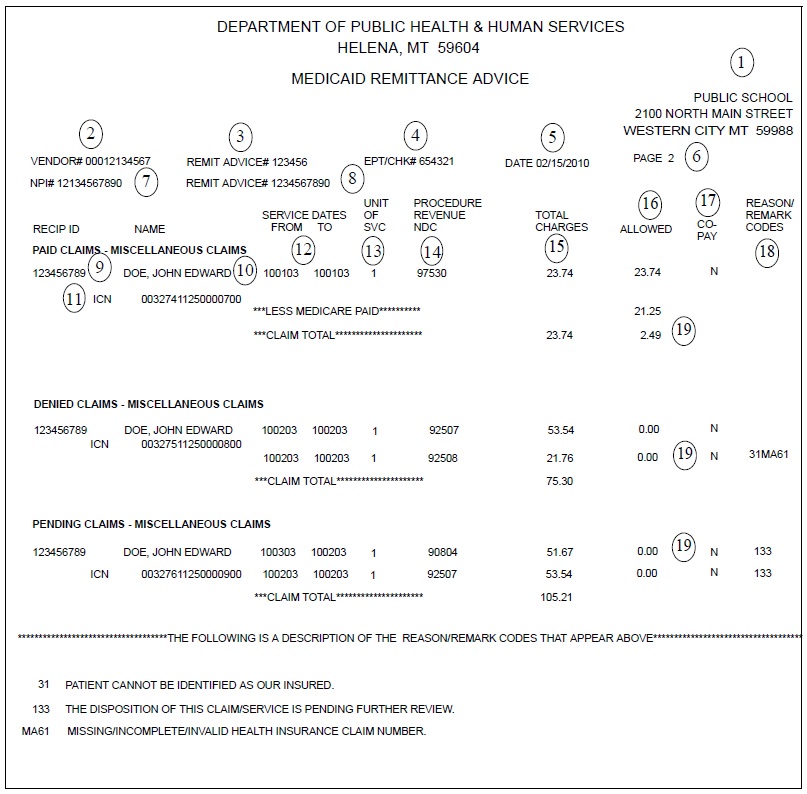
Key Fields on the Remittance Advice
Field: 1. Provider name and address
Description: Provider’s business name and address as recorded with the Department.
Field: 2. Vendor #
Description: The 7-digit number assigned to the provider.
Field: 3. Remittance advice number
Description: The remittance advice number.
Field: 4. EFT/Check number
Description: The EFT or check number of payment
Field: 5. Date
Description: The date the RA was issued.
Field: 6. Page number
Description: The page number of the RA.
Field: 7. NPI
Description: A unique 10-digit identification number required by HIPAA for all U.S. health care providers. Providers must use their NPI to identify themselves in all HIPAA transactions.
Field: 8. Taxonomy
Description: Alphanumeric code that indicates the provider’s specialty.
Field: 9. Member ID
Description: The member’s Montana Healthcare Programs ID number.
Field: 10. Name
Description: The member’s name.
Field: 11. Internal control number (ICN)
Description: Each claim is assigned a unique 17-digit number (ICN). Use this number when you have any questions concerning your claim. The claim number represents the following information:
0 00111 11 123 000123
A B C D E
A = Claim medium
0 = Paper claim
2 = Electronic claim
3 = Encounter claim
4 = System generated claim (mass adjustment, nursing home turn-around
document, or point-of-sale (POS) pharmacy claim)
6 = Pharmacy
B = Julian date (e.g. April 20, 2000 was the 111th day of 2000)
C = Microfilm number
00 = Electronic claim
11 = Paper claim
D = Batch number
E = Claim number
If the first number is:
0 = Regular claim
1 = Negative side adjustment claim (Montana Healthcare Programs recovers payment)
2 = Positive side adjustment claim (Montana Healthcare Programs reprocesses)
Field: 12. Service dates
Description: Dates services were provided. If services were performed in a single day, the same date will appear in both columns.
Field: 13. Unit of service
Description: The units of service rendered under this procedure or NDC code.
Field: 14. Procedure/Revenue/NDC
Description: The procedure code (CPT or HCPCS), National Drug Code (NDC), or revenue code will appear in this column. If a modifier was used, it will also appear in this column.
Field: 15. Total charges
Description: The amount a provider billed for this service.
Field: 16. Allowed
Description: The Montana Healthcare Programs allowed amount.
Field: 18. Reason and remark codes
Description: A code which explains why the specific service was denied or pended. Descriptions of these codes are listed at the end of the RA.
Field: 19. Deductions, billed amount, and paid amount
Description: Any deductions, such as third-party liability are listed first. The amount the provider billed is next, followed by the amount of Montana Healthcare Programs reimbursement.
Credit Balances
Credit balances occur when claim adjustments reduce original payments causing the provider to owe money to the Department. These claims are considered in process and continue to appear on the RA until the credit has been satisfied.
The credit balance section is informational only. Do not post from credit balance statements.
Credit balances can be resolved in two ways:
- By working off the credit balance. Remaining credit balances can be deducted from future claims. These claims will continue to appear on consecutive RAs until the credit has been paid.
- By sending a check payable to DPHHS for the amount owed. This method is required for providers who no longer submit claims to Montana Healthcare Programs. Attach a note stating that the check is to pay off a credit balance and include your NPI. Send the check to the attention of the Third-Party Liability Unit at the address in Key Contacts.
