Nutrition Manual
Printing the manual material found at this website for long-term use is not advisable. Department Policy material is updated periodically and it is the responsibility of the users to check and make sure that the policy they are researching or applying has the correct effective date for their circumstances.
If you experience any difficulty opening a section or link from this page, please email the webmaster.
How to Search this manual:
This edition has three search options.
- Search the whole manual. Open the Complete Manual pane. From your keyboard press the Ctrl and F keys at the same time. A search box will appear. Type in a descriptive or key word (for example "Denials". The search box will show all locations where denials discussed in the manual.
- Search by Chapter. Open any Chapter tab (for example the "Billing Procedures" tab). From your keyboard press the Ctrl and F keys at the same time. A search box will appear. Type in a descriptive or key word (for example "Denials". The search box will show where denials discussed in just that chapter.
- Site Search. Search the manual as well as other documents related to a particular search term on the Montana Healthcare Programs Site Specific Search page.
Prior manuals may be located through the provider website archives.
Updated 01/01/2020
Nutrition Manual
To print this manual, right click your mouse and choose "print". Printing the manual material found at this website for long-term use is not advisable. Department Policy material is updated periodically and it is the responsibility of the users to check and make sure that the policy they are researching or applying has the correct effective date for their circumstances.
Update Log
Publication History
This publication supersedes all previous Nutrition handbooks. Published by the Montana Department of Public Health & Human Services, January 2005.
Updated December 2015, July 2017,June 2018, and January 2020.
CPT codes, descriptions and other data only are copyright 2014 American Medical Association (or such other date of publication of CPT). All Rights reserved. Applicable FARS/DFARS Apply.
Update Log
01/01/2020
- Cost Share references removed from Covered Services, Billing Procedures, and Submitting A Claim Chapters.
- Term "Medicaid" replaced with "Montana Healthcare Programs" throughout the manual.
- Terms "member" and "member" replaced with "member".
06/04/2018
Removed commercial resource references.
07/19/2017
Nutrition Manual converted to an HTML format and adapted to 508 Accessibility Standards.
12/31/2015
Nutrition Services, January 2016: HELP Plan-Related Updates and Others
End of Update Log Chapter
Table of Contents
Key Contacts
Key Websites
Introduction
Manual Organization
Manual Maintenance
Rule References
Claim Review (MCA 53-6-111, ARM 37.85.406)
Getting Questions Answered
Other Department Programs
Covered Services
General Coverage Principles
- Services within scope of practice (ARM 37.85.401)
- Licensing
- Services for children (ARM 37.86.2201 - 2221)
Noncovered Services (ARM 37.85.207)
Coverage of Specific Services
Verifying Coverage
Passport to Health Program
Prior Authorization
Prior Authorization
Coordination of Benefits
When members Have Other Coverage
Identifying Additional Coverage
When a member Has Medicare
- Medicare Part B crossover claims
When a member Has TPL (ARM 37.85.407)
- Exceptions to billing third party first
- Requesting an exemption
- When the third party pays or denies a service
- When the third party does not respond
Billing Procedures
Claim Forms
Timely Filing Limits (ARM 37.85.406)
- Tips to avoid timely filing denials
When to Bill Montana Healthcare Programs members (ARM 37.85.406)
Member Co-Payment (ARM 37.85.204)
When members Have Other Insurance
Billing for Retroactively Eligible members
Usual and Customary Charge (ARM 37.85.406)
Coding
Using the Montana Healthcare Programs Fee Schedule
Using Modifiers
Billing Tips for Specific Providers
- Nutrition services
The Most Common Billing Errors and How to Avoid Them
Submitting a Claim
Electronic Claims
Billing Electronically with Paper Attachments
Paper Claims
Member Has Montana Healthcare Programs Coverage Only
Member Has Montana Healthcare Programs and Third Party Liability Coverage
CMS-1500 Agreement
Remittance Advices and Adjustments
The Remittance Advice
- Electronic Remittance Advice
- Paper RA
Sample Remittance Advice
- Credit balance claims
Rebilling and Adjustments
- How long do I have to rebill or adjust a claim?
- Rebilling Montana Healthcare Programs
- When to rebill Montana Healthcare Programs
- How to rebill
- Adjustments
- When to request an adjustment
- Completing an Adjustment Request Form
- Mass adjustments
Payment and the RA
How Payment Is Calculated
Overview
How Payment is Calculated on TPL Claims
How Payment is Calculated on Medicare Crossover Claims
Other Factors That May Affect Payment
Appendix A: Forms
Claim Inquiry Form
Individual Adjustment Request
Paperwork Attachment Cover Sheet
Definitions and Acronyms
Index
End of Table of Contents Chapter
Key Contacts
Hours for Key Contacts are 8:00 a.m. to 5:00 p.m. Monday through Friday (Mountain Time), unless otherwise stated. The phone numbers designated “In state” will not work outside Montana.
member Eligibility
FaxBack
(800) 714-0075 (24 hours)
Voice Response System
(800) 714-0060 (24 hours)
Montana Access to Health (MATH) Web Portal
Medifax EDI
(800) 444-4336 X 2072 (24 hours)
Direct Deposit Arrangements
Providers who would like to receive their remittance advices electronically and electronic funds transfer should call the number below.
(406) 444-5283
EDI Technical Help Desk
For questions regarding electronic claims submission:
(800) 987-6719 In/Out of state
(406) 442-1837 Helena
(850) 385-1705 Fax
Send e-mail inquiries to: MTEDIHelpdesk@conduent.com
Mail to:
Montana EDI
P.O. Box 4936
Helena, MT 59604
Nutrition Services
(406) 444-4189 In/Out of state
(406) 444-1861 Fax
Send written inquiries to:
Program Officer
Nutrition Services
DPHHS
P.O. Box 202951
Helena, MT 59620-2951
Paper Claims
Send paper claims to:
Claims Processing Unit
P.O. Box 8000
Helena, MT 59604
Parents Let’s Unite for Kids (PLUK)
PLUK
516 North 32nd Street
Billings, MT 59101-6003
(406) 255-0540 Phone
(800) 222-7585 Phone
(406) 255-0523 Fax
PLUK E-mail: info@pluk.org
PLUK Website: http://www. pluk.org/
Prior Authorization
For prior authorization requests or for authorization for nutritional services requests not included in the Montana Healthcare Programs fee schedule:
(800) 395-7961
(406) 443-6002 Helena
Mail backup documentation to:
Mountain-Pacific Quality Health
3404 Cooney Drive
Helena, MT 59602
Fax backup documentation to:
(800) 294-1350
(406) 513-1928 Helena
Provider Relations
For questions about eligibility, payments, denials, or general claims questions, or questions about Montana Healthcare Programs or Passport provider enrollment, address or phone number changes:
(800) 624-3958 In/out-of-state
(406) 442-1837 Helena
Send e-mail inquiries to: MTPRHelpdesk@Conduent.com
Send written inquiries to:
Provider Enrollment Unit
P.O. Box 4936
Helena, MT 59604
Provider’s Policy Questions
For policy questions, contact the appropriate division of the Department of Public Health and Human Services; see the Introduction chapter in the General Information for Providers manual.
Secretary of State
The Secretary of State’s office publishes the most current version of the Administrative Rules of Montana (ARM).
(406) 444-2055 Phone
Secretary of State
P.O. Box 202801
Helena, MT 59620-2801
Third Party Liability
For questions about private insurance, Medicare or other third party liability:
(800) 624-3958 In/Out of state
(406) 443-1365 Helena
(406) 442-0357 Fax
Send written inquiries to:
Conduent Third Party Liability Unit
P.O. Box 5838
Helena, MT 59604
End of Key Contacts Chapter
Key Websites
EDI Gateway - https://edisolutionsmmis.portal.conduent.com/gcro/
Gateway is Montana’s HIPAA clearinghouse.
Visit this website for more information on:
- EDI support
- Enrollment
- Manuals
- Provider services
- Software
Health Resources Division -https://dphhs.mt.gov/hrd/
- Big Sky Rx: Helps Medicare members pay for Medicare-approved prescription drug insurance premiums.
- Electronic Billing: How to submit Montana Healthcare Programs claims electronically.
- Healthy Montana Kids: Information on HMK. See website below.
- Montana Healthcare Programs member: Montana Healthcare Programs services for adults and children.
- Montana Healthcare Programs Provider Information: See Montana Access to Health (MATH) Web Portal and Provider Information Website below.
- Montana Healthcare Programs Fraud and Abuse Reporting: Provides telephone numbers to call if you have concerns about Montana Healthcare Programs fraud or abuse.
- Montana Healthcare Programs:
- Passport to Health: Information and enrollment forms for the Passport to Health primary care case management program.
- Prescription Assistance Programs: Summary of information on the programs designed to make prescription drugs more affordable.
- Team Care: Information and enrollment information for the Team Care program.
Montana Access to Health (MATH) Web Portal
Provider Information Website -http://Montana Healthcare Programsprovider.mt.gov/
- Fee schedules
- Forms
- Frequently asked questions (FAQs)
- HIPAA update
- Key contacts
- Links to other websites and more
- Montana Healthcare Programs news
- Newsletters
- Provider enrollment
- Provider manuals, notices and manual replacement pages
- Remittance advice notices
- Upcoming events
Washington Publishing Company -www.wpc-edi.com
- HIPAA guides and other tools
- EDI education
End of Key Websites Chapter
Introduction
Thank you for your willingness to serve members of the Montana Healthcare Programs and other medical assistance programs administered by the Department of Public Health and Human Services.
Manual Organization
This manual provides information specifically for providers of nutrition services. Additional essential information for providers is contained in the separate General Information for Providers manual. Each provider is asked to review both manuals.
A table of contents and an index allow you to quickly find answers to most questions. The margins contain important notes with extra space for writing notes. Each manual contains a list of Key Contacts. We have also included a space on the back of the front cover to record your NPI/API for quick reference when calling Provider Relations.
Manual Maintenance
In order to remain accurate, manuals must be kept current. Changes to manuals are provided through notices and replacement pages, which are posted on the Provider Information website (see Key Websites). When replacing a page in a paper manual, file the old pages and notices in the back of the manual for use with claims that originated under the old policy.
Rule References
Providers must be familiar with all current rules and regulations governing the Montana Healthcare Programs. Provider manuals are to assist providers in billing Montana Healthcare Programs; they do not contain all Montana Healthcare Programs rules and regulations. Rule citations in the text are a reference tool; they are not a summary of the entire rule. In the event that a manual conflicts with a rule, the rule prevails. Links to rules are available on the Provider Information website (see Key Websites). Paper copies of rules are available through the Secretary of State’s office (see Key Contacts).
Providers are responsible for knowing and following current laws and regulations.
In addition to the Montana Healthcare Programs rules outlined in the General Information for Providers manual, the following rules and regulations are also applicable to the nutrition program:
- Code of Federal Regulations (CFR)
- 42 CFR 441 Subpart B
- Montana Code Annotated (MCA)
- MCA 53-6-101
- Administrative Rules of Montana (ARM)
- ARM 37.86.2201–37.86.2209
Claims Review (MCA 53-6-111, ARM 37.85.406)
The Department is committed to paying Montana Healthcare Programs providers’ claims as quickly as possible. Montana Healthcare Programs claims are electronically processed and usually are not reviewed by medical experts prior to payment to determine if the services provided were appropriately billed. Although the computerized system can detect and deny some erroneous claims, there are many erroneous claims which it cannot detect. For this reason, payment of a claim does not mean that the service was correctly billed or the payment made to the provider was correct. The Department performs periodic retrospective reviews, which may lead to the discovery of incorrect billing or incorrect payment. If a claim is paid, and the Department later discovers that the service was incorrectly billed or paid or the claim was erroneous in some other way, the Department is required by Federal regulation to recover any overpayment, regardless of whether the incorrect payment was the result of Department or provider error or other cause.
Getting Questions Answered
The provider manuals are designed to answer most questions; however, questions may arise that require a call to a specific group (such as a prior authorization contractor or Provider Relations). The list of Key Contacts at the front of this manual has important phone numbers and addresses pertaining to this manual. The Introduction chapter in the General Information for Providers manual also has a list of contacts for specific program policy information. Montana Healthcare Programs manuals, notices, replacement pages, fee schedules, forms, and much more are available on the Provider Information website (see Key Websites).
Other Department Programs
The Montana Healthcare Programs nutrition services in this manual are not benefits of the Mental Health Services Plan (MHSP), so the information in this manual does not apply to MHSP. For more information on MHSP, see the mental health manual available on the Provider Information website (see Key Websites).
The Montana Healthcare Programs nutrition services in this manual are not covered benefits of Healthy Montana Kids (HMK). Additional information regarding HMK benefits is available by contacting Blue Cross and Blue Shield of Montana at 1 (877) 543-7669 (toll-free, follow menu) or 1 (855) 258-3489 (toll-free direct), or by visiting the HMK website (see Key Websites).
End of Introduction Chapter
Covered Services
General Coverage Principles
This chapter provides covered services information that applies specifically to services provided by nutrition services providers. Like all health care services received by Montana Healthcare Programs members, services rendered by these providers must also meet the general requirements listed in the General Information for Providers manual, Provider Requirements chapter.
Services within scope of practice (ARM 37.85.401)
Services are covered only when they are within the scope of the provider’s license. As a condition of participation in the Montana Healthcare Programs all providers must comply with all applicable state and Federal statutes, rules and regulations, including but not limited to Federal regulations and statutes found in Title 42 of the Code of Federal Regulations and the United States Code governing the Montana Healthcare Programs and all applicable Montana statutes and rules governing licensure and certification.
Licensing
A provider of nutrition services must be a nutritionist or dietician licensed or registered in accordance with the laws of the state in which he/she is practicing.
Services for children (ARM 37.86.2201–2221)
The Early and Periodic Screening, Diagnosis, and Treatment (EPSDT) program is a comprehensive approach to health care for Montana Healthcare Programs members ages 20 and under. It is designed to prevent, identify, and then treat health problems before they become disabling. Under EPSDT, Montana Healthcare Programs-eligible children may receive any medically necessary covered service, including all nutrition services described in this manual. All applicable Passport to Health and prior authorization requirements apply. See the General Information for Providers manual for more information on the EPSDT program.
Noncovered Services (ARM 37.85.207)
Montana Healthcare Programs does not cover the following services:
- Services provided to Montana Healthcare Programs members who are absent from the state, with the following exceptions:
- Medical emergency
- Required medical services are not available in Montana. Prior authorization may be required; see the Prior Authorization chapter in this manual.
