Hospital Inpatient Services Manual
Printing the manual material found at this website for long-term use is not advisable. Department Policy material is updated periodically and it is the responsibility of the users to check and make sure that the policy they are researching or applying has the correct effective date for their circumstances.
If you experience any difficulty opening a section or link from this page, please email the webmaster.
How to Search this manual:
This edition has three search options.
- Search the whole manual. Open the Complete Manual pane. From your keyboard press the Ctrl and F keys at the same time. A search box will appear. Type in a descriptive or key word (for example "Denials". The search box will show all locations where denials discussed in the manual.
- Search by Chapter. Open any Chapter tab (for example the "Billing Procedures" tab). From your keyboard press the Ctrl and F keys at the same time. A search box will appear. Type in a descriptive or key word (for example "Denials". The search box will show where denials discussed in just that chapter.
- Site Search. Search the manual as well as other documents related to a particular search term on the Montana Healthcare Programs Site Specific Search page.
Prior manuals may be located through the provider website archives.
Updated 07/01/2020
Hospital Inpatient Services Manual
To print this manual, right click your mouse and choose "print". Printing the manual material found at this website for long-term use is not advisable. Department Policy material is updated periodically and it is the responsibility of the users to check and make sure that the policy they are researching or applying has the correct effective date for their circumstances.
Update Log
Publication History
This publication supersedes all previous Hospital Inpatient Services handbooks. Published by the Montana Department of Public Health & Human Services, January 2005.
Updated October 2017, June 2018, January 2020, and July 2020.
CPT codes, descriptions and other data only are copyright 2014 American Medical Association (or such other date of publication of CPT). All Rights reserved. Applicable FARS/DFARS Apply.
Update Log
07/01/2020
A duplicate line was removed from the Billings Procedure chapter.
01/01/2020
Cost Share references removed from Billing Procedures, Submitting A Claim, and How Payments Is Calculated Chapters.
Term "Medicaid" replaced with "Montana Healthcare Programs" throughout the manual.
06/05/2018
Definitions and the How Payment is Calculated chapters were revised.
10/16/2017
Hospital Inpatient Services Manual converted to an HTML format and adapted to 508 Accessibility Standards.
End Update Log Chapter
Table of Contents
Key Contacts
Introduction
Manual Organization
Manual Maintenance
Rule References
Claims Review (MCA 53-6-111, ARM 37.85.406)
Getting Questions Answered
Covered Services
General Coverage Principles
- Hospital Inpatient Services (ARM 37.86.2801–2950)
- Services for Children (ARM 37.86.2201-2235)
- Importance of Fee Schedules
Physician Attestation and Acknowledgement (ARM 37.86.2904)
Utilization Reviews (42 CFR 456)
Obtaining Resident Status (ARM 37.86.2921)
Nursing Facility Placement (ARM 37.40.202)
Coverage of Specific Services
- Elective Deliveries
- Clinical Trials (ARM 37.86.2902)
- Inpatient Hospital Services
- Abortions (ARM 37.86.104)
- Air Transports
- Chemical Dependency Treatment
- Discharges
- Donor Transplants
- Emergency Department Admissions
- Mental Health Services
- Observation Bed
- Out-of-State Inpatient Services (ARM 37.86.2801)
- Readmissions (ARM 37.86.2918)
- Same Day Readmission
- Sterilization/Hysterectomy (ARM 37.86.104)
- Transfers (ARM 37.86.2918)
- Transplants (ARM 37.86.4701 and ARM 37.86.2902)
Non-Covered Services (ARM 37.85.207 and ARM 37.86.2902)
Prior Authorization
What is Prior Authorization (ARM 37.86.2801)
Billing Procedures
Claim Forms
Hospital Services Beyond Medical Necessity
Member Cost Sharing (ARM 37.83.825. 37.85.402)
Medicare Benefits Exhausted
Services Provided to Passport to Health Members
Services That Require Prior Authorization
Discharges and Transfers
Bundled Services
Unbundled Services (ARM 37.86.2905(5))
Split/Interim Billing
- Partial Eligibility
- Incurment
Billing for Abortions and Sterilizations
- Abortions
- Sterilizations
Billing Unlisted Services or Procedures
Billing Electronically with Paper Attachments
Submitting a Claim
Paper Claims
Present on Admission
How Payment Is Calculated
Overview
The Inpatient Prospective Payment System (PPS)
The Inpatient Prospective Payment Method Using All Patient Refined Diagnosis Related Groups (APR-DRG)
Ungroupable DRG
Relative Weights and Reimbursement Data
- APR-DRG Relative Weights
- DRG Base Price
- APR-DRG Base Payment
Computational Formulas and Definitions
Payment Factors
- Capital Related Costs
- Cost Outlier Payments
- Transfer Payment Adjustments
- Prorated Payment Adjustment
- The Cost-Based Payment Method for Exempt Hospitals and Services
- Exempt Services and Costs
- Reasonable Cost Reimbursement
Hospital Residents
How Payment Is Calculated on TPL Claims
How Payment Is Calculated on Medicare Crossover Claims
Payment Examples for Dually Eligible Members
Disproportionate Share Hospital (DSH) Payments (ARM 37.86.2925)
Appendix A: Forms
Definitions and Acronyms
Index/How To Search This Manual
End of Table of Contents Chapter
Key Contacts
Hours for Key Contacts are 8 a.m. to 5 p.m. Monday through Friday (Mountain Time), unless otherwise stated. The phone numbers designated only “In state” will not work outside Montana. For additional contacts and websites, see the Contact Us link in the left menu on the Provider Information website.