Rebilling and Adjustments
Rebillings and adjustments are important steps in correcting any billing problems you may experience. Knowing when to use the rebilling process versus the adjustment process is important.
Montana Healthcare Programs does not accept any claim for resubmission or adjustment after 12 months from the date of service (see Timely Filing Limits in Billing Procedures chapter).
How Long Do I Have to Rebill or Adjust a Claim?
- Providers may resubmit or adjust any initial claim within the timely filing limits described in the Billings Procedure chapter of this manual.
- These time periods do not apply to overpayments that the provider must refund to the Department. After the 12-month time period, a provider may not refund overpayments to the Department by completing a claim adjustment. The provider may refund overpayments by issuing a check or asking the TPL unit to complete a gross adjustment.
Rebilling Montana Healthcare Programs
Rebilling is when a provider submits a claim to Montana Healthcare Programs that was previously submitted for payment but was either returned or denied. Claims are often returned to the provider before processing because key information such as NPI and taxonomy or authorized signature and date are missing or unreadable. For tips on preventing returned or denied claims, see the Billing Procedures and Submitting a Claim chapters.
When to Rebill Montana Healthcare Programs
- Claim Denied. Providers can rebill Montana Healthcare Programs when a claim is denied in full, as long as the claim was denied for reasons that can be corrected. When the entire claim is denied, check the Reason and Remark Code/Description, make the appropriate corrections, and resubmit the claim (not an adjustment).
Rebill denied claims only after appropriate corrections have been made.
- Line Denied. When an individual line is denied on a multiple-line claim, correct any errors and rebill Montana Healthcare Programs. Do not use an adjustment form.
- Claim Returned. Rebill Montana Healthcare Programs when the claim is returned under separate cover. Occasionally, Montana Healthcare Programs is unable to process the claim and will return it to the provider with a letter stating that additional information is needed to process the claim. Correct the information as directed and resubmit your claim.
How to Rebill
- Check any Reason and Remark Code listed and make your corrections on a copy of the claim, or produce a new claim with the correct information.
- When making corrections on a copy of the claim, remember to cross out or omit all lines that have already been paid. The claim must be neat and legible for processing.
- Enter any insurance (TPL) information on the corrected claim, or include insurance denial information, and submit to Montana Healthcare Programs.
Adjustments
If a provider believes that a claim has been paid incorrectly, the provider may call Provider Relations or submit a claim inquiry for review. (See the Billing Procedures chapter, Claim Inquiries.) Once an incorrect payment has been verified, the provider may submit an Individual Adjustment Request to Provider Relations. If incorrect payment was the result of a Conduent keying error, contact Provider Relations.
When adjustments are made to previously paid claims, the Department recovers the original payment and issues appropriate repayment. The result of the adjustment appears on the provider’s RA as two transactions. The original payment will appear as a credit transaction. The replacement claim reflecting the corrections will be listed as a separate transaction and may or may not appear on the same RA as the credit transaction. The replacement transaction will have nearly the same ICN number as the credit transaction, except the 12th digit will be a 2, indicating an adjustment. See Key Fields on the Remittance Advice earlier in this chapter. Adjustments are processed in the same time frame as claims.
Adjustments can only be made to paid claims.
When to request an adjustment
- Request an adjustment when a claim was overpaid or underpaid.
- Request an adjustment when a claim was paid but the information on the claim was incorrect (e.g., member ID, provider NPI, date of service, procedure code, diagnoses, units).
How to Request an Adjustment
To request an adjustment, use the Individual Adjustment Request form. The requirements for adjusting a claim are as follows:
- Claims Processing must receive individual claim adjustment requests within 12 months from the date of service (see Timely Filing Limits in the Billing Procedures chapter).After this time, gross adjustments are required (see Definitions).
- Use a separate adjustment request form for each ICN.
- If you are correcting more than one error per ICN, use only one adjustment request form, and include each error on the form.
- If more than one line of the claim needs to be adjusted, indicate which lines and items need to be adjusted in the Remarks section of the adjustment form.
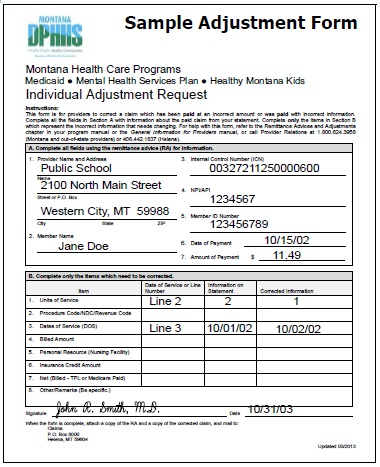
Completing an Adjustment Request Form
- Download the Individual Adjustment Request from the Provider Information website. (See Key Websites.) Complete Section A with provider and member information and the claim’s ICN number.
- Complete Section B with information about the claim. Fill in only the items that need to be corrected:
- Enter the date of service or the line number in the Date of Service or Line Number column.
- Enter the information from the claim that was incorrect in the Information on Statement column.
- Enter the correct information in the Corrected Information column.
- Attach copies of the RA and a corrected claim if necessary.
- If the original claim was billed electronically, a copy of the RA will suffice.
- If the RA is electronic, attach a screen print of the RA.
- Verify the adjustment request has been signed and dated.
- Send the adjustment request to Claims Processing. (See Key Contacts.)