- If the Department has determined that the general practice for members in a particular area of Montana is to use providers in another state
- When out-of-state medical services and all related expenses are less costly than in-state services
- When Montana makes adoption assistance or foster care maintenance payments for a member who is a child residing in another state
Coverage of Specific Services
Nutrition services are included as a component under the EPSDT program. Well-child EPSDT providers should assess the child’s nutritional status at each well-child screen. Children with nutritional problems may be referred to a licensed nutritionist or dietician for further assessment or counseling. The Montana Healthcare Programs nutrition services program covers the following nutrition services for children through age 20 through the EPSDT program:
- Nutrition screening to collect subjective and objective nutritional and dietary data about a child.
- Nutrition counseling with a child or a responsible caregiver, to explain the nutrition assessment and to implement a plan of nutrition care.
- Nutrition assessment for evaluation of a child’s nutritional problems, and design a plan to prevent, improve, or resolve identified nutritional problems, based upon the health objectives, resources, and capacity of the child.
- Nutrition counseling with or for health professionals, researching, or resolving special nutrition problems or referring a child to other services, pertaining to the nutritional needs of the child.
- Nutritional education for routine education for normal nutritional needs.
Verifying Coverage
The easiest way to verify coverage for a specific service is to check the Department’s fee schedule for your provider type. In addition to being listed on the fee schedule, all services provided must also meet the coverage criteria listed in this chapter and in the Provider Requirements chapter of the General Information for Providers manual. Use the current fee schedule in conjunction with the more detailed coding descriptions listed in the current CPT and HCPCS coding books. Use the fee schedule and coding books that pertain to the date of service.
Current fee schedules are available on the Provider Information website (see Key Websites).
End of Covered Services Chapter
Passport to Health Program
For Passport to Health information, see the Passport to Health manual. The manual is available on the Passport to Health page and applicable provider type pages on the Provider Information website.
End of Passport to Health Program Chapter
Prior Authorization
Nutrition services that are a covered service of Montana Healthcare Programs generally do not require prior authorization, but always refer to the current Montana Healthcare Programs fee schedule for PA requirements.
End of Prior Authorization Chapter
Coordination of Benefits
When Members Have Other Coverage
Montana Healthcare Programs members often have coverage through Medicare, workers’ compensation, employment-based coverage, individually purchased coverage, etc. Coordination of benefits is the process of determining which source of coverage is the primary payer in a particular situation. In general, providers should bill other carriers before billing Montana Healthcare Programs, but there are some exceptions (see Exceptions to billing third party first in this chapter). Medicare is processed differently than other sources of coverage.
Identifying Additional Coverage
Medicare or other third party payers (see the General Information for Providers manual, member Eligibility and Responsibilities). If a member has Medicare, the Medicare ID number is provided. If a member has additional coverage, the carrier is shown. Some examples of third party payers include:
- Private health insurance
- Employment-related health insurance
- Workers’ compensation insurance*
- Health insurance from an absent parent
- Automobile insurance*
- Court judgments and settlements*
- Long-term care insurance
*These third party payers (and others) may not be listed on the member’s Montana Healthcare Programs eligibility verification.
Providers should use the same procedures for locating third party sources for Montana Healthcare Programs members as for their non-Montana Healthcare Programs members. Providers cannot refuse service because of a third party payer or potential third party payer.
When a member Has Medicare
Medicare claims are processed and paid differently than other non-Montana Healthcare Programs claims. The other sources of coverage are called third party liability or TPL, but Medicare is not.
Medicare Part B crossover claims
Nutrition services may be covered under Medicare Part B. The Department has an agreement with the Medicare Part B carrier for Montana (Noridian) and the Durable Medical Equipment Regional Carrier [DMERC]) under which the carriers provide the Department with claims for members who have both Medicare and Montana Healthcare Programs coverage. Providers must tell Medicare that they want their claims sent to Montana Healthcare Programs automatically, and must have their Medicare provider number on file with Montana Healthcare Programs.
To avoid confusion and paperwork, submit Medicare Part B crossover claims to Montana Healthcare Programs only when necessary.
When members have both Medicare and Montana Healthcare Programs covered claims, and have made arrangements with both Medicare and Montana Healthcare Programs, Part B services need not be submitted to Montana Healthcare Programs. When a crossover claim is submitted only to Medicare, Medicare will process the claim, submit it to Montana Healthcare Programs, and send the provider an Explanation of Medicare Benefits (EOMB). Providers must check the EOMB for the statement indicating that the claim has been referred to Montana Healthcare Programs for further processing. It is the provider’s responsibility to follow up on crossover claims and make sure they are correctly billed to Montana Healthcare Programs within the timely filing limit (see the Billing Procedures chapter in this manual).
Providers should submit Medicare crossover claims to Montana Healthcare Programs only when:
- The referral to Montana Healthcare Programs statement is missing. In this case, submit a claim and a copy of the Medicare EOMB to Montana Healthcare Programs for processing.
- The referral to Montana Healthcare Programs statement is present, but the provider does not hear from Montana Healthcare Programs within 45 days of receiving the Medicare EOMB. Submit a claim and a copy of the Medicare EOMB to Montana Healthcare Programs for processing.
- Medicare denies the claim, you may submit the claim to Montana Healthcare Programs with the EOMB and denial explanation (as long as the claim has not automatically crossed over from Medicare).
All Part B crossover claims submitted to Montana Healthcare Programs before the 45-day Medicare response time will be returned to the provider.
When submitting electronic claims with paper attachments, see the Billing Electronically with Paper Attachments section of the Submitting a Claim chapter in this manual.
When submitting a claim with the Medicare EOMB, use Montana Healthcare Programs billing instructions and codes. Medicare’s instructions, codes, and modifiers may not be the same as Montana Healthcare Programs’s. The claim must also include the Montana Healthcare Programs provider number and Montana Healthcare Programs member ID number. It is the provider’s responsibility to follow up on crossover claims and make sure they are correctly billed to Montana Healthcare Programs within the timely filing limit (see the Billing Procedures chapter in this manual).
When submitting a Medicare crossover claim to Montana Healthcare Programs, use Montana Healthcare Programs billing instructions and codes; they may not be the same as Medicare’s.
When a Member Has TPL (ARM 37.85.407)
When a Montana Healthcare Programs member has additional medical coverage (other than Medicare), it is often referred to as third party liability or TPL. In most cases, providers must bill other insurance carriers before billing Montana Healthcare Programs.
Providers are required to notify their members that any funds the member receives from third party payers (when the services were billed to Montana Healthcare Programs) must be turned over to the Department. The following words printed on the member’s statement will fulfill this obligation: “When services are covered by Montana Healthcare Programs and another source, any payment the member receives from the other source must be turned over to Montana Healthcare Programs.”
Exceptions to billing third party first
In a few cases, providers may bill Montana Healthcare Programs first:
- When a Montana Healthcare Programs member is also covered by Indian Health Service (IHS) or Crime Victim Compensation, providers must bill Montana Healthcare Programs first. These are not considered a third party liability.
- When a member has Montana Healthcare Programs eligibility and Mental Health Services Plan (MHSP) eligibility for the same month, Montana Healthcare Programs must be billed before MHSP.
- If the third party has only potential liability, such as automobile insurance, the provider may bill Montana Healthcare Programs first. Do not indicate the potential third party on the claim. Instead, notify the Department of the potential third party by sending the claim and notification directly to the Third Party Liability Unit (see Key Contacts).
Requesting an exemption
Providers may request to bill Montana Healthcare Programs first under certain circumstances. In each of these cases, the claim and required information should be sent directly to the Third Party Liability Unit (see Key Contacts).
- When a provider is unable to obtain a valid assignment of benefits, the provider should submit the claim with documentation that the provider attempted to obtain assignment and certification that the attempt was unsuccessful.
- When the provider has billed the third party insurance and has received a non-specific denial (e.g., no member name, date of service, amount billed), submit the claim with a copy of the denial and a letter of explanation.
- When the Child Support Enforcement Division has required an absent parent to have insurance on a child, the claim can be submitted to Montana Healthcare Programs when the following requirements are met:
- The third party carrier has been billed, and 30 days or more have passed since the date of service.
- The claim is accompanied by a certification that the claim was billed to the third party carrier, and payment or denial has not been received.
- If another insurance has been billed, and 90 days have passed with no response, submit the claim with a note explaining that the insurance company has been billed, or attach a copy of the letter sent to the insurance company. Include the date the claim was submitted to the insurance company and certification that there has been no response.
When the third party pays or denies a service
When a third party payer is involved (excluding Medicare) and the other payer:
- Pays the claim, indicate the amount paid when submitting the claim to Montana Healthcare Programs for processing.
- Allows the claim, and the allowed amount went toward the member’s deductible, include the insurance explanation of benefits (EOB) when billing Montana Healthcare Programs.
- Denies the claim, submit the claim and a copy of the denial (including the reason explanation) to Montana Healthcare Programs.
- Denies a line on the claim, bill the denied line on a separate claim and submit to Montana Healthcare Programs. Include the EOB from the other payer as well as an explanation of the reason for denial (e.g., definition of denial codes).
If the provider receives a payment from a third party after the Department has paid the provider, the provider must return the lower of the two payments to the Department within 60 days.
When the third party does not respond
If another insurance has been billed, and 90 days have passed with no response, bill Montana Healthcare Programs as follows:
- Submit the claim and a note explaining that the insurance company has been billed, or attach a copy of the letter sent to the insurance company.
- Include the date the claim was submitted to the insurance company.
- Send this information to the Third Party Liability Unit (see Key Contacts).
End of Coordination of Benefits Chapter
Billing Procedures
Claim Forms
Services provided by nutrition services providers must be billed either electronically or on a CMS-1500 claim form. CMS-1500 forms are available from various publishing companies; they are not available from the Department or Provider Relations.
Timely Filing Limits (ARM 37.85.406)
Providers must submit clean claims to Montana Healthcare Programs within:
- Twelve months from whichever is later:
- the date of service
- the date retroactive eligibility or disability is determined
- For claims involving Medicare or TPL, if the 12-month time limit has passed, providers must submit clean claims to Montana Healthcare Programs:
- Medicare Crossover Claims: Six months from the date on the Medicare explanation of benefits approving the service (if the Medicare claim was timely filed and the member was eligible for Medicare at the time the Medicare claim was filed).
- Claims involving other third party payers (excluding Medicare): Six months from the date on an adjustment notice from a third party payer who has previously processed the claim for the same service, and the adjustment notice is dated after the periods described above.
Clean claims are claims that can be processed without additional information or action from the provider. All problems with claims must be resolved within this 12-month period.
Tips to avoid timely filing denials
- Correct and resubmit denied claims promptly (see the Remittance Advices and Adjustments chapter in this manual).
- If a claim submitted to Montana Healthcare Programs does not appear on the remittance advice within 30 days, contact Provider Relations for claim status (see Key Contacts).
- If another insurer has been billed and 90 days have passed with no response, you can bill Montana Healthcare Programs (see the Coordination of Benefits chapter in this manual for more information).
- To meet timely filing requirements for Medicare/Montana Healthcare Programs crossover claims, see the Coordination of Benefits chapter in this manual.
When to Bill Montana Healthcare Programs Members (ARM 37.85.406)
In most circumstances, providers may not bill Montana Healthcare Programs members for services covered under Montana Healthcare Programs. Exceptions are outlined in ARM 37.85.204.
More specifically, providers cannot bill members directly:
- For the difference between charges and the amount Montana Healthcare Programs paid.
- When the provider bills Montana Healthcare Programs for a covered service, and Montana Healthcare Programs denies the claim because of billing errors.
- When a third party payer does not respond.
- When a member fails to arrive for a scheduled appointment. Montana Healthcare Programs may not be billed for no-show appointments.
- When services are free to the member. Montana Healthcare Programs may not be billed for those services either.
Under certain circumstances, providers may need a signed agreement in order to bill a Montana Healthcare Programs member (see the following table).
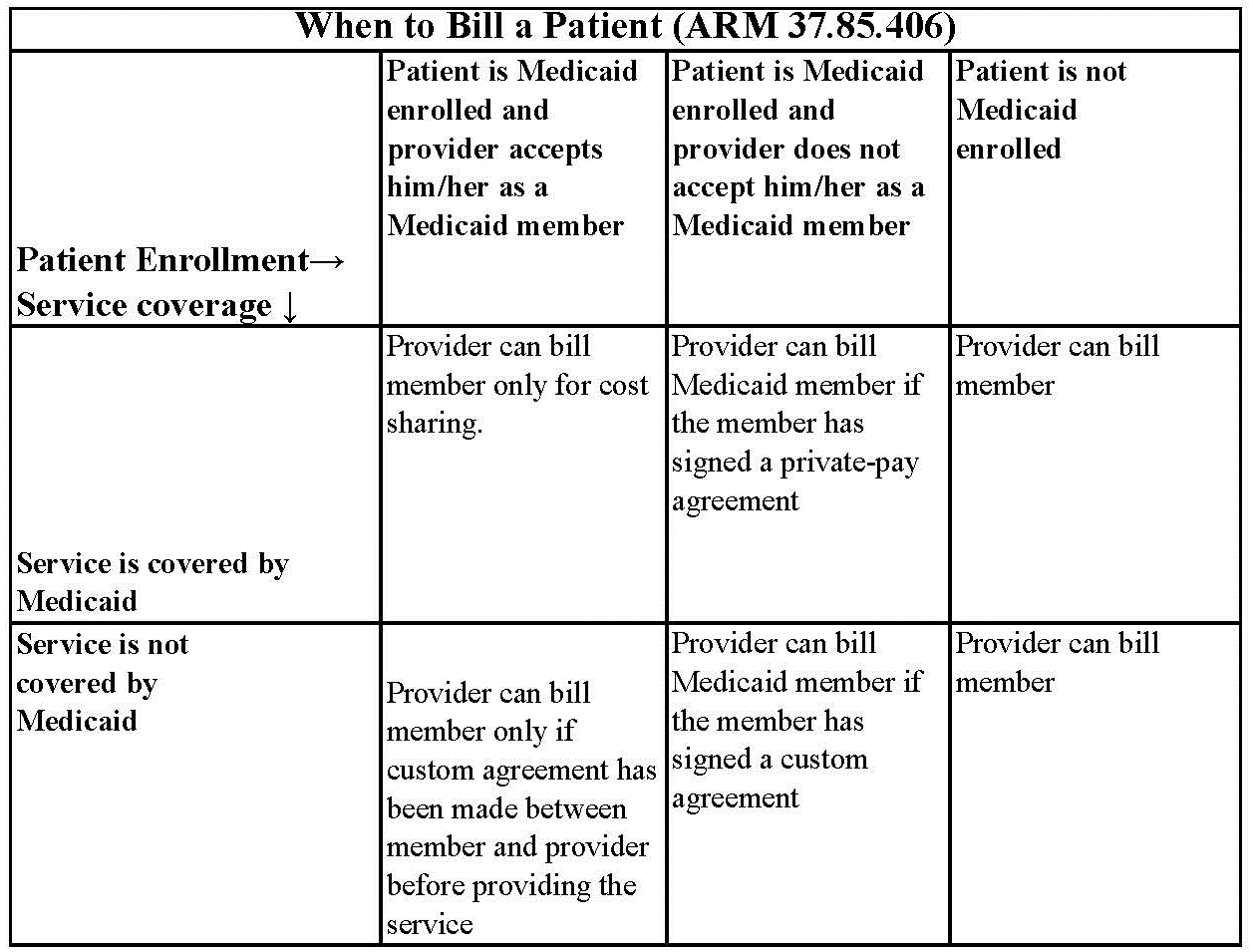
Routine Agreement: This may be a routine agreement between the provider and member which states that the member is not accepted as a Montana Healthcare Programs member, and then he/ she must pay for the services received.