CLIA Certification
For questions regarding CLIA certification, call or write:
(406) 444-1451 Phone
(406) -444-3456 Fax
Quality Assurance Division
Certification Bureau
DPHHS
2401 Colonial Drive
P.O. Box 202953
Helena, MT 59620-2953
Hospital Program
To qualify a member for residency status or to submit claims for hospital residents:
(406) 444-7018 Phone
(406) 444-4441 Fax
Hospital Program Officer
Health Resources Division
P.O. Box 202951
Helena, MT 59620
Lab
Public Health Lab assistance:
(800) 821-7284 In state
(406) 444-3444 Helena/Out of state
DPHHS Public Health Lab
1400 Broadway
P.O. Box 6489
Helena, MT 59620
Nursing Facility/Swing Bed Pre-Admission Screening
For Level I screening and Level of Care (LOC) screening for members entering a nursing facility or swing bed hospital, contact:
(800) 219-7035 Phone In/Out of state
(406) 443-0320 Phone Helena
(800) 413-3890 Fax In/Out of state
(406) 513-1921 Fax Helena
Mountain-Pacific Quality Health
3404 Cooney Drive
Helena, MT 59602
End Key Contacts Chapter
Introduction
Thank you for your willingness to serve members of the Montana Healthcare Programs and other medical assistance programs administered by the Department of Public Health and Human Services.
Manual Organization
This manual provides information specifically for hospital inpatient services. Other essential information for providers is contained in the separate General Information for Providers manual. Providers are responsible for reviewing both manuals.
A table of contents and an index allow you to quickly find answers to most questions. The margins contain important notes with extra space for writing notes. There is a list of contacts at the beginning of each manual. There is also space on the inside of the front cover to record your NPI for quick reference when calling Provider Relations.
Manual Maintenance
Manuals must be kept current. Changes to manuals are provided through provider notices and replacement pages. Manual replacement pages can be downloaded from the provider type pages on the Provider Information website and are identified by a note at the top of the page indicating Replacement Page and the date. They are designed to be printed on the front and back of each page, so they are always in sets of two beginning with an odd page followed by an even page, even though one of the pages may not have any changes. When replacing a page in a paper manual, file the old pages and provider notices in the back of the manual for use with claims that originated under the old policy.
Rules References
Providers must be familiar with all current rules and regulations governing the Montana Healthcare Programs. Provider manuals are to assist providers in billing Montana Healthcare Programs; they do not contain all Montana Healthcare Programs rules and regulations. Rule citations in the text are a reference tool; they are not a summary of the entire rule. In the event that a manual conflicts with a rule, the rule prevails. Links to rules are available on the Provider Information website. Paper copies of rules are available through the Secretary of State’s office. See the Contact Us link in the left menu on the Provider Information website.
Providers are responsible for knowing and following current Montana Healthcare Programs rules and regulations.