- If an original payment was an underpayment by Montana Healthcare Programs, the adjustment will result in the provider receiving the additional payment amount allowed.
- If an original payment was an overpayment by Montana Healthcare Programs, the adjustment will result in recovery of the overpaid amount through a credit. If the result is a credit balance, it can be worked off or the provider can pay off the balance by check. (See Credit Balances earlier in this chapter.)
- Any questions regarding claims or adjustments must be directed to Provider Relations. (See Key Contacts.)
Completing an Individual Adjustment Request Form
Section A
Field: 1. Provider name and address
Description: Provider’s name and address (and mailing address if different).
Field: 2. Member name
Description: The member’s name is here.
Field: 3.* Internal control number (ICN)
Description: There can be only one ICN per adjustment request form. When adjusting a claim that has been previously adjusted, use the ICN of the most recent claim.
Field: 4.* Provider NPI
Description: The provider’s NPI.
Field: 5.* Member Montana Healthcare Programs number
Description: Member’s Montana Healthcare Programs ID number.
Field: 6. Date of payment
Description: Date claim was paid is found on remittance advice field 5 (see the sample RA earlier in this chapter).
Field: 7. Amount of payment
Description: The amount of payment from the remittance advice field 17 (see the sample RA earlier in this chapter.).
Section B
Field: 1. Units of service
Description: If a payment error was caused by an incorrect number of units, complete this line.
Field: 2. Procedure code/NDC/Revenue code
Description: If the procedure code, NDC, or revenue code is incorrect, complete this line.
Field: 3. Dates of service (DOS)
Description: If the date of service is incorrect, complete this line.
Field: 4. Billed amount
Description: If the billed amount is incorrect, complete this line.
Field: 5. Personal resource (nursing facility)
Description: If the member’s personal resource amount is incorrect, complete this line.
Field: 6. Insurance credit amount
Description: If the member’s insurance credit amount is incorrect, complete this line.
Field: 7. Net (Billed – TPL or Medicare paid)
Description: If the payment error was caused by a missing or incorrect insurance credit, complete this line. Net is billed amount minus the amount third party liability or Medicare paid.
Field: 8. Other/Remarks
Description: If none of the above items apply, or if you are unsure what caused the payment error, complete this line.
*Indicates a required field.
Mass Adjustments
Mass adjustments are done when it is necessary to reprocess multiple claims.
They generally occur when:
- Montana Healthcare Programs has a change of policy or fees that is retroactive. In this case federal laws require claims affected by the changes to be mass adjusted.
- A system error that affected claims processing is identified.
Providers are informed of mass adjustments on the first page of the RA in the RA Notice section. Mass adjustment claims shown on the RA have an ICN that begins with a 4. (See Key Fields on the Remittance Advice earlier in this chapter.)
Electronic RAs are available for only 90 days on the web portal.
Payment and the RA
Providers receive their Montana Healthcare Programs payment and remittance advice weekly. Payment can be via check or electronic funds transfer (EFT). Direct deposit is another name for EFT.
With EFT, the Department deposits the funds directly to the provider’s bank account. If the scheduled deposit day is a holiday, funds will be available on the next business day. This process does not affect the delivery of the remittance advice that providers currently receive with payments. RAs will continue to be mailed to providers unless they specifically request an electronic RA.
To participate in EFT, providers must complete a Direct Deposit Sign-Up Form (Standard Form 1199A). One form must be completed for each provider NPI. See the following table, Required Forms for EFT and/or Electronic RA.
Once electronic transfer testing shows payment to the provider’s account, all Montana Healthcare Programs payments will be made through EFT. See Direct Deposit Arrangements under Key Contacts for questions or changes regarding EFT.
Required Forms for EFT and/or Electronic RA
Form:
- EDI Provider Enrollment Form
- EDI Trading Partner Agreement
Purpose:
Allows providers to access their RAs on the Montana Access to Health (MATH) web portal.
Must also include:
- EDI Provider Enrollment Form
- EDI Trading Partner Agreement
Where to Get:
- Provider Information website
- Provider Relations (See Key Contacts.)
Where to Send:
Fax to number on form.
Form:
- Direct Deposit Sign-Up Form (Standard Form 1199A)
Purpose:
Allows the Department to automatically deposit Montana Healthcare Programs payment into provider’s bank account
Where to Get:
- Provider Information website (Forms)
- Provider’s bank Provider Relations (See Key Contacts.)
End of Remittance Advices and Adjustments Chapter
How Payment Is Calculated
Overview
Though providers do not need the information in this chapter in order to submit claims to the Department, the information allows providers to understand how payment is calculated and to predict approximate payment for particular claims. The payment methods described do not apply to services provided under Healthy Montana Kids (HMK)/Children’s Health Insurance Program (CHIP).
Payment for School-Based Services
Federal regulations specify that one government entity may not bill another government entity more than their cost (OMB A-87). The following describes payment methods for various services that can be provided in the school setting. Payment for these services is limited to the lower of the calculated fee or the billed amount.
Speech, Occupational and Physical Therapy Services
Speech and language therapy services, occupational therapy services and physical therapy services are paid by the Resource Based Relative Value Scale (RBRVS) method of reimbursement. As noted above, only the federal portion will be paid. For more detail on the RBRVS system, see the How Payment Is Calculated chapter of the Physician-Related Services provider manual, which is available on the Provider Information website. (See Key Websites.)