Custom Agreement: This agreement lists the service the member is receiving and states that the service is not covered by Montana Healthcare Programs and that the member will pay for it.
Member Co-Payment (ARM 37.85.204)
Effective for all claims paid on or after January 1, 2020 co-payment will not be assessed.
When Members Have Other Insurance
If a Montana Healthcare Programs member is also covered by Medicare, has other insurance, or some other third party is responsible for the cost of the member’s health care, see the Coordination of Benefits chapter in this manual.
Billing for Retroactively Eligible Members
When a member becomes retroactively eligible for Montana Healthcare Programs, the provider has 12 months from the date retroactive eligibility was determined to bill for those services. When submitting claims for retroactively eligible members, attach a copy of the FA-455 (eligibility determination letter) to the claim if the date of service is more than 12 months earlier than the date the claim is submitted.
When a provider chooses to accept the member from the date retroactive eligibility was effective, and the member has made a full or partial payment for services, the provider must refund the member’s payment for the services before billing Montana Healthcare Programs for the services.
For more information on retroactive eligibility, see the General Information for Providers manual,Member Eligibility and Responsibilities chapter.
Usual and Customary Charge (ARM 37.85.406)
Providers should bill Montana Healthcare Programs their usual and customary charge for each service; that is, the same charge that is made to other payers for that service.
Coding
Standard use of medical coding conventions is required when billing Montana Healthcare Programs. Provider Relations or the Department cannot suggest specific codes to be used in billing for services. For coding assistance and resources, see the table of Coding Resources on the following page. The following suggestions may help reduce coding errors and unnecessary claim denials:
- Use current CPT, HCPCS, and ICD coding books.
- Always read the complete description and guidelines in the coding books. Relying on short descriptions can result in inappropriate billing.
- Attend classes on coding offered by certified coding specialists.
- Use the correct units measurement on the claim.
Coding Resources
Please note that the Department does not endorse the products of any particular publisher.
CPT
Description:
CPT codes and definitions.
Updated each January.
Contact:
American Medical Association
(800) 621-8335
https://commerce.ama-assn.org/store/
CPT Assistant
Description:
A newsletter on CPT coding issues.
Contacts:
American Medical Association
(800) 621-8335
https://commerce.ama-assn.org/store/
HCPCS Level II
Description:
HCPCS codes and definitions.
Updated each January and throughout the year.
Contact:
Available through various publishers and bookstores or from CMS at www.cms.gov.
ICD
Description:
ICD diagnosis and procedure code definitions.
Updated each October.
Contact:
Available through various publishers and bookstores.
Miscellaneous
Various newsletters and other coding resources are available in the commercial marketplace.
Using the Montana Healthcare Programs Fee Schedule
When billing Montana Healthcare Programs, it is important to use the Department’s fee schedule for your provider type in conjunction with the detailed coding descriptions listed in the current CPT and HCPCS coding books.
In addition to covered services and payment rates, fee schedules often contain helpful information such as appropriate modifiers and prior authorization indicators. Department fee schedules are updated each January and July. Current fee schedules are available on the Provider Information website (see Key Websites).
Using Modifiers
- Review the guidelines for using modifiers in the most current CPT, HCPCS, or other helpful resources.
- Always read the complete description for each modifier; some modifiers are described in the CPT manual while others are in the HCPCS book.
- The Montana Healthcare Programs claims processing system recognizes only two pricing modifiers and one informational modifier per claim line. Providers are asked to place any modifiers that affect pricing in the first two modifier fields.
- Modifier 52 must be used when billing for a partial EPSDT well-child screen.
Billing Tips for Specific Providers
Nutrition services
Montana Healthcare Programs reimburses nutritional services in 15-minute units. Four units equal one hour of service. Montana Healthcare Programs will pay up to the rate on the fee schedule for each unit of service billed in the Days or Units field of the claim form. Montana Healthcare Programs will not reimburse for two services that duplicate one another on the same day.
The Most Common Billing Errors and How to Avoid Them
Paper claims are often returned to the provider before they can be processed, and many other claims (both paper and electronic) are denied. To avoid unnecessary returns and denials, double-check each claim to confirm the following items are included and are accurate.
Common Billing Errors
Reasons for Returns or Denials:
Provider’s NPI and/or taxonomy missing or invalid
How to Prevent Returned or Denied Claims:
The provider number is a 10-digit number assigned to the provider during Montana Healthcare Programs enrollment. Verify the correct NPI and taxonomy are on the claim.
Reasons for Returns or Denials:
Authorized signature missing
How to Prevent Returned or Denied Claims:
Each claim must have an authorized signature belonging to the provider, billing clerk, or office personnel. The signature may be typed, stamped, or handwritten.
Reasons for Returns or Denials:
Signature date missing
How to Prevent Returned or Denied Claims:
Each claim must have a signature date.
Reasons for Returns or Denials:
Incorrect claim form used
How to Prevent Returned or Denied Claims:
The claim must be the correct form for the provider type. Services covered in this manual require a CMS-1500 claim form.
Reasons for Returns or Denials:
Information on claim form not legible
How to Prevent Returned or Denied Claims:
Information on the claim form must be legible. Use dark ink and center the information in the field. Information must not be obscured by lines.
Reasons for Returns or Denials:
Member number not on file, or member was not eligible on date of service.
How to Prevent Returned or Denied Claims:
Before providing services to the member:
- View the member’s eligibility information at each visit; Montana Healthcare Programs eligibility may change monthly.
- Verify member eligibility by using one of the methods described in the Member Eligibility and Responsibilities chapter of the General Information for Providers manual.
Reasons for Returns or Denials:
Procedure requires Passport provider referral – No Passport provider number on claim
How to Prevent Returned or Denied Claims:
A Passport provider number must be on the claim form when a referral is required. See the Passport chapter in this manual.
Reasons for Returns or Denials:
Duplicate claim
How to Prevent Returned or Denied Claims:
Check all remittance advices (RAs) for previously submitted claims before resubmitting.
When making changes to previously paid claims, submit an adjustment form rather than a new claim form (see Remittance Advices and Adjustments in this manual).
Allow 45 days for the Medicare/Montana Healthcare Programs Part B crossover claim to appear on the RA before submitting the claim directly to Montana Healthcare Programs.
Reasons for Returns or Denials:
Prior authorization number is missing
How to Prevent Returned or Denied Claims:
Prior authorization (PA) is required for certain services, and the PA number must be on the claim form (see the Prior Authorization chapter in this manual).
Reasons for Returns or Denials:
TPL on file and no credit amount on claim
How to Prevent Returned or Denied Claims:
If the member has any other insurance (or Medicare), bill the other carrier before Montana Healthcare Programs. See the Coordination of Benefits chapter in this manual.
If the member’s TPL coverage has changed, providers must notify the TPL Unit (see Key Contacts) before submitting a claim.
Reasons for Returns or Denials:
Claim past 365-day filing limit
How to Prevent Returned or Denied Claims:
The Claims Processing Unit must receive all clean claims and adjustments within the timely filing limits described in this chapter.
To ensure timely processing, claims and adjustments must be mailed to Claims Processing at the address shown in Key Contacts.
Reasons for Returns or Denials:
Missing Medicare EOMB
How to Prevent Returned or Denied Claims:
All Medicare crossover claims on CMS-1500 forms must have an EOMB attached.
Reasons for Returns or Denials:
Provider is not eligible during dates of services, or provider number terminated
How to Prevent Returned or Denied Claims:
Out-of-state providers must update enrollment early to avoid denials. If enrollment has lapsed, claims submitted with a date of service after the expiration date will be denied until the provider updates his or her enrollment.
New providers cannot bill for services provided before Montana Healthcare Programs enrollment begins.
If a provider is terminated from the Montana Healthcare Program, claims submitted with a date of service after the termination date will be denied.
Reasons for Returns or Denials:
Type of service/procedure is not allowed for provider type
How to Prevent Returned or Denied Claims:
Provider is not allowed to perform the service.
Verify the procedure code is correct using current HCPCS and CPT billing manuals.
Check the Montana Healthcare Programs fee schedule to verify the procedure code is valid for your provider type.
End of Billing Procedures Chapter
Submitting a Claim
Electronic Claims
Professional and institutional claims submitted electronically are referred to as ANSI ASC X12N 837 transactions. Providers who submit claims electronically experience fewer errors and quicker payment. Claims may be submitted electronically by the following methods:
- WINASAP 5010. This free software is available for providers to create and submit claims to Montana Healthcare Programs, MHSP, and HMK (dental and eyeglasses only) and FQHC/RHC. It does not support submissions to Medicare or other payers, and creates an 837 transaction, but does not accept an 835 transaction back from the Department.
- EDI Gateway Clearinghouse. Providers can send claims to the EDI Gateway clearinghouse in X12 837 format using a dial-up connection. Electronic submitters are required to certify their 837 transactions as HIPAA-compliant before sending their transactions through EDI Gateway. EDIFECS certifies the 837 HIPAA transactions at no cost to the provider. EDIFECS certification is completed through EDI Gateway.
- Clearinghouse. Providers can contract with a clearinghouse and send claims to the clearinghouse in whatever format they accept. The provider's clearinghouse then sends the in the X12 837 format. The provider’s clearinghouse also needs to have their 837 transactions certified through EDIFECS before submitting claims. EDIFECS certification is completed through EDI Gateway. For information on electronic claims submission, contact Provider Relations (see Key Contacts).
- Montana Access to Health (MATH) web portal. Providers can upload and download electronic transactions 7 days a week through the web portal. This availability is subject to scheduled and unscheduled host downtime.
- B2B Gateway SFTP/FTPS site. Providers can use this method to send electronic transactions through this secure FTP process. This is typically encountered with high volume/high-frequency submitters.
- MOVEit DMZ. Providers can use this secure transmission protocol and secure storage landing zone (intermediate storage) for the exchange of files between trading partners and Conduent. Its use is intended for those trading partners/submitters who will be submitting a larger volume of physical files (in excess of 20 per day) or whose physical file sizes regularly exceed 2 MB.
Providers should be familiar with the Federal rules and regulations on preparing electronic transactions.
Billing Electronically with Paper Attachments
When submitting claims that require additional supporting documentation, the Attachment Control Number field must be populated with an identifier. Identifier formats can be designed by software vendors or clearinghouses, but the preferred method is the provider’s Montana Healthcare Programs ID number followed by the member’s ID number and the date of service, each separated by a dash:
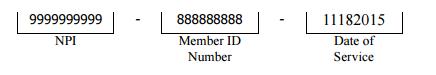
The supporting documentation must be submitted with a Paperwork Attachment Cover Sheet (on the Provider Information website and in Appendix A: Forms). The number in the paper Attachment Control Number field must match the number on the cover sheet. For more information on attachment control numbers and submitting electronic claims, contact Provider Relations (see Key Contacts).
Paper Claims
The services described in this manual are billed on CMS-1500 claim forms. Claims submitted with all of the necessary information are referred to as clean and are usually paid in a timely manner (see the Billing Procedures chapter in this manual).
Claims are completed differently for the different types of coverage a member has. This chapter includes instructions and a sample claim for the following scenarios:
- member has Montana Healthcare Programs coverage only
- member has Montana Healthcare Programs and third party liability coverage
When completing a claim, remember the following:
- Required fields are indicated by “*”.
- Fields that are required if the information is applicable to the situation or member are indicated by “**”.
- Field 24h, EPSDT/Family Planning, is used to override copayment and Passport authorization requirements for certain members or services.
The following are accepted codes:
EPSDT/Family Planning Overrides
Code: 1 member/ Service: EPSDT
Purpose: Overrides some benefit limits for member under age 21.
Code: 2 member/ Service: Family planning
Purpose: Overrides the Passport authorization on the line.
Code: 5 member/ Service: Nursing facility member
Purpose: Overrides the Medicare edit for oxygen services on the line.
Unless otherwise stated, all paper claims are mailed to:
Claims Processing
P.O. Box 8000
Helena, MT 59604
All Montana Healthcare Programs claims must be submitted on Department approved claim forms. CMS-1500 forms are available from various publishing companies; they are not available from the Department or Provider Relations.
EPSDT/ Family Planning Indicators
Code: 1 Member/Service: EPSDT
Purpose: Used when the member is under age 21.
Code: 2 Member/ Service: Family Planning
Purpose: Used when providing family planning services.
Code: 3 Member/ Service: EPSDT and Family Planning
Purpose: Used when the member is under age 21 and is receiving family planning services.
Code: 4 Member/ Service: Pregnancy (any service provided to a pregnant woman)
Purpose: Used when providing services to pregnant women.
Code: 6 Member/ Service: Nursing facility member
Purpose: Used when providing services to nursing facility residents.
Unless otherwise stated, all paper claims are mailed to:
Claims Processing
P.O. Box 8000
Helena, MT 59604
All Montana Healthcare Programs claims must be submitted on Department approved claim forms. CMS-1500 forms are available from various publishing companies; they are not available from the Department or Provider Relations.
member Has Montana Healthcare Programs Coverage Only
Field: 1 Field Title: Program
Instructions: Check Montana Healthcare Programs.
Field: 1a Field Title: Insured’s ID number
Instructions: Leave this field blank for Montana Healthcare Programs only claims.
Field: 2* Field Title: member’s name
Instructions: Enter the member’s name as it appears on the Montana Healthcare Programs member’s eligibility information.
Field: 3 Field Title: member’s birth date and sex
Instructions: member’s birth date in mm/dd/yyyy format. Check M (male) or F (female) box.