In addition to the general Montana Healthcare Programs rules outlined in the General Information for Providers manual, the following rules and regulations are also applicable to the hospital inpatient program:
- Code of Federal Regulations (CFR)
- 42 CFR 440.10, Inpatient Hospital Services, Other Than Services in an Institution for Mental Disease
- Montana Codes Annotated (MCA)
- MCA Title 50-5-101–50-5-1205, Hospitals and Related Facilities
- Administrative Rules of Montana (ARM)
- ARM Title 37.86.2801–37.86.2950, Inpatient Hospital Services
Claims Review (MCA 53-6-111 and ARM 37.85.406)
The Department is committed to paying Montana Healthcare Programs providers’ claims as quickly as possible. Montana Healthcare Programs claims are electronically processed and usually are not reviewed by medical experts prior to payment to determine if the services provided were appropriately billed. Although the computerized system can detect and deny some erroneous claims, there are many erroneous claims it cannot detect. For this reason, payment of a claim does not mean the service was correctly billed or the payment made to the provider was correct. Periodic retrospective reviews are performed that may lead to the discovery of incorrect billing or incorrect payment. If a claim is paid and the Department later discovers the service was incorrectly billed or paid or the claim was erroneous in some other way, the Department is required by federal regulation to recover any overpayment, regardless of whether the incorrect payment was the result of Department or provider error or other cause.
Getting Questions Answered
The provider manuals are designed to answer most questions; however, questions may arise that require a call to a specific group (such as a program officer, Provider Relations, or a prior authorization unit). A list of key contacts and websites is available online. On the Provider Information website, choose the Contact Us link in the left menu. Providers should also read the monthly Claim Jumper newsletter for Montana Healthcare Programs updates and changes. Montana Healthcare Programs provider manuals, provider notices, replacement pages, fee schedules, forms, and more are available on the Provider Information website.
End of Introduction Chapter
Covered Services
General Coverage Principles
Montana Healthcare Programs covers inpatient hospital services when they are medically necessary. This chapter provides covered services information that applies specifically to inpatient hospital services. Like all healthcare services received by Montana Healthcare Programs members, these services must also meet the general requirements listed in the Provider Requirements chapter of the General Information for Providers manual.
Hospital Inpatient Services (ARM 37.86.2801–2950)
Inpatient hospital services are provided to Montana Healthcare Programs members who are formally admitted as an inpatient and whose expected hospital stay is greater than 24 hours. Inpatient services must be ordered by a licensed physician or dentist and provided in an institution maintained primarily for treatment and care of patients with disorders other than tuberculosis or mental diseases. The institution must be currently licensed by the designated state licensing authority in the state where the institution is located, must meet the requirements for participation in Medicare as a hospital, and must have in effect a utilization review plan that meets the requirements of 42 CFR 482.30.
Services for Children (ARM 37.86.2201–2235)
The Early and Periodic Screening, Diagnostic, and Treatment (EPSDT) Services program is a comprehensive approach to healthcare for Montana Healthcare Programs members ages 20 and under. It is designed to prevent, identify, and then treat health problems before they become disabling. Under EPSDT, Montana Healthcare Programs eligible children may receive any medically necessary covered service, including all inpatient hospital services described in this manual. All applicable Passport to Health and prior authorization requirements apply.
Importance of Fee Schedules
The easiest way to verify coverage for a specific service is to check the Department’s fee schedule for your provider type. In addition to being listed on the fee schedule, all services provided must also meet the coverage criteria listed in the Provider Requirements chapter of the General Information for Providers manual and in this chapter. Use the fee schedule in conjunction with the more detailed coding descriptions listed in the current ICD coding book. Take care to use the fee schedule and coding books that pertain to the date of service. Fee schedules are available on the Provider Information website.
Physician Attestation and Acknowledgment (ARM 37.86.2904)
At the time a claim is submitted, the hospital must have on file a signed and dated acknowledgment from the attending physician that the physician has received the following notice:
Notice to physicians: Montana Healthcare Programs payment to hospitals is based on all of each patient’s diagnoses and the procedures performed on the patient, as attested to by the patient's attending physician by virtue of his or her signature in the medical record. Anyone who misrepresents, falsifies or conceals essential information required for payment of federal funds, may be subject to fine, imprisonment or civil penalty under applicable federal laws.
The acknowledgement must be completed by the physician at the time that the physician is granted admitting privileges at the hospital, or before or at the time the physician admits his/her first member to the hospital. Existing acknowledgments signed by physicians already on staff remain in effect as long as the physician has admitting privileges at the hospital. The provider may, at its discretion, add to the language of this statement the word Medicare so that two separate forms will not be required by the provider to comply with state and federal requirements.
Utilization Reviews (42 CFR 456)
The Department or its contractor may at any time review paid claims, provider documentation for medical necessity, appropriate billing, etc. Providers must maintain documentation of medical necessity for services such as initial hospitalization, transfers, and readmissions. For more information on provider requirements for maintaining documentation, see the Record Keeping section in the Provider Requirements chapter of the General Information for Providers manual. Also see the Claims Review section in the Introduction chapter of this manual.