Each RBRVS fee is the product of a relative value times a conversion factor. This total is always multiplied by the current Federal Matching Assistance Percentage (FMAP).
The Department publishes relative weights, the current conversion factor, and the current FMAP figure. The conversion factor is determined by the Department and set at a level intended to achieve legislatively set budget targets.
Private Duty Nursing
The only code available for this service is T1000. Payment for this code is based on the Montana Healthcare Programs fee schedule, and is calculated as follows:
Fee x number of 15-minute units = payment
The current FMAP is then calculated against this total for final reimbursement
School Psychologist
Both codes available for billing school psychologist services are paid by the RBRVS method.
Each RBRVS fee is the product of a relative value times a conversion factor. This total is always multiplied by the current FMAP for a total reimbursement.
The Department publishes relative weights, the current conversion factor, and the current FMAP figure. The conversion factor is determined by the Department and set at a level intended to achieve legislatively set budget targets.
Personal Care Paraprofessionals
The only code available for this service is T1019. Payment for this code is based on the Montana Healthcare Programs fee schedule, and is calculated as follows:
Fee x number of 15-minute units = payment
The current FMAP is then calculated against this total for final reimbursement.
How Payment Is Calculated on TPL Claims
When a member has coverage from both Montana Healthcare Programs and another insurance company, the other insurance company is referred to as Third Party Liability (TPL). In these cases, the other insurance is the primary payer (as described in the Coordination of Benefits chapter of this manual), and Montana Healthcare Programs makes a payment as the secondary payer. Montana Healthcare Programs will make a payment only when the TPL payment is less than the Montana Healthcare Programs allowed amount.
How Payment Is Calculated on Medicare Crossover Claims
When a member has coverage from both Medicare and Montana Healthcare Programs, Medicare is the primary payer. Montana Healthcare Programs will pay the coinsurance and deductible amounts for these dually eligible individuals. See the How Payment is Calculated chapter in the Physician-Related Services manual for examples on how payment is calculated on Medicare crossover claims.
End of How Payment is Calculated Chapter
Appendix A: Forms
- Individual Adjustment Request
- Audit Preparation Checklist
- Request for Private Duty Nursing Services
- Paperwork Attachment Cover Sheet
End of Appendix A: Forms Chapter
Appendix B: Personal Care Paraprofessional Services Documentation
Personal Care Paraprofessional Services Provided in Schools – Child Profile
Purpose
The Child Profile is intended to:
- To provide an instrument for collecting and documenting essential information needed to establish the Montana Healthcare Programs child’s functional limitations and ability to perform activities of daily living.
- To document information on service planning issues for personal care services.
- To provide a worksheet for determining the daily units per week needed by the child.
Procedure
The Profile must be completed by the Individualized Education Plan (IEP) team at the initial meeting for services, at the annual review, and whenever a significant change in the child’s condition occurs causing the service need to change.
Instructions
- Child Name: Enter the child's full name.
- Child ID: Enter child's Montana Healthcare Programs ID number.
- DOB: Child’s date of birth.
- Date Span: The time period the child will receive personal care services, up to one year.
- Level of Impairment: Rate the child's impairment level according to the following scale for each task listed:
0 = Independent: No functional impairment. The child is able to conduct the activities without difficulty and has no need for assistance. Need is met with adaptive equipment or service animal.
1 = Standby/Cuing: Mild functional impairment. The child is able to conduct the activity but does require standby assist or cuing.
2 = Limited Assist: Moderate functional impairment. The child is able to conduct the activity with moderate difficulty and requires minimal assistance.
3 = Extensive Assist: Severe functional impairment. The child has considerable difficulty completing the activity and requires extensive assistance.
4 = Total Dependence: Total functional impairment. The child is completely unable to carry out any part of the activity.
An IEP team member must decide which of the five impairment levels best describes the child reviewed. An impairment in this context is a functional limitation (i.e., a limitation in the ability to carry out an activity or function). A member is considered to have an impairment with respect to a particular activity if he/she is limited, either physically or mentally, in his/her ability to carry out that activity.
The “0” and “4” rating is absolute in the sense that they indicate no functional impairment or total dependency. For example, if a child can perform any of the dressing tasks for themselves, a “4” is not appropriate. If he/she can perform the dressing task without difficulty, a “0” is appropriate.
If a child is able to conduct an activity only with difficulty, and the difficulty is such that the child frequently cannot complete some part of the activity, then the child is impaired, even if the child at other times can complete the entire activity. In addition, if the degree of difficulty is such that the child should have at least minimal assistance with that activity, then the child is impaired, even if the child can (with difficulty) conduct the activity without assistance. If the child can complete the activity but needs cuing to do so, or, because of safety considerations needs someone there while completing the task, they would require standby assistance. If the difficulty with an activity does not affect the child's conduct of the activity or does not cause any problems for the child, the child is not impaired.
Enter a Level for Each Task
The Personal Care Paraprofessional Services Profile is designed to rate a child's capacity for self-care. Determine the level for each task according to the capacity for self-care and not according to the child's access to a resource to assist with the task. In rating each item, use the child's response, your own observations of activity, and any knowledge provided about the child from other sources. To determine the severity of the child's impairment, consider the following factors:
- Child Perception of the Impairment: Does the child view the impairment as a major or minor problem?