Field: 5 Field Title: Insured’s address
Instructions: member’s address.
Field: 10 Field Title: Is member’s condition related to employment, auto accident, other accident?
Instructions: Check Yes or No to indicate whether employment, auto liability, or other accident involvement applies to one or more of the services described in Field 24. If you answered Yes to any of these, enter the two-letter state abbreviation on the Place line to indicate where the accident occurred.
Field: 10d* Field Title: Reserved for local use
Instructions: Enter the member’s Montana Healthcare Programs ID number as it appears on the member’s Montana Healthcare Programs eligibility information.
Field: 11d* Field Title: Is there another health benefit plan?
Instructions: Enter No, or if Yes, follow claim instructions for appropriate coverage later in this chapter.
Field: 14 Field Title: Date of current illness, injury, or pregnancy
Instructions: Enter date in mm/dd/yyyy format. This field is optional for Montana Healthcare Programs-only claims.
Field: 16 Field Title: Dates member unable to work in current occupation
Instructions: If applicable, enter date in mm/dd/yyyy format. This field is optional for Montana Healthcare Programs-only claims.
Field: 17 Field Title: Name of referring provider or other source
Instructions: Enter the name of the referring provider. For Passport members, the name of the member’s Passport provider goes here.
Field: 17a** Field Title: NPI of referring provider
Instructions: Enter the referring or ordering physician’s NPI. For Passport members, enter the member’s Passport provider’s Passport ID number.
Field: 18 Field Title: Hospitalization dates related to current service
Instructions: Enter dates if the medical service is furnished as a result of, or subsequent to, a related hospitalization. This field is optional for Montana Healthcare Programs only claims.
Field: 19 Field Title: Reserved for local use
Instructions: This field is used for any special messages regarding the claim or member.
Field: 20 Field Title: Outside lab?
Instructions: Check No. Montana Healthcare Programs requires all lab tests to be billed directly by the provider who performed them.
Field: 21* Field Title: Diagnosis or nature of illness or injury
Instructions: Enter the appropriate ICD diagnosis codes (up to 4 codes in priority order (primary, secondary)).
Field: 23** Field Title: Prior authorization number
Instructions: If the service requires prior authorization (PA), enter the PA number you received for this service.
Field: 24A* Field Title: Dates of service
Instructions: Enter date of service for each procedure, service, or supply.
Field: 24B* Field Title: Place of service
Instructions: Enter the appropriate two-digit place of service.
Field: 24D* Field Title: Procedures, services, or supplies
Instructions: Enter the appropriate CPT or HCPCS code for the procedure, service, or supply. When applicable, enter the appropriate CPT/HCPCS modifier. Montana Healthcare Programs allows up to three modifiers per procedure code.
Field: 24E* Field Title: Diagnosis code
Instructions: Enter the corresponding diagnosis code reference number (1, 2, 3 or 4) from Field 21 (do not enter the diagnosis code). Any combination of applicable diagnosis reference numbers may be listed on one line.
Field: 24F* Field Title: Charges
Instructions: Enter provider’s usual and customary charge for the procedure on this line.
Field: 24G* Field Title: Days or units
Instructions: Enter the number of units or days for the procedure and date of service billed on this line (see Billing Procedures, Coding for additional tips on days/units).
Field: 24H** Field Title: EPSDT/Family Plan(ning)
Instructions: If applicable, enter the appropriate code for the member/service: 1, 2, 3, 4 or 6 (see complete description in the EPSDT/Family Planning Overrides table in this chapter).
Field: 24I** Field Title: ID qualifier
Instructions:
Field: 28* Field Title: Total charge
Instructions: Enter the sum of all charges billed in Field 24F.
Field: 29 Field Title: Amount paid
Instructions: Leave blank or enter $0.00. Do not report member co-payment or Montana Healthcare Programs payment amounts on this form.
Field: 30* Field Title: Balance due
Instructions: Enter the balance due as recorded in Field 28.
Field: 31* Field Title: Signature and date
Instructions: This field must contain an authorized signature of physician or supplier (include degree or credentials) which is either handwritten, stamped, or computer-generated, and a date.
Field: 32 Field Title: Service facility location
Instructions: Enter the name, address, city, state, and ZIP code of the person, organization, or facility performing the services if other than the member’s home or physician’s office.
Field: 33* Field Title: Billing provider info and phone
Instructions: Enter the name, address, city, state, ZIP code, and phone number and NPI of the provider or supplier who furnished the service.
* = Required field ** = Required, if applicable
member Has Montana Healthcare Programs and Third Party Liability Coverage
Field: 1 Field Title: Program
Instructions: Check Montana Healthcare Programs.
Field: 1a* Field Title: Insured’s ID number
Instructions: Enter the member’s ID number for the primary carrier.
Field: 2* Field Title: member’s name
Instructions: Enter the member’s name as it appears on the Montana Healthcare Programs member’s eligibility information.
Field: 3 Field Title: member’s birth date and sex
Instructions: member’s birth date in mm/dd/yyyy format. Check male or female box.
Field: 4 Field Title: Insured’s name
Instructions: Enter the name of the insured or SAME.
Field: 5 Field Title: member’s address
Instructions: member’s address.
Field: 7 Field Title: Insured’s address
Instructions: Enter the insured’s address and telephone number or SAME.
Field: 9–9d Field Title: Other insured’s information
Instructions: Use these fields only if there are two or more third party insurance carriers (not including Montana Healthcare Programs and Medicare).
Field: 10 Field Title: Is member’s condition related to:
Instructions: Check Yes or No to indicate whether employment, auto liability, or other accident involvement applies to one or more of the services described in Field 24. If you answered yes to any of these, enter the 2-letter state abbreviation on the Place line to indicate in which state the accident occurred.
Field: 10d* Field Title: Reserved for local use
Instructions: Enter the member’s Montana Healthcare Programs ID number as it appears on the member’s Montana Healthcare Programs eligibility information.
Field: 11 Field Title: Insured’s policy group
Instructions: Leave this field blank, or enter the member’s ID number for the primary payer.
Field: 11c* Field Title: Insurance plan or program
Instructions: Enter the name of the other insurance plan or program (e.g., BlueCross BlueShield, NewWest).
Field: 11d* Field Title: Is there another health benefit plan?
Instructions: Check “Yes.”
Field: 14 Field Title: Date of current illness, injury, pregnancy
Instructions: Enter date in mm/dd/yyyy format.
Field: 16 Field Title: Dates member unable to work in current occupation
Instructions: If applicable, enter date in mm/dd/yyyy format.
Field: 17 Field Title: Name of referring provider
Instructions: Enter the name of the referring provider. For Passport members, the name of the member’s Passport provider goes here.
Field: 17a** Field Title: NPI of referring provider
Instructions: Enter the referring or ordering provider’s NPI. For Passport members, enter the member’s Passport provider’s Passport ID number.
Field: 18 Field Title: Hospitalization dates related to current service
Instructions: Enter dates if the medical service is furnished as a result of, or subsequent to, a related hospitalization.
Field: 19 Field Title: Reserved for local use
Instructions: This field is used for any special messages regarding the claim or member.
Field: 20 Field Title: Outside lab?
Instructions: Check No. Montana Healthcare Programs requires all lab tests to be billed directly by the provider who performed them.
Field: 21* Field Title: Diagnosis or nature of illness or injury
Instructions: Enter the appropriate ICD diagnosis codes. Enter up to four codes in priority order (primary, secondary).
Field: 23** Field Title: Prior authorization number
Instructions: If the service requires prior authorization (PA), enter the PA number you received for this service.
Field: 24A* Field Title: Date(s) of service
Instructions: Enter date of service for each procedure, service, or supply.
Field: 24B* Field Title: Place of service
Instructions: Enter the appropriate two-digit place of service.
Field: 24D* Field Title: Procedure, service, or supplies
Instructions: Enter the appropriate CPT or HCPCS code for the procedure, service, or supply. When applicable, enter appropriate modifiers. Montana Healthcare Programs recognizes two pricing and one informational modifier per code.
Field: 24E* Field Title: Diagnosis code
Instructions: Enter the corresponding diagnosis code reference number (1, 2, 3 or 4) from Field 21 (do not enter the diagnosis code). Any combination of applicable diagnosis reference numbers may be listed on one line.
Field: 24F* Field Title: Charges
Instructions: Enter your usual and customary charge for the procedure on this line.
Field: 24G* Field Title: Days or units
Instructions: Enter the number of units or days for the procedure and date of service billed on this line (see Billing Procedures, Coding for additional tips on days/units).
Field: 24H** Field Title: EPSDT/family planning
Instructions: If applicable, enter the appropriate code for the member/service: 1, 2, 3, 4 or 6 (see complete description in the EPSDT/Family Planning Overrides table earlier in this chapter).
Field: 24I** Field Title: ID qualifier
Instructions:
Field: 28* Field Title: Total charge
Instructions: Enter the sum of all charges billed in Field 24f.
Field: 29* Field Title: Amount paid
Instructions: Enter the amount paid by the other insurance. Do not include any adjustment amounts or coinsurance.
Field: 30* Field Title: Balance due
Instructions: Enter the balance due (the amount in Field 28 less the amount in Field 29).
Field: 31* Field Title: Signature and date
Instructions: This field must contain the date and the authorized signature of physician or supplier, which can be handwritten, stamped, or computer-generated.
Field: 32 Field Title: Service facility location information
Instructions: Enter the name, address, city, state, and ZIP code of the person, organization, or facility performing the services if other than the member’s home or physician’s office.
Field: 33* Field Title: Billing provider info and phone
Instructions: Enter the name, address, city, state, ZIP code, phone number, and NPI of the provider or supplier who furnished the service.
* = Required Field ** = Required if applicable
CMS-1500 Agreement
Your signature on the CMS-1500 constitutes your agreement to the terms presented on the back of the form. This form is subject to change by the Centers for Medicare and Montana Healthcare Programs Services (CMS).
Claim Inquiries
Claim inquiries can be obtained electronically through ANSI ASC X12N 276/277 transactions or by contacting Provider Relations. Providers may also contact Provider Relations for questions regarding payments, denials, and other claim questions (see Key Contacts).
If you prefer to communicate with Provider Relations in writing, use the Montana Health Care Programs Claim Inquiry Form on the Provider Information website (see Key Websites). A copy of the form is also in Appendix A: Forms. Complete the top portion of the form with the provider’s name and address.
Provider Relations will respond to the inquiry within 10 days. The response includes the status of the claim: paid (date paid), denied (date denied), or in process. Denied claims will include an explanation of the denial and steps to follow for payment (if the claim is payable).
Avoiding Claim Errors
Claims are often denied or even returned to the provider before they can be processed. To avoid denials and returns, double-check each claim form to confirm the following items are accurate. For more information on returned and denied claims, see the Billing Procedures chapter in this manual.
Common Claim Errors
Claim Error: Required field is blank
Prevention: Check the claim instructions earlier in this chapter for required fields (indicated by * or **). If a required field is blank, the claim may either be returned or denied.
Claim Error: member ID number missing or invalid
Prevention: This is a required field (Field 10d); verify that the member’s Montana Healthcare Programs ID number is listed as it appears on the member’s eligibility information.
Claim Error: member name missing
Prevention: This is a required field (Field 2); check that it is correct.
Claim Error: NPI/API missing or invalid
Prevention: The NPI is a 10-digit number (API is a 7-digit) assigned to the provider. Verify the correct NPI/API is on the claim.
Claim Error: Referring or Passport provider name and ID number missing
Prevention: When a provider refers a member to another provider, include the referring provider’s name and ID number or Passport number (see the Passport chapter in this manual).
Claim Error: Prior authorization number missing
Prevention: When prior authorization (PA) is required for a service, the PA number must be on the claim (see the Prior Authorization chapter in this manual).
Claim Error: Not enough information regarding other coverage
Prevention: Fields 1a and 11d are required fields when a member has other coverage (see examples earlier in this chapter).
Claim Error: Authorized signature missing
Prevention: Each claim must have an authorized signature belonging to the provider, billing clerk, or office personnel. The signature may be typed, stamped, or handwritten.
Claim Error: Signature date missing
Prevention: Each claim must have a signature date.
Claim Error: Incorrect claim form used
Prevention: Services covered in this manual require a CMS-1500 claim form.
Claim Error: Information on claim form not legible
Prevention: Information on the claim form must be legible. Use dark ink and center the information in the field. Information must not be obscured by lines.
Claim Error: Medicare EOMB not attached
Prevention: When Medicare is involved in payment on a claim, the Medicare EOMB must be submitted with the claim or it will be denied.
End of Submitting a Claim Chapter
How Payment Is Calculated
Overview
Though providers do not need the information in this chapter in order to submit claims to the Department, the information allows providers to understand how payment is calculated and to predict approximate payment for particular claims. These examples are for July 2004 and these rates may not apply at other times.
How Payment is Calculated on TPL Claims
When a member has coverage from both Montana Healthcare Programs and another insurance company, the other insurance company is often referred to as third party liability or TPL. In these cases, the other insurance is the primary payer (as described in the Coordination of Benefits chapter in this manual), and Montana Healthcare Programs makes a payment as the secondary payer. For example, a member receives one visit of EPSDT nutrition consultation (S0302). The third party insurance is billed first and pays $15.00. The Montana Healthcare Programs allowed amount for this service totals $30.57. The amount the insurance paid ($15.00) is subtracted from the Montana Healthcare Programs allowed amount ($30.57), leaving a balance of $15.57, which Montana Healthcare Programs will pay on this claim.
Many Montana Healthcare Programs payment methods are based on Medicare, but there are differences. In these cases, the Montana Healthcare Programs method prevails.
How Payment is Calculated on Medicare Crossover Claims
When a member has coverage from both Montana Healthcare Programs and Medicare, Medicare is the primary payer as described in the Coordination of Benefits chapter of this manual. Montana Healthcare Programs then makes a payment as the secondary payer. For the provider types covered in this manual, Montana Healthcare Programs’s payment is calculated so that the total payment to the provider is either the Montana Healthcare Programs allowed amount less the Medicare paid amount or the sum of the Medicare coinsurance and deductible, whichever is lower. This method is sometimes called “lower of” pricing.
Other Factors That May Affect Payment
When Montana Healthcare Programs payment differs from the fee schedule, consider the following:
- The Department pays the lower of the established Montana Healthcare Programs fee or the provider’s charge
- The member may have an incurment amount that must be met before Montana Healthcare Programs will pay for services (see the General Information for Providers manual, member Eligibility and Responsibilities chapter, Coverage for the Medically Needy section.
- Date of service; fees for services may change over time.