Obtaining Resident Status (ARM 37.86.2921)
Providers must contact the Department to obtain hospital residence status prior to billing Montana Healthcare Programs. To qualify for residency status, a member must meet the following requirements:
- Use a ventilator for a continuous period of not less than 8 hours in a 24-hour period or require at least 10 hours of direct nursing care in a 24-hour period.
- Must have been an inpatient in an acute care hospital for a minimum of 6 continuous months within the requesting facility.
It is the provider’s responsibility to determine whether services could be provided in a skilled nursing care facility or by the Home and Community-Based Waiver Program. The provider must maintain written records of inquiries and responses about the present and future availability of openings in nursing facilities and the Home and Community-Based Waiver Program. A redetermination of nursing facility or waiver availability must be made at least every 6 months.
Nursing Facility Placement (ARM 37.40.202)
Hospitalized Montana Healthcare Programs members and Montana Healthcare Programs applicants being considered for nursing facility placement from the hospital shall be referred in a timely manner to the preadmission screening team. The preadmission screening form (Form DPHHS-SLTC-61) must be completed before placement and payment is made on their behalf.
Coverage of Specific Services
Elective Deliveries
Effective July 1, 2014, all facilities must have a hard-stop policy in place regarding non-medically necessary inductions prior to 39 weeks and nonmedically necessary Cesarean sections at any gestational age. The policy must contain the following:
- No non-medically necessary inductions and Cesarean sections prior to39 weeks and 0/7 days gestation, and no non-medically necessary Cesarean sections at any gestational age.
- Confirmation of weeks gestation by ACOG guidelines (at least one of the following guidelines must be met to show gestational age):
- Fetal heart tones have been documented for 20 weeks by non-electronic fetoscope or 30 weeks by Doppler;
- 36 weeks since a positive serum or urine pregnancy test that was performed by a reliable laboratory; or
- An ultrasound prior to 20 weeks that confirms the gestational age of at least 39 weeks.
- If pregnancy care was not initiated prior to 20 weeks gestation, the gestational age may be documented from first day of the last menstrual period (LMP).
- Policy must have a multistep review process prior to all inductions and Cesarean Sections including final decision being made by the Perinatology Chair/Obstetrical Chair, OB Director, or Medical Director.
Effective October 1, 2014, Montana Healthcare Programs will reduce reimbursement rates for non-medically necessary inductions prior to 39 weeks, and non-medically necessary Cesarean sections at any gestational ages. All hospital claims with an admit date on or after October 1, 2014, will require coding changes to delivery claims.
Hospital inpatient claims and birthing center claims will require the use of condition codes for all induction and Cesarean section deliveries. These claims will be reviewed for medical necessity based on an approved list of diagnosis codes. The condition codes are:
- 81 − Cesarean section or induction performed at less than 39 weeks gestation for medical necessity.
- 82 − Cesarean section or induction performed at less than 39 weeks gestation elective.
- 83 − Cesarean section or induction performed at 39 weeks gestation or greater.
Clinical Trials (ARM 37.86.2902)
Clinical trial drugs, devices, and procedures are not reimbursable. Clinical trials are limited to Montana Healthcare Programs coverage of routine costs plus reasonable and necessary items and services used to diagnose and treat complications arising from participation in all qualifying clinical trials. Qualifying clinical trials include those that are directly funded or supported by centers or cooperating groups funded by the National Institutes of Health (NIH), Centers for Disease Control (CDC), Agency for Healthcare Research and Quality (AHRQ), Department of Defense (DOD), or Veterans Affairs (VA).
Inpatient Hospital Services
The following are coverage rules for specific inpatient hospital services. Inpatient hospital services included in the All Patient Refined Diagnosis-Related Group (APR-DRG) payment methodology include all routine services such as the following:
- Bed and board
- Nursing services and other related services
- Use of hospital facilities
- Medical social services
- Drugs, biologicals, supplies, appliances, and equipment furnished by the hospital for the care and treatment of inpatients
- Other diagnostic or therapeutic items or services provided in the hospital that are not specifically excluded (ARM 37.85.207). See the Non-Covered Services section in this chapter.
- Outpatient services provided by the hospital facility the day of admission or the day before.
Abortions (ARM 37.86.104)
Abortions are covered when one of the following conditions are met:
- The member’s life would be endangered if the fetus is carried to term.