- Congruence: Is the child's response to a particular question consistent with the child's response to other questions and, also, consistent with what you have observed?
- Child History: Probe for an understanding of the child's history as it relates to the current situation and of the child's attitude about the severity of the impairment. How has the impairment changed the child's lifestyle?
- Adaptation: If the child has adapted his physical environment or clothing to the extent that he is able to function without assistance, the degree of impairment will be lessened, but the child will still have an impairment. This includes the use of adaptive equipment.
Use the following examples for each item to help you differentiate between scores of 2 or 3.
ADL: Grooming
2 = Limited Assist: Child may set out supplies. Child may accomplish tasks an adaptive device for assistance.
3 = Extensive: Child needs to have help with shaving or shampooing, etc., because of inability to see well, to reach, or to successfully use equipment. Child needs someone to put lotion on body or to comb or brush hair.
ADL: Toileting
2 = Limited Assist: Child has instances of urinary incontinence, and needs help because of this from time to time. Fecal incontinence does not occur unless child has a specific illness episode. Child may have catheter or colostomy bag, and occasionally needs assistance with management.
3 = Extensive: Child often is unable to get to the bathroom on time to urinate. Child has occasional episodes of fecal incontinence. Child may wear diapers to manage the problem and needs some assistance with them. Child usually needs assistance with catheter or colostomy bag.
ADL: Dressing
2 = Limited Assist: Child needs occasional help with zippers, buttons, or putting on shoes and socks. Child may need help laying out and selecting clothes.
3 = Extensive: Child needs help with zippers, buttons, or shoes and socks. Child needs help getting into garments, including putting arms in sleeves, legs in pants, or pulling up pants. Child may dress totally inappropriately without help or would not finish dressing without physical assistance.
ADL: Transferring
2 = Limited Assist: Child usually can get out of bed or chair with minimal assistance.
3 = Extensive: Child needs hands-on assistance when rising to a standing position or moving into a wheelchair to prevent losing balance or falling. Child is able to help with the transfer by holding on, pivoting, and/or supporting himself.
ADL: Ambulation
2 = Limited Assist: Child walks alone without assistance for only short distances. Child can walk with minimal difficulty using an assistive device or by holding onto walls or furniture.
3 = Extensive: Child has considerable difficulty walking even with an assistive device. Child can walk only with assistance from another person. Child never walks alone outdoors without assistance. Child may use a wheelchair periodically.
ADL: Eating
2 = Limited Assist: Child may need occasional physical help. Child eats with adaptive devices but requires help with their positioning.
3 = Extensive: Child usually needs extensive hands-on assistance with eating. Child may hold eating utensils but needs continuous assistance during meals. Child would not complete meal without continual help. Spoon-feeding of most foods is required, but child can eat some finger foods.
ADL: Exercise
2 = Limited Assist: Child may need occasional assistance in completing exercise routine. Child may need occasional support or guidance.
3 = Extensive: Child needs some assistance in completing exercise routine. Child needs support or guidance.
ADL: Bus Escort
2 = Limited Assist: Child requires minimal assistance on bus en route to or from school. Child does not have family or caregiver to assist. Child receives a medical service at school on this date.
3 = Extensive: Child requires assistance on bus en route to or from school. Child does not have family or caregiver to assist. Child receives a medical service at school on this date.
Check the appropriate column that indicates the degree to which the child's need for help in the completion of each task is met. Check one column for each task:
M = Met: The child's needs are met. The child may be independent in this task or someone other than the Personal Care Paraprofessional is meeting the child’s need for help. Other sources for meeting the need include family or friends. No time can be authorized for any task coded with an “M”.
P = Partially Met: The child requires help with the task. Someone other than the personal care paraprofessional is providing that help part of the time, or the child may participate
in the task.
U = Unmet: The child requires help with the task and the need is currently unmet.
- Notes: Enter any appropriate notes.
- Minutes Per Day: For each task to be provided, enter the daily number of minutes needed to conduct that task.
- Days Per Week: For each task to be provided, enter the number of days per week the child will require assistance with the task.
- Total Minutes: Multiply the minutes per day times the days per week to obtain the total minutes per week for each task.
The amount of time allowed for any particular task should be determined by taking into account:
- The amount of assistance the child will usually need.
- Which specific activities need to be accomplished.
- Environmental/housing factors that may hinder (or facilitate) service delivery.
- Child’s unique circumstances.
Personal Care Paraprofessional Services Provided In Schools Child Profile - Form
Task/Hour Guide Instructions
Purpose
The purpose of this form is to record the amount of time that is spent providing Personal Care services. This form is a sample and can be recreated by district personnel to meet specific needs.
Specific Tasks
Each task has one or more activities or sub-tasks that forms the overall task. When calculating time, carefully consider which activities were provided.
- Dressing:
- Dressing member
- Undressing member
- Cuing assistance
- Exercise:
- Range of motion
- Grooming:
- Brushing teeth
- Laying out supplies
- Combing/brushing hair
- Applying nonprescription lotion to skin
- Washing hands and face
- Cuing assistance
- Toileting:
- Changing diapers
- Changing colostomy bag/emptying catheter bag
- Assisting on/off bed pan
- Assisting with use of urinal
- Assisting with feminine hygiene needs
- Assisting with clothing during toileting
- Assisting with toilet hygiene; includes use of toilet paper & washing hands
- Set-up supplies and equipment (Does NOT include preparing catheter equipment)
- Standby assistance
- Transfer:
- Non-ambulatory movement from one stationary position to another (transfer)
- Adjusting/changing member’s position in bed or chair (positioning)
- Ambulation (Walking):
- Assisting child in rising from a sitting to a standing position and/or position for use of walking apparatus
- Assisting with putting on and removing leg braces and prostheses for ambulation
- Assisting with ambulation/using steps
- Standby assistance with ambulation
- Assistance with wheelchair ambulation
NOTE: Do not include exercise as ambulation.