- Medicare, incurment, and/or TPL payments, which are shown on the remittance advice.
End of How Payment Is Calculated Chapter
Appendix A: Forms
For the forms listed below and others, see the Forms page on the Provider Information website.
- Montana Healthcare Programs Montana Healthcare Programs/MHSP/HMK Individual Adjustment Request
- Paperwork Attachment Cover Sheet
End of Appendix A: Forms Chapter
Definitions and Acronyms
End of Definitions and Acronyms Chapter
Index
Previous editions of this manual contained an index.
This edition has three search options.
1.Search the whole manual. Open the Complete Manual pane. From your keyboard press the Ctrl and F keys at the same time. A search box will appear. Type in a descriptive or key word (for example "Denials". The search box will show all locations where denials discussed in the manual.
2.Search by Chapter. Open any Chapter tab (for example the "Billing Procedures" tab). From your keyboard press the Ctrl and F keys at the same time. A search box will appear. Type in a descriptive or key word (for example "Denials". The search box will show where denials discussed in just that chapter.
End of Index Chapter
End of Nutrition Manual
Update Log
Publication History
This publication supersedes all previous Nutrition handbooks. Published by the Montana Department of Public Health & Human Services, January 2005.
Updated December 2015, July 2017,June 2018, and January 2020.
CPT codes, descriptions and other data only are copyright 2014 American Medical Association (or such other date of publication of CPT). All Rights reserved. Applicable FARS/DFARS Apply.
Update Log
01/01/2020
- Cost Share references removed from Covered Services, Billing Procedures, and Submitting A Claim Chapters.
- Term "Medicaid" replaced with "Montana Healthcare Programs" throughout the manual.
- Terms "client" and "patient" replaced with "member".
06/04/2018
Removed commercial resource references.
07/19/2017
Nutrition Manual converted to an HTML format and adapted to 508 Accessibility Standards.
12/31/2015
Nutrition Services, January 2016: HELP Plan-Related Updates and Others
End of Update Log Chapter
Table of Contents
Key Contacts
Key Websites
Introduction
Manual Organization
Manual Maintenance
Rule References
Claim Review (MCA 53-6-111, ARM 37.85.406)
Getting Questions Answered
Other Department Programs
Covered Services
General Coverage Principles
- Services within scope of practice (ARM 37.85.401)
- Licensing
- Services for children (ARM 37.86.2201 - 2221)
Noncovered Services (ARM 37.85.207)
Coverage of Specific Services
Verifying Coverage
Passport to Health Program
Prior Authorization
Prior Authorization
Coordination of Benefits
When members Have Other Coverage
Identifying Additional Coverage
When a member Has Medicare
- Medicare Part B crossover claims
When a member Has TPL (ARM 37.85.407)
- Exceptions to billing third party first
- Requesting an exemption
- When the third party pays or denies a service
- When the third party does not respond
Billing Procedures
Claim Forms
Timely Filing Limits (ARM 37.85.406)
- Tips to avoid timely filing denials
When to Bill Montana Healthcare Programs members (ARM 37.85.406)
Member Co-Payment (ARM 37.85.204)
When members Have Other Insurance
Billing for Retroactively Eligible members
Usual and Customary Charge (ARM 37.85.406)
Coding
Using the Montana Healthcare Programs Fee Schedule
Using Modifiers
Billing Tips for Specific Providers
- Nutrition services
The Most Common Billing Errors and How to Avoid Them
Submitting a Claim
Electronic Claims
Billing Electronically with Paper Attachments
Paper Claims
Member Has Montana Healthcare Programs Coverage Only
Member Has Montana Healthcare Programs and Third Party Liability Coverage
CMS-1500 Agreement
Remittance Advices and Adjustments
The Remittance Advice
- Electronic Remittance Advice
- Paper RA
Sample Remittance Advice
- Credit balance claims
Rebilling and Adjustments
- How long do I have to rebill or adjust a claim?
- Rebilling Montana Healthcare Programs
- When to rebill Montana Healthcare Programs
- How to rebill
- Adjustments
- When to request an adjustment
- Completing an Adjustment Request Form
- Mass adjustments
Payment and the RA
How Payment Is Calculated
Overview
How Payment is Calculated on TPL Claims
How Payment is Calculated on Medicare Crossover Claims
Other Factors That May Affect Payment
Appendix A: Forms
Claim Inquiry Form
Individual Adjustment Request
Paperwork Attachment Cover Sheet
Definitions and Acronyms
Index
End of Table of Contents Chapter
Key Websites
EDI Gateway - https://edisolutionsmmis.portal.conduent.com/gcro/
Gateway is Montana’s HIPAA clearinghouse.
Visit this website for more information on:
- EDI support
- Enrollment
- Manuals
- Provider services
- Software
Health Resources Division -https://dphhs.mt.gov/hrd/
- Big Sky Rx: Helps Medicare clients pay for Medicare-approved prescription drug insurance premiums.
- Electronic Billing: How to submit Montana Healthcare Programs claims electronically.
- Healthy Montana Kids: Information on HMK. See website below.
- Montana Healthcare Programs Member: Montana Healthcare Programs services for adults and children.
- Montana Healthcare Programs Provider Information: See Montana Access to Health (MATH) Web Portal and Provider Information Website below.
- Montana Healthcare Programs Fraud and Abuse Reporting: Provides telephone numbers to call if you have concerns about Montana Healthcare Programs fraud or abuse.
- Montana Healthcare Programs
- Passport to Health: Information and enrollment forms for the Passport to Health primary care case management program.
- Prescription Assistance Programs: Summary of information on the programs designed to make prescription drugs more affordable.
- Team Care: Information and enrollment information for the Team Care program.
Montana Access to Health (MATH) Web Portal
- Fee schedules
- Forms
- Frequently asked questions (FAQs)
- HIPAA update
- Key contacts
- Links to other websites and more
- Montana Healthcare Programs news
- Newsletters
- Provider enrollment
- Provider manuals, notices and manual replacement pages
- Remittance advice notices
- Upcoming events
Washington Publishing Company -www.wpc-edi.com
- HIPAA guides and other tools
- EDI education
End of Key Websites Chapter
Introduction
Thank you for your willingness to serve members of the Montana Healthcare Programs program and other medical assistance programs administered by the Department of Public Health and Human Services.
Manual Organization
This manual provides information specifically for providers of nutrition services. Additional essential information for providers is contained in the separate General Information for Providers manual. Each provider is asked to review both manuals.
A table of contents and an index allow you to quickly find answers to most questions. The margins contain important notes with extra space for writing notes. Each manual contains a list of Key Contacts. We have also included a space on the back of the front cover to record your NPI/API for quick reference when calling Provider Relations.
Manual Maintenance
In order to remain accurate, manuals must be kept current. Changes to manuals are provided through notices and replacement pages, which are posted on the Provider Information website (see Key Websites). When replacing a page in a paper manual, file the old pages and notices in the back of the manual for use with claims that originated under the old policy.
Rule References
Providers must be familiar with all current rules and regulations governing the Montana Healthcare Programs program. Provider manuals are to assist providers in billing Montana Healthcare Programs; they do not contain all Montana Healthcare Programs rules and regulations. Rule citations in the text are a reference tool; they are not a summary of the entire rule. In the event that a manual conflicts with a rule, the rule prevails. Links to rules are available on the Provider Information website (see Key Websites). Paper copies of rules are available through the Secretary of State’s office (see Key Contacts).
Providers are responsible for knowing and following current laws and regulations.
In addition to the Montana Healthcare Programs rules outlined in the General Information for Providers manual, the following rules and regulations are also applicable to the nutrition program:
- Code of Federal Regulations (CFR)
- 42 CFR 441 Subpart B
- Montana Code Annotated (MCA)
- MCA 53-6-101
- Administrative Rules of Montana (ARM)
- ARM 37.86.2201–37.86.2209
Claims Review (MCA 53-6-111, ARM 37.85.406)
The Department is committed to paying Montana Healthcare Programs providers’ claims as quickly as possible. Montana Healthcare Programs claims are electronically processed and usually are not reviewed by medical experts prior to payment to determine if the services provided were appropriately billed. Although the computerized system can detect and deny some erroneous claims, there are many erroneous claims which it cannot detect. For this reason, payment of a claim does not mean that the service was correctly billed or the payment made to the provider was correct. The Department performs periodic retrospective reviews, which may lead to the discovery of incorrect billing or incorrect payment. If a claim is paid, and the Department later discovers that the service was incorrectly billed or paid or the claim was erroneous in some other way, the Department is required by Federal regulation to recover any overpayment, regardless of whether the incorrect payment was the result of Department or provider error or other cause.
Getting Questions Answered
The provider manuals are designed to answer most questions; however, questions may arise that require a call to a specific group (such as a prior authorization contractor or Provider Relations). The list of Key Contacts at the front of this manual has important phone numbers and addresses pertaining to this manual. The Introduction chapter in the General Information for Providers manual also has a list of contacts for specific program policy information. Montana Healthcare Programs manuals, notices, replacement pages, fee schedules, forms, and much more are available on the Provider Information website (see Key Websites).
Other Department Programs
The Montana Healthcare Programs nutrition services in this manual are not benefits of the Mental Health Services Plan (MHSP), so the information in this manual does not apply to MHSP. For more information on MHSP, see the mental health manual available on the Provider Information website (see Key Websites).
The Montana Healthcare Programs nutrition services in this manual are not covered benefits of Healthy Montana Kids (HMK). Additional information regarding HMK benefits is available by contacting Blue Cross and Blue Shield of Montana at 1 (877) 543-7669 (toll-free, follow menu) or 1 (855) 258-3489 (toll-free direct), or by visiting the HMK website (see Key Websites).
End of Introduction Chapter
Covered Services
General Coverage Principles
This chapter provides covered services information that applies specifically to services provided by nutrition services providers. Like all health care services received by Montana Healthcare Programs members, services rendered by these providers must also meet the general requirements listed in the General Information for Providers manual, Provider Requirements chapter.
Services within scope of practice (ARM 37.85.401)
Services are covered only when they are within the scope of the provider’s license. As a condition of participation in the Montana Healthcare Programs all providers must comply with all applicable state and Federal statutes, rules and regulations, including but not limited to Federal regulations and statutes found in Title 42 of the Code of Federal Regulations and the United States Code governing the Montana Healthcare Programs and all applicable Montana statutes and rules governing licensure and certification.
Licensing
A provider of nutrition services must be a nutritionist or dietician licensed or registered in accordance with the laws of the state in which he/she is practicing.
Services for children (ARM 37.86.2201–2221)
The Early and Periodic Screening, Diagnosis, and Treatment (EPSDT) program is a comprehensive approach to health care for Montana Healthcare Programs members ages 20 and under. It is designed to prevent, identify, and then treat health problems before they become disabling. Under EPSDT, Montana Healthcare Programs-eligible children may receive any medically necessary covered service, including all nutrition services described in this manual. All applicable Passport to Health and prior authorization requirements apply. See the General Information for Providers manual for more information on the EPSDT program.
Noncovered Services (ARM 37.85.207)
Montana Healthcare Programs does not cover the following services:
- Services provided to Montana Healthcare Programs members who are absent from the state, with the following exceptions:
- Medical emergency
- Required medical services are not available in Montana. Prior authorization may be required; see the Prior Authorization chapter in this manual.
- If the Department has determined that the general practice for members in a particular area of Montana is to use providers in another state
- When out-of-state medical services and all related expenses are less costly than in-state services
- When Montana makes adoption assistance or foster care maintenance payments for a member who is a child residing in another state
Coverage of Specific Services
Nutrition services are included as a component under the EPSDT program. Well-child EPSDT providers should assess the child’s nutritional status at each well-child screen. Children with nutritional problems may be referred to a licensed nutritionist or dietician for further assessment or counseling. The Montana Healthcare Programs nutrition services program covers the following nutrition services for children through age 20 through the EPSDT program:
- Nutrition screening to collect subjective and objective nutritional and dietary data about a child.
- Nutrition counseling with a child or a responsible caregiver, to explain the nutrition assessment and to implement a plan of nutrition care.
- Nutrition assessment for evaluation of a child’s nutritional problems, and design a plan to prevent, improve, or resolve identified nutritional problems, based upon the health objectives, resources, and capacity of the child.
- Nutrition counseling with or for health professionals, researching, or resolving special nutrition problems or referring a child to other services, pertaining to the nutritional needs of the child.
- Nutritional education for routine education for normal nutritional needs.
Verifying Coverage
The easiest way to verify coverage for a specific service is to check the Department’s fee schedule for your provider type. In addition to being listed on the fee schedule, all services provided must also meet the coverage criteria listed in this chapter and in the Provider Requirements chapter of the General Information for Providers manual. Use the current fee schedule in conjunction with the more detailed coding descriptions listed in the current CPT and HCPCS coding books. Use the fee schedule and coding books that pertain to the date of service.
Current fee schedules are available on the Provider Information website (see Key Websites).
End of Covered Services Chapter
Passport to Health Program
For Passport to Health information, see the Passport to Health manual. The manual is available on the Passport to Health page and applicable provider type pages on the Provider Information website.
End of Passport to Health Program Chapter
Prior Authorization
Nutrition services that are a covered service of Montana Healthcare Programs generally do not require prior authorization, but always refer to the current Medicaid fee schedule for PA requirements.
End of Prior Authorization Chapter
Coordination of Benefits
When Members Have Other Coverage
Montana Healthcare Programs members often have coverage through Medicare, workers’ compensation, employment-based coverage, individually purchased coverage, etc. Coordination of benefits is the process of determining which source of coverage is the primary payer in a particular situation. In general, providers should bill other carriers before billing Montana Healthcare Programs, but there are some exceptions (see Exceptions to billing third party first in this chapter). Medicare is processed differently than other sources of coverage.
Identifying Additional Coverage
Medicare or other third party payers (see the General Information for Providers manual, member Eligibility and Responsibilities). If a member has Medicare, the Medicare ID number is provided. If a member has additional coverage, the carrier is shown. Some examples of third party payers include:
- Private health insurance
- Employment-related health insurance
- Workers’ compensation insurance*
- Health insurance from an absent parent
- Automobile insurance*
- Court judgments and settlements*
- Long-term care insurance
*These third party payers (and others) may not be listed on the member’s Montana Healthcare Programs eligibility verification.
Providers should use the same procedures for locating third party sources for Montana Healthcare Programs members as for their non-Montana Healthcare Programs members. Providers cannot refuse service because of a third party payer or potential third party payer.
When a member Has Medicare
Medicare claims are processed and paid differently than other non-Montana Healthcare Programs claims. The other sources of coverage are called third party liability or TPL, but Medicare is not.
Medicare Part B crossover claims
Nutrition services may be covered under Medicare Part B. The Department has an agreement with the Medicare Part B carrier for Montana (Noridian) and the Durable Medical Equipment Regional Carrier [DMERC]) under which the carriers provide the Department with claims for members who have both Medicare and Montana Healthcare Programs coverage. Providers must tell Medicare that they want their claims sent to Montana Healthcare Programs automatically, and must have their Medicare provider number on file with Montana Healthcare Programs.
To avoid confusion and paperwork, submit Medicare Part B crossover claims to Montana Healthcare Programs only when necessary.
When members have both Medicare and Montana Healthcare Programs covered claims, and have made arrangements with both Medicare and Montana Healthcare Programs, Part B services need not be submitted to Montana Healthcare Programs. When a crossover claim is submitted only to Medicare, Medicare will process the claim, submit it to Montana Healthcare Programs, and send the provider an Explanation of Medicare Benefits (EOMB). Providers must check the EOMB for the statement indicating that the claim has been referred to Montana Healthcare Programs for further processing. It is the provider’s responsibility to follow up on crossover claims and make sure they are correctly billed to Montana Healthcare Programs within the timely filing limit (see the Billing Procedures chapter in this manual).
Providers should submit Medicare crossover claims to Montana Healthcare Programs only when:
- The referral to Montana Healthcare Programs statement is missing. In this case, submit a claim and a copy of the Medicare EOMB to Montana Healthcare Programs for processing.
- The referral to Montana Healthcare Programs statement is present, but the provider does not hear from Montana Healthcare Programs within 45 days of receiving the Medicare EOMB. Submit a claim and a copy of the Medicare EOMB to Montana Healthcare Programs for processing.
- Medicare denies the claim, you may submit the claim to Montana Healthcare Programs with the EOMB and denial explanation (as long as the claim has not automatically crossed over from Medicare).
All Part B crossover claims submitted to Montana Healthcare Programs before the 45-day Medicare response time will be returned to the provider.
When submitting electronic claims with paper attachments, see the Billing Electronically with Paper Attachments section of the Submitting a Claim chapter in this manual.
When submitting a claim with the Medicare EOMB, use Montana Healthcare Programs billing instructions and codes. Medicare’s instructions, codes, and modifiers may not be the same as Montana Healthcare Programs’s. The claim must also include the Montana Healthcare Programs provider number and Montana Healthcare Programs member ID number. It is the provider’s responsibility to follow up on crossover claims and make sure they are correctly billed to Montana Healthcare Programs within the timely filing limit (see the Billing Procedures chapter in this manual).
When submitting a Medicare crossover claim to Montana Healthcare Programs, use Montana Healthcare Programs billing instructions and codes; they may not be the same as Medicare’s.
When a Member Has TPL (ARM 37.85.407)
When a Montana Healthcare Programs member has additional medical coverage (other than Medicare), it is often referred to as third party liability or TPL. In most cases, providers must bill other insurance carriers before billing Montana Healthcare Programs.
Providers are required to notify their members that any funds the member receives from third party payers (when the services were billed to Montana Healthcare Programs) must be turned over to the Department. The following words printed on the member’s statement will fulfill this obligation: “When services are covered by Montana Healthcare Programs and another source, any payment the member receives from the other source must be turned over to Montana Healthcare Programs.”
Exceptions to billing third party first
In a few cases, providers may bill Montana Healthcare Programs first:
- When a Montana Healthcare Programs member is also covered by Indian Health Service (IHS) or Crime Victim Compensation, providers must bill Montana Healthcare Programs first. These are not considered a third party liability.
- When a member has Montana Healthcare Programs eligibility and Mental Health Services Plan (MHSP) eligibility for the same month, Montana Healthcare Programs must be billed before MHSP.
- If the third party has only potential liability, such as automobile insurance, the provider may bill Montana Healthcare Programs first. Do not indicate the potential third party on the claim. Instead, notify the Department of the potential third party by sending the claim and notification directly to the Third Party Liability Unit (see Key Contacts).
Requesting an exemption
Providers may request to bill Montana Healthcare Programs first under certain circumstances. In each of these cases, the claim and required information should be sent directly to the Third Party Liability Unit (see Key Contacts).
- When a provider is unable to obtain a valid assignment of benefits, the provider should submit the claim with documentation that the provider attempted to obtain assignment and certification that the attempt was unsuccessful.
- When the provider has billed the third party insurance and has received a non-specific denial (e.g., no member name, date of service, amount billed), submit the claim with a copy of the denial and a letter of explanation.
- When the Child Support Enforcement Division has required an absent parent to have insurance on a child, the claim can be submitted to Montana Healthcare Programs when the following requirements are met:
- The third party carrier has been billed, and 30 days or more have passed since the date of service.
- The claim is accompanied by a certification that the claim was billed to the third party carrier, and payment or denial has not been received.
- If another insurance has been billed, and 90 days have passed with no response, submit the claim with a note explaining that the insurance company has been billed, or attach a copy of the letter sent to the insurance company. Include the date the claim was submitted to the insurance company and certification that there has been no response.
When the third party pays or denies a service
When a third party payer is involved (excluding Medicare) and the other payer:
- Pays the claim, indicate the amount paid when submitting the claim to Montana Healthcare Programs for processing.
- Allows the claim, and the allowed amount went toward the member’s deductible, include the insurance explanation of benefits (EOB) when billing Montana Healthcare Programs.
- Denies the claim, submit the claim and a copy of the denial (including the reason explanation) to Montana Healthcare Programs.
- Denies a line on the claim, bill the denied line on a separate claim and submit to Montana Healthcare Programs. Include the EOB from the other payer as well as an explanation of the reason for denial (e.g., definition of denial codes).
If the provider receives a payment from a third party after the Department has paid the provider, the provider must return the lower of the two payments to the Department within 60 days.
When the third party does not respond
If another insurance has been billed, and 90 days have passed with no response, bill Montana Healthcare Programs as follows:
- Submit the claim and a note explaining that the insurance company has been billed, or attach a copy of the letter sent to the insurance company.
- Include the date the claim was submitted to the insurance company.
- Send this information to the Third Party Liability Unit (see Key Contacts).
End of Coordination of Benefits Chapter
Billing Procedures
Claim Forms
Services provided by nutrition services providers must be billed either electronically or on a CMS-1500 claim form. CMS-1500 forms are available from various publishing companies; they are not available from the Department or Provider Relations.
Timely Filing Limits (ARM 37.85.406)
Providers must submit clean claims to Montana Healthcare Programs within:
- Twelve months from whichever is later:
- the date of service
- the date retroactive eligibility or disability is determined
- For claims involving Medicare or TPL, if the 12-month time limit has passed, providers must submit clean claims to Montana Healthcare Programs:
- Medicare Crossover Claims: Six months from the date on the Medicare explanation of benefits approving the service (if the Medicare claim was timely filed and the member was eligible for Medicare at the time the Medicare claim was filed).
- Claims involving other third party payers (excluding Medicare): Six months from the date on an adjustment notice from a third party payer who has previously processed the claim for the same service, and the adjustment notice is dated after the periods described above.
Clean claims are claims that can be processed without additional information or action from the provider. All problems with claims must be resolved within this 12-month period.
Tips to avoid timely filing denials
- Correct and resubmit denied claims promptly (see the Remittance Advices and Adjustments chapter in this manual).
- If a claim submitted to Montana Healthcare Programs does not appear on the remittance advice within 30 days, contact Provider Relations for claim status (see Key Contacts).
- If another insurer has been billed and 90 days have passed with no response, you can bill Montana Healthcare Programs (see the Coordination of Benefits chapter in this manual for more information).
- To meet timely filing requirements for Medicare/Montana Healthcare Programs crossover claims, see the Coordination of Benefits chapter in this manual.
When to Bill Montana Healthcare Programs Members (ARM 37.85.406)
In most circumstances, providers may not bill Montana Healthcare Programs members for services covered under Montana Healthcare Programs. Exceptions are outlined in ARM 37.85.204.
More specifically, providers cannot bill members directly:
- For the difference between charges and the amount Montana Healthcare Programs paid.
- When the provider bills Montana Healthcare Programs for a covered service, and Montana Healthcare Programs denies the claim because of billing errors.
- When a third party payer does not respond.
- When a member fails to arrive for a scheduled appointment. Montana Healthcare Programs may not be billed for no-show appointments.
- When services are free to the member. Montana Healthcare Programs may not be billed for those services either.
Under certain circumstances, providers may need a signed agreement in order to bill a Montana Healthcare Programs member (see the following table).
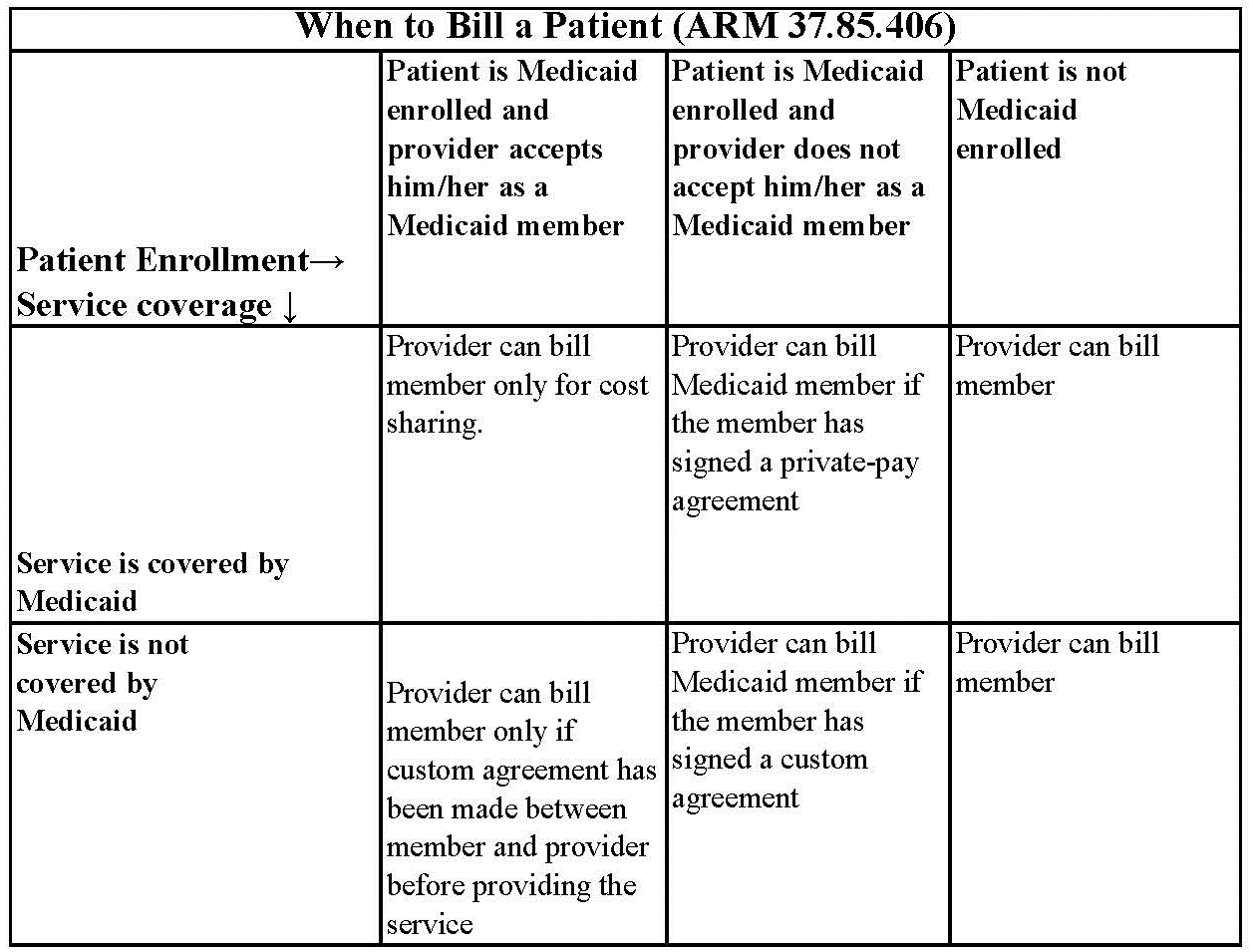
Routine Agreement: This may be a routine agreement between the provider and member which states that the member is not accepted as a Montana Healthcare Programs member, and then he/ she must pay for the services received.
Custom Agreement: This agreement lists the service the member is receiving and states that the service is not covered by Montana Healthcare Programs and that the member will pay for it.
Member Co-Payment (ARM 37.85.204)
Effective for all claims paid on or after January 1, 2020 co-payment will not be assessed.
When Members Have Other Insurance
If a Montana Healthcare Programs member is also covered by Medicare, has other insurance, or some other third party is responsible for the cost of the member’s health care, see the Coordination of Benefits chapter in this manual.
Billing for Retroactively Eligible Members
When a member becomes retroactively eligible for Montana Healthcare Programs, the provider has 12 months from the date retroactive eligibility was determined to bill for those services. When submitting claims for retroactively eligible members, attach a copy of the FA-455 (eligibility determination letter) to the claim if the date of service is more than 12 months earlier than the date the claim is submitted.
When a provider chooses to accept the member from the date retroactive eligibility was effective, and the member has made a full or partial payment for services, the provider must refund the member’s payment for the services before billing Montana Healthcare Programs for the services.
For more information on retroactive eligibility, see the General Information for Providers manual,Member Eligibility and Responsibilities chapter.
Usual and Customary Charge (ARM 37.85.406)
Providers should bill Montana Healthcare Programs their usual and customary charge for each service; that is, the same charge that is made to other payers for that service.
Coding
Standard use of medical coding conventions is required when billing Montana Healthcare Programs. Provider Relations or the Department cannot suggest specific codes to be used in billing for services. For coding assistance and resources, see the table of Coding Resources on the following page. The following suggestions may help reduce coding errors and unnecessary claim denials:
- Use current CPT, HCPCS, and ICD coding books.
- Always read the complete description and guidelines in the coding books. Relying on short descriptions can result in inappropriate billing.
- Attend classes on coding offered by certified coding specialists.
- Use the correct units measurement on the claim.
Coding Resources
Please note that the Department does not endorse the products of any particular publisher.
CPT
Description:
CPT codes and definitions.
Updated each January.
Contact:
American Medical Association
(800) 621-8335
https://commerce.ama-assn.org/store/
CPT Assistant
Description:
A newsletter on CPT coding issues.