- Eating:
- Spoon feeding
- Bottle feeding
- Set up of utensils/adaptive devices
- Assistance with using eating or drinking utensils/adaptive devices
- Cutting up foods
- Standby assistance/encouragement
NOTE: Tube feeding is not an allowable service.
- Bus Escort:
- Accompanying a child on the bus when the child is functionally limited and receives medical service at the school on that date. Not for purposes of behavioral management.
End of Appendix B: Personal Care Paraprofessional Services Documentation Chapter
Definitions and Acronyms
This section contains definitions, abbreviations, and acronyms used in this manual.
270/271 Transactions
The ASC X12N eligibility inquiry (270) and response (271) transactions.
276/277 Transactions
The ASC X12N claim status request (276) and response (277) transactions.
278 Transactions
The ASC X12N request for services review and response used for prior authorization.
835 Transactions
The ASC X12N payment and remittance advice (explanation of benefits) transaction.
837 Transactions
The ASC X12N professional, institutional, and dental claim transactions (each with its own separate Implementation Guide).
Accredited Standards Committee X12, Insurance Subcommittee (ASC X12N)
The ANSI-accredited standards development organization, and one of the six Designated Standards Maintenance Organizations (DSMO), that created and is tasked with maintaining the administrative and financial transactions standards adopted under HIPAA for all health plans, clearinghouses, and providers who use electronic transactions.
Administrative Rules of Montana (ARM)
The rules published by the executive departments and agencies of the state government.
Allowed Amount
The maximum amount reimbursed to a provider for a health care service as determined by Montana Healthcare Programs/MHSP/HMK or another payer. Other cost factors, (such as TPL, or incurment) are often deducted from the allowed amount before final payment. Montana Healthcare Programs’ allowed amount for each covered service is listed on the Department fee schedule.
Ancillary Provider
Any provider that is subordinate to the member’s primary provider, or providing services in the facility or institution that has accepted the member as a Montana Healthcare Programs member.
Assignment of Benefits
A voluntary decision by the member to have insurance benefits paid directly to the provider rather than to the member. The act requires the signing of a form for the purpose. The provider is not obligated to accept an assignment of benefits. However, the provider may require assignment in order to protect the provider’s revenue.
Authorization
An official approval for action taken for, or on behalf of, a Montana Healthcare Programs member. This approval is only valid if the member is eligible on the date of service.
Basic Montana Healthcare Programs
members with Basic Montana Healthcare Programs have limited Montana Healthcare Programs services. See the Montana Healthcare Programs Covered Services chapter General Information for Providers manual.
Bundled
Items or services that are deemed integral to performing a procedure or visit are not paid separately in the APC system. They are packaged (also called bundled) into the payment for the procedure or visit. Medicare developed the relative weights for surgical, medical, and other types of visits so that the weights reflect the packaging rules used in the APC method. Items or services that are packaged receive a status code of “N”.
Cash Option
Cash option allows the member to pay a monthly premium to Montana Healthcare Programs and have Montana Healthcare Programs coverage for the entire month rather than a partial month.
Centers for Medicare and Medicaid Services (CMS)
Administers the Medicare program and oversees the state Montana Healthcare Programs.
Children’s Health Insurance Program (CHIP)
The Montana plan is now known as Healthy Montana Kids (HMK).
Children’s Special Health Services (CSHS)
CSHS assists children with special health care needs who are not eligible for Montana Healthcare Programs by paying medical costs, finding resources, and conducting clinics.
Clean Claim
A claim that can be processed without additional information from or action by the provider of the service.
Code of Federal Regulations (CFR)
Rules published by executive departments and agencies of the federal government.
Coinsurance
The member’s financial responsibility for a medical bill as assigned by Montana Healthcare Programs or Medicare (usually a percentage). Montana Healthcare Programs coinsurance is usually 5% of the Montana Healthcare Programs allowed amount, and Medicare coinsurance is usually 20% of the Medicare allowed amount.
Conversion Factor
A state specific dollar amount that converts relative values into an actual fee. This calculation allows each payer to adopt the RBRVS to its own economy.
Copayment
The member’s financial responsibility for a medical bill as assigned by Montana Healthcare Programs (usually a flat fee).
Cosmetic
Serving to modify or improve the appearance of a physical feature, defect, or irregularity.
CPT
Physicians’ Current Procedural Terminology contains procedure codes which are used by medical practitioners in billing for services rendered. The book is published by the American Medical Association.
Credit Balance Claims
Adjusted claims that reduce original payments, causing the provider to owe money to the Department. These claims are considered in process and continue to appear on the remittance advice until the credit has been satisfied.
Crossovers
Claims for members who have both Medicare and Montana Healthcare Programs. These claims may come electronically from Medicare or directly from the provider.