Contacts:
American Medical Association
(800) 621-8335
https://commerce.ama-assn.org/store/
HCPCS Level II
Description:
HCPCS codes and definitions.
Updated each January and throughout the year.
Contact:
Available through various publishers and bookstores or from CMS at www.cms.gov.
ICD
Description:
ICD diagnosis and procedure code definitions.
Updated each October.
Contact:
Available through various publishers and bookstores.
Miscellaneous
Various newsletters and other coding resources are available in the commercial marketplace.
Using the Montana Healthcare Programs Fee Schedule
When billing Montana Healthcare Programs, it is important to use the Department’s fee schedule for your provider type in conjunction with the detailed coding descriptions listed in the current CPT and HCPCS coding books.
In addition to covered services and payment rates, fee schedules often contain helpful information such as appropriate modifiers and prior authorization indicators. Department fee schedules are updated each January and July. Current fee schedules are available on the Provider Information website (see Key Websites).
Using Modifiers
- Review the guidelines for using modifiers in the most current CPT, HCPCS, or other helpful resources.
- Always read the complete description for each modifier; some modifiers are described in the CPT manual while others are in the HCPCS book.
- The Montana Healthcare Programs claims processing system recognizes only two pricing modifiers and one informational modifier per claim line. Providers are asked to place any modifiers that affect pricing in the first two modifier fields.
- Modifier 52 must be used when billing for a partial EPSDT well-child screen.
Billing Tips for Specific Providers
Nutrition services
Montana Healthcare Programs reimburses nutritional services in 15-minute units. Four units equal one hour of service. Montana Healthcare Programs will pay up to the rate on the fee schedule for each unit of service billed in the Days or Units field of the claim form. Montana Healthcare Programs will not reimburse for two services that duplicate one another on the same day.
The Most Common Billing Errors and How to Avoid Them
Paper claims are often returned to the provider before they can be processed, and many other claims (both paper and electronic) are denied. To avoid unnecessary returns and denials, double-check each claim to confirm the following items are included and are accurate.
Common Billing Errors
Reasons for Returns or Denials:
Provider’s NPI and/or taxonomy missing or invalid
How to Prevent Returned or Denied Claims:
The provider number is a 10-digit number assigned to the provider during Montana Healthcare Programs enrollment. Verify the correct NPI and taxonomy are on the claim.
Reasons for Returns or Denials:
Authorized signature missing
How to Prevent Returned or Denied Claims:
Each claim must have an authorized signature belonging to the provider, billing clerk, or office personnel. The signature may be typed, stamped, or handwritten.
Reasons for Returns or Denials:
Signature date missing
How to Prevent Returned or Denied Claims:
Each claim must have a signature date.
Reasons for Returns or Denials:
Incorrect claim form used
How to Prevent Returned or Denied Claims:
The claim must be the correct form for the provider type. Services covered in this manual require a CMS-1500 claim form.
Reasons for Returns or Denials:
Information on claim form not legible
How to Prevent Returned or Denied Claims:
Information on the claim form must be legible. Use dark ink and center the information in the field. Information must not be obscured by lines.
Reasons for Returns or Denials:
Member number not on file, or member was not eligible on date of service.
How to Prevent Returned or Denied Claims:
Before providing services to the member:
- View the member’s eligibility information at each visit; Montana Healthcare Programs eligibility may change monthly.
- Verify member eligibility by using one of the methods described in the Member Eligibility and Responsibilities chapter of the General Information for Providers manual.
Reasons for Returns or Denials:
Procedure requires Passport provider referral – No Passport provider number on claim
How to Prevent Returned or Denied Claims:
A Passport provider number must be on the claim form when a referral is required. See the Passport chapter in this manual.
Reasons for Returns or Denials:
Duplicate claim
How to Prevent Returned or Denied Claims:
Check all remittance advices (RAs) for previously submitted claims before resubmitting.
When making changes to previously paid claims, submit an adjustment form rather than a new claim form (see Remittance Advices and Adjustments in this manual).
Allow 45 days for the Medicare/Montana Healthcare Programs Part B crossover claim to appear on the RA before submitting the claim directly to Montana Healthcare Programs.
Reasons for Returns or Denials:
Prior authorization number is missing
How to Prevent Returned or Denied Claims:
Prior authorization (PA) is required for certain services, and the PA number must be on the claim form (see the Prior Authorization chapter in this manual).
Reasons for Returns or Denials:
TPL on file and no credit amount on claim
How to Prevent Returned or Denied Claims:
If the member has any other insurance (or Medicare), bill the other carrier before Montana Healthcare Programs. See the Coordination of Benefits chapter in this manual.
If the member’s TPL coverage has changed, providers must notify the TPL Unit (see Key Contacts) before submitting a claim.
Reasons for Returns or Denials:
Claim past 365-day filing limit
How to Prevent Returned or Denied Claims:
The Claims Processing Unit must receive all clean claims and adjustments within the timely filing limits described in this chapter.
To ensure timely processing, claims and adjustments must be mailed to Claims Processing at the address shown in Key Contacts.
Reasons for Returns or Denials:
Missing Medicare EOMB
How to Prevent Returned or Denied Claims:
All Medicare crossover claims on CMS-1500 forms must have an EOMB attached.
Reasons for Returns or Denials:
Provider is not eligible during dates of services, or provider number terminated
How to Prevent Returned or Denied Claims:
Out-of-state providers must update enrollment early to avoid denials. If enrollment has lapsed, claims submitted with a date of service after the expiration date will be denied until the provider updates his or her enrollment.
New providers cannot bill for services provided before Montana Healthcare Programs enrollment begins.
If a provider is terminated from the Montana Healthcare Program, claims submitted with a date of service after the termination date will be denied.
Reasons for Returns or Denials:
Type of service/procedure is not allowed for provider type
How to Prevent Returned or Denied Claims:
Provider is not allowed to perform the service.
Verify the procedure code is correct using current HCPCS and CPT billing manuals.
Check the Montana Healthcare Programs fee schedule to verify the procedure code is valid for your provider type.
End of Billing Procedures Chapter
Submitting a Claim
Electronic Claims
Professional and institutional claims submitted electronically are referred to as ANSI ASC X12N 837 transactions. Providers who submit claims electronically experience fewer errors and quicker payment. Claims may be submitted electronically by the following methods:
- WINASAP 5010. This free software is available for providers to create and submit claims to Montana Healthcare Programs, MHSP, and HMK (dental and eyeglasses only) and FQHC/RHC. It does not support submissions to Medicare or other payers, and creates an 837 transaction, but does not accept an 835 transaction back from the Department.
- EDI Gateway Clearinghouse. Providers can send claims to the EDI Gateway clearinghouse in X12 837 format using a dial-up connection. Electronic submitters are required to certify their 837 transactions as HIPAA-compliant before sending their transactions through EDI Gateway. EDIFECS certifies the 837 HIPAA transactions at no cost to the provider. EDIFECS certification is completed through EDI Gateway.
- Clearinghouse. Providers can contract with a clearinghouse and send claims to the clearinghouse in whatever format they accept. The provider's clearinghouse then sends the in the X12 837 format. The provider’s clearinghouse also needs to have their 837 transactions certified through EDIFECS before submitting claims. EDIFECS certification is completed through EDI Gateway. For information on electronic claims submission, contact Provider Relations (see Key Contacts).
- Montana Access to Health (MATH) web portal. Providers can upload and download electronic transactions 7 days a week through the web portal. This availability is subject to scheduled and unscheduled host downtime.
- B2B Gateway SFTP/FTPS site. Providers can use this method to send electronic transactions through this secure FTP process. This is typically encountered with high volume/high-frequency submitters.
- MOVEit DMZ. Providers can use this secure transmission protocol and secure storage landing zone (intermediate storage) for the exchange of files between trading partners and Conduent. Its use is intended for those trading partners/submitters who will be submitting a larger volume of physical files (in excess of 20 per day) or whose physical file sizes regularly exceed 2 MB.
Providers should be familiar with the Federal rules and regulations on preparing electronic transactions.
Billing Electronically with Paper Attachments
When submitting claims that require additional supporting documentation, the Attachment Control Number field must be populated with an identifier. Identifier formats can be designed by software vendors or clearinghouses, but the preferred method is the provider’s Montana Healthcare Programs ID number followed by the member’s ID number and the date of service, each separated by a dash:
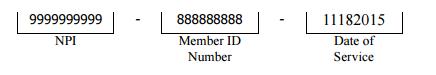
The supporting documentation must be submitted with a Paperwork Attachment Cover Sheet (on the Provider Information website and in Appendix A: Forms). The number in the paper Attachment Control Number field must match the number on the cover sheet. For more information on attachment control numbers and submitting electronic claims, contact Provider Relations (see Key Contacts).
Paper Claims
The services described in this manual are billed on CMS-1500 claim forms. Claims submitted with all of the necessary information are referred to as clean and are usually paid in a timely manner (see the Billing Procedures chapter in this manual).
Claims are completed differently for the different types of coverage a member has. This chapter includes instructions and a sample claim for the following scenarios:
- member has Montana Healthcare Programs coverage only
- member has Montana Healthcare Programs and third party liability coverage
When completing a claim, remember the following:
- Required fields are indicated by “*”.
- Fields that are required if the information is applicable to the situation or member are indicated by “**”.
- Field 24h, EPSDT/Family Planning, is used to override copayment and Passport authorization requirements for certain members or services.
The following are accepted codes:
EPSDT/Family Planning Overrides
Code: 1 member/ Service: EPSDT
Purpose: Overrides some benefit limits for member under age 21.
Code: 2 member/ Service: Family planning
Purpose: Overrides the Passport authorization on the line.
Code: 3 member/ Service: EPSDT and family planning
Purpose: Overrides Passport authorization for persons under the age of 21.
Code: 5 member/ Service: Nursing facility member
Purpose: Overrides the Medicare edit for oxygen services on the line.
Unless otherwise stated, all paper claims are mailed to:
Claims Processing
P.O. Box 8000
Helena, MT 59604
All Montana Healthcare Programs claims must be submitted on Department approved claim forms. CMS-1500 forms are available from various publishing companies; they are not available from the Department or Provider Relations.
EPSDT/ Family Planning Indicators
Code: 1 Member/Service: EPSDT
Purpose: Used when the member is under age 21.
Code: 2 Member/ Service: Family Planning
Purpose: Used when providing family planning services.
Code: 3 Member/ Service: EPSDT and Family Planning
Purpose: Used when the member is under age 21 and is receiving family planning services.
Code: 4 Member/ Service: Pregnancy (any service provided to a pregnant woman)
Purpose: Used when providing services to pregnant women.
Code: 6 Member/ Service: Nursing facility member
Purpose: Used when providing services to nursing facility residents.
Unless otherwise stated, all paper claims are mailed to:
Claims Processing
P.O. Box 8000
Helena, MT 59604
All Montana Healthcare Programs claims must be submitted on Department approved claim forms. CMS-1500 forms are available from various publishing companies; they are not available from the Department or Provider Relations.
Client Has Medicaid Coverage Only
Field: 1 Field Title: Program
Instructions: Check Medicaid.
Field: 1a Field Title: Insured’s ID number
Instructions: Leave this field blank for Montana Healthcare Programs only claims.
Field: 2* Field Title: member’s name
Instructions: Enter the member’s name as it appears on the Montana Healthcare Programs member’s eligibility information.
Field: 3 Field Title: member’s birth date and sex
Instructions: member’s birth date in mm/dd/yyyy format. Check M (male) or F (female) box.
Field: 5 Field Title: Insured’s address
Instructions: member’s address.
Field: 10 Field Title: Is member’s condition related to employment, auto accident, other accident?
Instructions: Check Yes or No to indicate whether employment, auto liability, or other accident involvement applies to one or more of the services described in Field 24. If you answered Yes to any of these, enter the two-letter state abbreviation on the Place line to indicate where the accident occurred.
Field: 10d* Field Title: Reserved for local use
Instructions: Enter the member’s Montana Healthcare Programs ID number as it appears on the member’s Montana Healthcare Programs eligibility information.
Field: 11d* Field Title: Is there another health benefit plan?
Instructions: Enter No, or if Yes, follow claim instructions for appropriate coverage later in this chapter.
Field: 14 Field Title: Date of current illness, injury, or pregnancy
Instructions: Enter date in mm/dd/yyyy format. This field is optional for Montana Healthcare Programs-only claims.
Field: 16 Field Title: Dates member unable to work in current occupation
Instructions: If applicable, enter date in mm/dd/yyyy format. This field is optional for Montana Healthcare Programs-only claims.
Field: 17 Field Title: Name of referring provider or other source
Instructions: Enter the name of the referring provider. For Passport members, the name of the member’s Passport provider goes here.
Field: 17a** Field Title: NPI of referring provider
Instructions: Enter the referring or ordering physician’s NPI. For Passport members, enter the member’s Passport provider’s Passport ID number.
Field: 18 Field Title: Hospitalization dates related to current service
Instructions: Enter dates if the medical service is furnished as a result of, or subsequent to, a related hospitalization. This field is optional for Montana Healthcare Programs only claims.
Field: 19 Field Title: Reserved for local use
Instructions: This field is used for any special messages regarding the claim or member.
Field: 20 Field Title: Outside lab?
Instructions: Check No. Montana Healthcare Programs requires all lab tests to be billed directly by the provider who performed them.
Field: 21* Field Title: Diagnosis or nature of illness or injury
Instructions: Enter the appropriate ICD diagnosis codes (up to 4 codes in priority order (primary, secondary)).
Field: 23** Field Title: Prior authorization number
Instructions: If the service requires prior authorization (PA), enter the PA number you received for this service.
Field: 24A* Field Title: Dates of service
Instructions: Enter date of service for each procedure, service, or supply.
Field: 24B* Field Title: Place of service
Instructions: Enter the appropriate two-digit place of service.
Field: 24D* Field Title: Procedures, services, or supplies
Instructions: Enter the appropriate CPT or HCPCS code for the procedure, service, or supply. When applicable, enter the appropriate CPT/HCPCS modifier. Montana Healthcare Programs allows up to three modifiers per procedure code.
Field: 24E* Field Title: Diagnosis code
Instructions: Enter the corresponding diagnosis code reference number (1, 2, 3 or 4) from Field 21 (do not enter the diagnosis code). Any combination of applicable diagnosis reference numbers may be listed on one line.
Field: 24F* Field Title: Charges
Instructions: Enter provider’s usual and customary charge for the procedure on this line.
Field: 24G* Field Title: Days or units
Instructions: Enter the number of units or days for the procedure and date of service billed on this line (see Billing Procedures, Coding for additional tips on days/units).