DPHHS, State Agency
The Montana Department of Public Health and Human Services (DPHHS or the Department) is the designated State Agency that administers the Montana Healthcare Program. The Department's legal authority is contained in Title 53, Chapter 6 MCA. At the federal level, the legal basis for the program is contained in Title XIX of the Social Security Act and Title 42 of the Code of Federal Regulations (CFR). The program is administered in accordance with the Administrative Rules of Montana (ARM), Title 37, Chapter 86.
Dual Eligibles
Members who are covered by Medicare and Montana Healthcare Programs.
Early and Periodic Screening, Diagnosis, and Treatment (EPSDT)
This program provides Montana Healthcare Programs-covered children with comprehensive health screenings, diagnostic services, and treatment of health problems.
Electronic Funds Transfer (EFT)
Payment of medical claims that are deposited directly to the provider’s bank account.
Emergency Services
A service is reimbursed as an emergency if one of the following criteria is met:
- The service is billed with CPT Code 99284 or 99285
- The member has a qualifying emergency diagnosis code. A list of emergency diagnosis codes is available on the Provider Information website.
- The services did not meet one of the previous two requirements, but the hospital believes an emergency existed. In this case, the claim and documentation supporting the emergent nature of the service must be mailed to the emergency department review contractor.
Experimental
A noncovered item or service that researchers are studying to investigate how it affects health.
Explanation of Medicare Benefits (EOMB)
A notice sent to providers informing them of the services which have been paid by Medicare.
Fiscal Agent
Conduent State Healthcare, LLC, is the fiscal agent for the State of Montana and processes claims at the Department's direction and in accordance with ARM 37.86 et seq.
Full Montana Healthcare Programs
members with Full Montana Healthcare Programs have a full scope of Montana Healthcare Programs benefits. See the General Information for Providers manual, Montana Healthcare Programs Covered Services.
Gross Adjustment
A lump sum debit or credit that is not claim specific made to a provider.
HCPCS
Acronym for the Healthcare Common Procedure Coding System, and is pronounced “hickpicks.” There are two types of HCPCS codes:
- Level 1 includes the CPT codes.
- Level 2 includes the alphanumeric codes A–V which CMS maintains for a wide range of services from ambulance trips to hearing aids which are not addressed by CPT coding.
Health Improvement Program (HIP)
A service provided under the Passport to Health program for members who have one or more chronic health conditions. Care management focuses on helping members improve their health outcomes through education, help with social services, and coordination with the member's medical providers.
Health Insurance Portability and Accountability Act (HIPAA)
A federal plan designed to improve efficiency of the health care system by establishing standards for transmission, storage, and handling of data.
Healthy Montana Kids (HMK)
HMK offers low-cost or free health insurance for low-income children younger than 19. Children must be uninsured U.S. citizens or qualified aliens, Montana residents who are not eligible for Montana Healthcare Programs. DPHHS administers the program and purchases health insurance from Blue Cross and Blue Shield of Montana (BCBSMT). Benefits for dental services and eyeglasses are provided by DPHHS through the same contractor (Conduent State Healthcare, LLC) that handles Montana Healthcare Programs provider relations and claims processing.
International Classification of Disease (ICD)
The International Classification of Diseases contains the diagnosis codes used in coding claims and the procedure codes used in billing for services performed in a hospital setting.
Indian Health Service (IHS)
IHS provides health services to American Indians and Alaska Natives.
Individual Adjustment
A request for a correction to a specific paid claim.
Internal Control Number (ICN)
The unique number assigned to each claim transaction that is used for tracking.
Investigational
A noncovered item or service that researchers are studying to investigate how it affects health.
Mass Adjustment
Adjustments made to multiple claims at the same time. They generally occur when the Department has a change of policy or fees that is retroactive, or when a system error that affected claims processing is identified.
Member
An individual enrolled in a Department medical assistance program.
Medically Necessary
A term describing a requested service which is reasonably calculated to prevent, diagnose, correct, cure, alleviate or prevent worsening of conditions in the member. These conditions must be classified as one of the following: endanger life, cause suffering or pain, result in an illness or infirmity, threaten to cause or aggravate a handicap, or cause physical deformity or malfunction. There must be no other equally effective, more conservative, or substantially less costly course of treatment available or suitable for the member requesting the service. For the purpose of this definition, course of treatment may include mere observation or, when appropriate, no treatment at all.
Medicare
The federal health insurance program for certain aged or disabled members.
Mental Health Services Plan (MHSP)
This plan is for individuals who have a severe and disabling mental illness (SDMI), are ineligible for Montana Healthcare Programs, and have a family income that does not exceed an amount established by the Department.
Mentally Incompetent
According to CFR 441.251, a mentally incompetent individual means an individual who has been declared mentally incompetent by a federal, state, or local court of competent jurisdiction for any purpose, unless the individual has been declared competent for purposes which include the ability to consent to sterilization.
Montana Access to Health (MATH) Web Portal
A secure website on which providers may view members’ medical history, verify member eligibility, submit claims to Montana Healthcare Programs, check the status of a claim, verify the status of a warrant, and download remittance advice reports.
Montana Breast and Cervical Cancer Treatment Program
This program provides Full Montana Healthcare Programs coverage for women who have been screened through the Montana Breast and Cervical Health Program (MBCHP) and diagnosed with breast and/or cervical cancer or a pre-cancerous condition.
Montana Healthcare Programs/HMK Plus
A program that provides health care coverage to specific populations, especially low-income families with children, pregnant women, disabled individuals, and the elderly. Montana Healthcare Programs is administered by state governments under broad federal guidelines.
Passport Referral Number
This is a 7-digit number assigned to Passport providers. When a Passport provider refers a member to another provider for services, this number is given to the other provider and is required when processing the claim.
Passport to Health
A Montana Healthcare Programs medical home program where the member selects a primary care provider who manages the member’s health care needs.
Pay-and-Chase
Montana Healthcare Programs pays a claim and then recovers payment from the third-party carrier that is financially responsible for all or part of the claim.
Pending Claim
These claims have been entered into the system but have not reached final disposition. They require either additional review or are waiting for member eligibility information.
Potential Third-Party Liability
Any entity that may be liable to pay all or part of the medical cost of care for a Montana Healthcare Programs, MHSP or HMK member.
Prior Authorization (PA)
The approval process required before certain services or supplies are paid by Montana Healthcare Programs. Prior authorization must be obtained before providing the service or supply.
Private-Pay
When a member chooses to pay for medical services out of his or her own pocket.
Protocols
Written plans developed by a public health clinic in collaboration with physician and nursing staff. Protocols specify nursing procedures to be followed in giving a specific exam, or providing care for particular conditions. Protocols must by updated and approved by a physician at least annually.
Provider or Provider of Service
An institution, agency, or person:
- • Having a signed agreement with the Department to furnish medical care and goods and/or services to members; and
- Eligible to receive payment from the Department.
Qualified Medicare Beneficiary (QMB)
QMB members are members for whom Montana Healthcare Programs pays their Medicare premiums and some or all of their Medicare coinsurance and deductibles.
Reason and Remark Code
A code which prints on the Montana Healthcare Programs remittance advice (RA) that explains why a claim was denied or suspended. The explanation of the Reason/Remark codes is found at the end of the RA (formerly called EOB code).
Referral
When providers refer members to other Montana Healthcare Programs providers for medically necessary services that they cannot provide.
Remittance Advice (RA)
The results of claims processing (including paid, denied, and pending claims) are listed on the RA.
Relative Value Scale (RVS)
A numerical scale designed to permit comparisons of appropriate prices for various services. The RVS is made up of the relative value units (RVUs) for all the objects in the class for which it is developed.
Relative Value Unit (RVU)
The numerical value given to each service in a relative value scale.
Resource-Based Relative Value Scale (RBRVS)
A method of determining physicians’ fees based on the time, training, skill, and other factors required to deliver various services.
Retroactive Eligibility
When a member is determined to be eligible for Montana Healthcare Programs effective prior to the current date.
Sanction
The penalty for noncompliance with laws, rules, and policies regarding Montana Healthcare Programs. A sanction may include withholding payment from a provider or terminating Montana Healthcare Programs enrollment.
School-Based Services
Medically necessary health-related services provided to Montana Healthcare Programs eligible children up to and including age 20. These services are provided in a school setting by licensed medical professionals.
Specified Low-Income Medicare Beneficiaries (SLMB)
For these members, Montana Healthcare Programs pays the Medicare premium only. They are not eligible for other Montana Healthcare Programs benefits and must pay their own Medicare coinsurance and deductibles.
Spending Down
Members with high medical expenses relative to their income can become eligible for Montana Healthcare Programs by “spending down” their income to specified levels. The member is responsible to pay for services received before eligibility begins, and Montana Healthcare Programs pays for remaining covered services.
Team Care
A restricted services program that is part of Passport to Health. Restricted services programs are designed to assist members in making better health care decisions so that they can avoid overutilizing health services. Team Care members are joined by a team assembled to assist them in accessing health care. The team consists of the member, the PCP, a pharmacy, the Department, and the Department’s quality improvement organization. The team may also include a community-based care manager from the Department's Health Improvement Program.
Third Party Liability (TPL)
Any entity that is, or may be, liable to pay all or part of the medical cost of care for a Montana Healthcare Programs, MHSP or HMK member.
Timely Filing
Providers must submit clean claims (claims that can be processed without additional information or documentation from or action by the provider) to Montana Healthcare Programs within:
- Twelve months from whichever is later:
- the date of service;
- the date retroactive eligibility or disability is determined;
- Six months from the date on the Medicare explanation of benefits approving the service; or
- Six months from the date on an adjustment notice from a third-party payer who has previously processed the claim for the same service, and the adjustment notice is dated after the periods described above.
Usual and Customary
The fee that the provider most frequently charges the general public for a service or item.
WINASAP 5010
WINASAP 5010 is a Windows-based electronic claims entry application for Montana Healthcare Programs. This software was developed as an alternative to submitting claims on paper. For more information, contact the EDI Technical Help Desk. (See Key Contacts.)
End of Definitions and Acronyms Chapter
Search Options
Previous editions of this manual contained an index.
This edition has three search options.
1.Search the whole manual. Open the Complete Manual pane. From your keyboard press the Ctrl and F keys at the same time. A search box will appear. Type in a descriptive or key word (for example "Denials". The search box will show all locations where denials discussed in the manual.
2.Search by Chapter. Open any Chapter tab (for example the "Billing Procedures" tab). From your keyboard press the Ctrl and F keys at the same time. A search box will appear. Type in a descriptive or key word (for example "Denials". The search box will show where denials discussed in just that chapter.