Field: 24H** Field Title: EPSDT/Family Plan(ning)
Instructions: If applicable, enter the appropriate code for the member/service: 1, 2, 3, 4 or 6 (see complete description in the EPSDT/Family Planning Overrides table in this chapter).
Field: 24I** Field Title: ID qualifier
Instructions:
Field: 28* Field Title: Total charge
Instructions: Enter the sum of all charges billed in Field 24F.
Field: 29 Field Title: Amount paid
Instructions: Leave blank or enter $0.00. Do not report member Montana Healthcare Programs payment amounts on this form.
Field: 30* Field Title: Balance due
Instructions: Enter the balance due as recorded in Field 28.
Field: 31* Field Title: Signature and date
Instructions: This field must contain an authorized signature of physician or supplier (include degree or credentials) which is either handwritten, stamped, or computer-generated, and a date.
Field: 32 Field Title: Service facility location
Instructions: Enter the name, address, city, state, and ZIP code of the person, organization, or facility performing the services if other than the member’s home or physician’s office.
Field: 33* Field Title: Billing provider info and phone
Instructions: Enter the name, address, city, state, ZIP code, and phone number and NPI of the provider or supplier who furnished the service.
* = Required field ** = Required, if applicable
member Has Montana Healthcare Programs and Third Party Liability Coverage
Field: 1 Field Title: Program
Instructions: Check Montana Healthcare Programs.
Field: 1a* Field Title: Insured’s ID number
Instructions: Enter the member’s ID number for the primary carrier.
Field: 2* Field Title: member’s name
Instructions: Enter the member’s name as it appears on the Montana Healthcare Programs member’s eligibility information.
Field: 3 Field Title: member’s birth date and sex
Instructions: member’s birth date in mm/dd/yyyy format. Check male or female box.
Field: 4 Field Title: Insured’s name
Instructions: Enter the name of the insured or SAME.
Field: 5 Field Title: member’s address
Instructions: member’s address.
Field: 7 Field Title: Insured’s address
Instructions: Enter the insured’s address and telephone number or SAME.
Field: 9–9d Field Title: Other insured’s information
Instructions: Use these fields only if there are two or more third party insurance carriers (not including Montana Healthcare Programs and Medicare).
Field: 10 Field Title: Is member’s condition related to:
Instructions: Check Yes or No to indicate whether employment, auto liability, or other accident involvement applies to one or more of the services described in Field 24. If you answered yes to any of these, enter the 2-letter state abbreviation on the Place line to indicate in which state the accident occurred.
Field: 10d* Field Title: Reserved for local use
Instructions: Enter the member’s Montana Healthcare Programs ID number as it appears on the member’s Montana Healthcare Programs eligibility information.
Field: 11 Field Title: Insured’s policy group
Instructions: Leave this field blank, or enter the member’s ID number for the primary payer.
Field: 11c* Field Title: Insurance plan or program
Instructions: Enter the name of the other insurance plan or program (e.g., BlueCross BlueShield, NewWest).
Field: 11d* Field Title: Is there another health benefit plan?
Instructions: Check “Yes.”
Field: 14 Field Title: Date of current illness, injury, pregnancy
Instructions: Enter date in mm/dd/yyyy format.
Field: 16 Field Title: Dates member unable to work in current occupation
Instructions: If applicable, enter date in mm/dd/yyyy format.
Field: 17 Field Title: Name of referring provider
Instructions: Enter the name of the referring provider. For Passport members, the name of the member’s Passport provider goes here.
Field: 17a** Field Title: NPI of referring provider
Instructions: Enter the referring or ordering provider’s NPI. For Passport members, enter the member’s Passport provider’s Passport ID number.
Field: 18 Field Title: Hospitalization dates related to current service
Instructions: Enter dates if the medical service is furnished as a result of, or subsequent to, a related hospitalization.
Field: 19 Field Title: Reserved for local use
Instructions: This field is used for any special messages regarding the claim or member.
Field: 20 Field Title: Outside lab?
Instructions: Check No. Montana Healthcare Programs requires all lab tests to be billed directly by the provider who performed them.
Field: 21* Field Title: Diagnosis or nature of illness or injury
Instructions: Enter the appropriate ICD diagnosis codes. Enter up to four codes in priority order (primary, secondary).
Field: 23** Field Title: Prior authorization number
Instructions: If the service requires prior authorization (PA), enter the PA number you received for this service.
Field: 24A* Field Title: Date(s) of service
Instructions: Enter date of service for each procedure, service, or supply.
Field: 24B* Field Title: Place of service
Instructions: Enter the appropriate two-digit place of service.
Field: 24D* Field Title: Procedure, service, or supplies
Instructions: Enter the appropriate CPT or HCPCS code for the procedure, service, or supply. When applicable, enter appropriate modifiers. Montana Healthcare Programs recognizes two pricing and one informational modifier per code.
Field: 24E* Field Title: Diagnosis code
Instructions: Enter the corresponding diagnosis code reference number (1, 2, 3 or 4) from Field 21 (do not enter the diagnosis code). Any combination of applicable diagnosis reference numbers may be listed on one line.
Field: 24F* Field Title: Charges
Instructions: Enter your usual and customary charge for the procedure on this line.
Field: 24G* Field Title: Days or units
Instructions: Enter the number of units or days for the procedure and date of service billed on this line (see Billing Procedures, Coding for additional tips on days/units).
Field: 24H** Field Title: EPSDT/family planning
Instructions: If applicable, enter the appropriate code for the member/service: 1, 2, 3, 4 or 6 (see complete description in the EPSDT/Family Planning Overrides table earlier in this chapter).
Field: 24I** Field Title: ID qualifier
Instructions:
Field: 28* Field Title: Total charge
Instructions: Enter the sum of all charges billed in Field 24f.
Field: 29* Field Title: Amount paid
Instructions: Enter the amount paid by the other insurance. Do not include any adjustment amounts or coinsurance.
Field: 30* Field Title: Balance due
Instructions: Enter the balance due (the amount in Field 28 less the amount in Field 29).
Field: 31* Field Title: Signature and date
Instructions: This field must contain the date and the authorized signature of physician or supplier, which can be handwritten, stamped, or computer-generated.
Field: 32 Field Title: Service facility location information
Instructions: Enter the name, address, city, state, and ZIP code of the person, organization, or facility performing the services if other than the member’s home or physician’s office.
Field: 33* Field Title: Billing provider info and phone
Instructions: Enter the name, address, city, state, ZIP code, phone number, and NPI of the provider or supplier who furnished the service.
* = Required Field ** = Required if applicable
CMS-1500 Agreement
Your signature on the CMS-1500 constitutes your agreement to the terms presented on the back of the form. This form is subject to change by the Centers for Medicare and Montana Healthcare Programs Services (CMS).
Claim Inquiries
Claim inquiries can be obtained electronically through ANSI ASC X12N 276/277 transactions or by contacting Provider Relations. Providers may also contact Provider Relations for questions regarding payments, denials, and other claim questions (see Key Contacts).
If you prefer to communicate with Provider Relations in writing, use the Montana Health Care Programs Claim Inquiry Form on the Provider Information website (see Key Websites). A copy of the form is also in Appendix A: Forms. Complete the top portion of the form with the provider’s name and address.
Provider Relations will respond to the inquiry within 10 days. The response includes the status of the claim: paid (date paid), denied (date denied), or in process. Denied claims will include an explanation of the denial and steps to follow for payment (if the claim is payable).
Avoiding Claim Errors
Claims are often denied or even returned to the provider before they can be processed. To avoid denials and returns, double-check each claim form to confirm the following items are accurate. For more information on returned and denied claims, see the Billing Procedures chapter in this manual.
Common Claim Errors
Claim Error: Required field is blank
Prevention: Check the claim instructions earlier in this chapter for required fields (indicated by * or **). If a required field is blank, the claim may either be returned or denied.
Claim Error: member ID number missing or invalid
Prevention: This is a required field (Field 10d); verify that the member’s Montana Healthcare Programs ID number is listed as it appears on the member’s eligibility information.
Claim Error: member name missing
Prevention: This is a required field (Field 2); check that it is correct.
Claim Error: NPI/API missing or invalid
Prevention: The NPI is a 10-digit number (API is a 7-digit) assigned to the provider. Verify the correct NPI/API is on the claim.
Claim Error: Referring or Passport provider name and ID number missing
Prevention: When a provider refers a member to another provider, include the referring provider’s name and ID number or Passport number (see the Passport chapter in this manual).
Claim Error: Prior authorization number missing
Prevention: When prior authorization (PA) is required for a service, the PA number must be on the claim (see the Prior Authorization chapter in this manual).
Claim Error: Not enough information regarding other coverage
Prevention: Fields 1a and 11d are required fields when a member has other coverage (see examples earlier in this chapter).
Claim Error: Authorized signature missing
Prevention: Each claim must have an authorized signature belonging to the provider, billing clerk, or office personnel. The signature may be typed, stamped, or handwritten.
Claim Error: Signature date missing
Prevention: Each claim must have a signature date.
Claim Error: Incorrect claim form used
Prevention: Services covered in this manual require a CMS-1500 claim form.
Claim Error: Information on claim form not legible
Prevention: Information on the claim form must be legible. Use dark ink and center the information in the field. Information must not be obscured by lines.
Claim Error: Medicare EOMB not attached
Prevention: When Medicare is involved in payment on a claim, the Medicare EOMB must be submitted with the claim or it will be denied.
End of Submitting a Claim Chapter
How Payment Is Calculated
Overview
Though providers do not need the information in this chapter in order to submit claims to the Department, the information allows providers to understand how payment is calculated and to predict approximate payment for particular claims. These examples are for July 2004 and these rates may not apply at other times.
How Payment is Calculated on TPL Claims
When a member has coverage from both Montana Healthcare Programs and another insurance company, the other insurance company is often referred to as third party liability or TPL. In these cases, the other insurance is the primary payer (as described in the Coordination of Benefits chapter in this manual), and Montana Healthcare Programs makes a payment as the secondary payer. For example, a member receives one visit of EPSDT nutrition consultation (S0302). The third party insurance is billed first and pays $15.00. The Montana Healthcare Programs allowed amount for this service totals $30.57. The amount the insurance paid ($15.00) is subtracted from the Montana Healthcare Programs allowed amount ($30.57), leaving a balance of $15.57, which Montana Healthcare Programs will pay on this claim.
Many Montana Healthcare Programs payment methods are based on Medicare, but there are differences. In these cases, the Montana Healthcare Programs method prevails.
How Payment is Calculated on Medicare Crossover Claims
When a member has coverage from both Montana Healthcare Programs and Medicare, Medicare is the primary payer as described in the Coordination of Benefits chapter of this manual. Montana Healthcare Programs then makes a payment as the secondary payer. For the provider types covered in this manual, Montana Healthcare Programs’s payment is calculated so that the total payment to the provider is either the Montana Healthcare Programs allowed amount less the Medicare paid amount or the sum of the Medicare coinsurance and deductible, whichever is lower. This method is sometimes called “lower of” pricing.
Other Factors That May Affect Payment
When Montana Healthcare Programs payment differs from the fee schedule, consider the following:
- The Department pays the lower of the established Montana Healthcare Programs fee or the provider’s charge
- The member may have an incurment amount that must be met before Montana Healthcare Programs will pay for services (see the General Information for Providers manual, member Eligibility and Responsibilities chapter, Coverage for the Medically Needy section.
- Date of service; fees for services may change over time.
- Cost sharing, Medicare, and/or TPL payments, which are shown on the remittance advice.
End of How Payment Is Calculated Chapter
How Payment Is Calculated
Overview
Though providers do not need the information in this chapter in order to submit claims to the Department, the information allows providers to understand how payment is calculated and to predict approximate payment for particular claims. These examples are for July 2004 and these rates may not apply at other times.
How Payment is Calculated on TPL Claims
When a member has coverage from both Montana Healthcare Programs and another insurance company, the other insurance company is often referred to as third party liability or TPL. In these cases, the other insurance is the primary payer (as described in the Coordination of Benefits chapter in this manual), and Montana Healthcare Programs makes a payment as the secondary payer. For example, a member receives one visit of EPSDT nutrition consultation (S0302). The third party insurance is billed first and pays $15.00. The Montana Healthcare Programs allowed amount for this service totals $30.57. The amount the insurance paid ($15.00) is subtracted from the Montana Healthcare Programs allowed amount ($30.57), leaving a balance of $15.57, which Montana Healthcare Programs will pay on this claim.
Many Montana Healthcare Programs payment methods are based on Medicare, but there are differences. In these cases, the Montana Healthcare Programs method prevails.
How Payment is Calculated on Medicare Crossover Claims
When a member has coverage from both Montana Healthcare Programs and Medicare, Medicare is the primary payer as described in the Coordination of Benefits chapter of this manual. Montana Healthcare Programs then makes a payment as the secondary payer. For the provider types covered in this manual, Montana Healthcare Programs’s payment is calculated so that the total payment to the provider is either the Montana Healthcare Programs allowed amount less the Medicare paid amount or the sum of the Medicare coinsurance and deductible, whichever is lower. This method is sometimes called “lower of” pricing.
Other Factors That May Affect Payment
When Montana Healthcare Programs payment differs from the fee schedule, consider the following:
- The Department pays the lower of the established Montana Healthcare Programs fee or the provider’s charge
- The member may have an incurment amount that must be met before Montana Healthcare Programs will pay for services (see the General Information for Providers manual, member Eligibility and Responsibilities chapter, Coverage for the Medically Needy section.
- Date of service; fees for services may change over time.
- Medicare, incurment, and/or TPL payments, which are shown on the remittance advice.
End of How Payment Is Calculated Chapter
Appendix A: Forms
For the forms listed below and others, see the Forms page on the Provider Information website.
- Montana Healthcare Programs Medicaid/MHSP/HMK Individual Adjustment Request
- Paperwork Attachment Cover Sheet
End of Appendix A: Forms Chapter
Definitions and Acronyms
End of Definitions and Acronyms Chapter
Index
Previous editions of this manual contained an index.
This edition has three search options.
1.Search the whole manual. Open the Complete Manual pane. From your keyboard press the Ctrl and F keys at the same time. A search box will appear. Type in a descriptive or key word (for example "Denials". The search box will show all locations where denials discussed in the manual.
2.Search by Chapter. Open any Chapter tab (for example the "Billing Procedures" tab). From your keyboard press the Ctrl and F keys at the same time. A search box will appear. Type in a descriptive or key word (for example "Denials". The search box will show where denials discussed in just that chapter.
End of Index Chapter
End of Nutrition Manual