- The pregnancy is the result of rape or incest.
- The abortion is determined by the attending physician to be medically necessary, even if the member’s life is not endangered if the fetus is carried to term.
A completed Montana Healthcare Programs Physician Certification for Abortion Services (MA-37) form must be submitted with every abortion claim or payment will be denied. Complete only one section of this form. This form is the only form Montana Healthcare Programs accepts for abortion services.
When using mifepristone (Mifeprex or RU 486) to terminate a pregnancy, it must be administered within 49 days from the beginning of the last menstrual period by or under the supervision of a physician who:
- Can assess the duration of a pregnancy.
- Can diagnose ectopic pregnancies.
- Can provide surgical intervention in cases of incomplete abortion or severe bleeding, or can provide such care through other qualified physicians.
- Can assure access to medical facilities equipped to provide blood transfusion and resuscitation.
- Has read, understood, and explained to the member the prescribing information for mifepristone.
Air Transports
Air transport providers must be registered with Montana Healthcare Programs as an ambulance provider. Claims for these services are billed on a CMS-1500 claim form. See the Ambulance Services manual available on the Provider Information website.
Chemical Dependency Treatment
Chemical dependency services are limited. Providers must be approved by the Department before providing this service. Contact the Chemical Dependency Bureau for information. (See the Contact Us link on the Provider Information website.)
Discharges
A hospital’s utilization review (UR) committee must comply with the Code of Federal Regulations 42 CFR 456.131 through 42 CFR 456.137 prior to notifying a Montana Healthcare Programs member that he/she no longer needs medical care. The hospital is not required to obtain approval from Montana Healthcare Programs at the member’s discharge; however, a hospital’s UR plan must provide written notice to Montana Healthcare Programs if a member decides to stay in the hospital when it is not medically necessary. (See the Hospital Services Beyond Medical Necessity section in the Billing Procedures chapter of this manual.)
Donor Transplants
Montana Healthcare Programs covers successful donor-related testing and services and organ acquisition services, which are bundled into the Montana Healthcare Programs member’s transplant hospitalization, and are covered in this APR-DRG payment.
Emergency Department Admissions
Emergency medical services are those services required to evaluate, treat and stabilize an emergency medical condition.
Mental Health Services
Montana Healthcare Programs covers inpatient mental health services for Montana Healthcare Programs-enrolled members when prior authorized. (See the Prior Authorization chapter in this manual. and refer to the mental health manual available on the Provider Information website.)
Observation Bed
Members in observation beds (admission of 72 hours or less) are considered outpatients and claims should be filed accordingly. (See the Hospital Outpatient Services manual available on the Provider Information website.)
Out-of-State Inpatient Services (ARM 37.86.2801)
Montana Healthcare Programs covers treatment in an out-of-state facility only when all of the following requirements are met:
- The member cannot be treated in state, and the provider contacts the prior authorization designated review organization to determine if services are available in Montana before considering placement in an out-of-state facility.
- The provider received prior authorization for out-of-state services before the member is sent to an out-of-state hospital. See the Prior Authorization chapter in this manual for more information.
It is not the intent of the Montana Healthcare Programs to interfere or delay a transfer when a physician has determined a situation to be emergent. Prior authorization is not required in emergency situations. Emergency inpatient admissions must be authorized within 2 working days (Monday–Friday) of admission to an out-of-state hospital.
If a hospital that is located over 100 miles outside of the borders of Montana or a Center for Excellence hospital fails to obtain prior authorization before providing services to a Montana Healthcare Programs member, retrospective authorization may be granted under the following circumstances only: The person to whom services were provided was determined by the Department to be retrospectively eligible for Montana Healthcare Programs benefits;
- The hospital can document that the admission was an emergency admit for the purpose of stabilization or stabilization for transfer;
- The hospital must call for authorization within three working days (Monday-Friday) of the admission or knowledge of the member’s Montana Healthcare Programs eligibility;
- Interim claims equal to or greater than 30 days of continuous inpatient services at the same facility; or
- The hospital is retroactively enrolled as a Montana Healthcare Programs provider, and the enrollment includes the dates of service for which authorization is requested; provided the hospital’s retroactive enrollment is completed, allowing time for the hospital to obtain prior authorization and to submit a clean claim within timely filing deadlines in accordance with ARM 37.85.406.
Readmissions (ARM 37.86.2918)
All readmissions are subject to review for medical necessity of the initial stay as well as the subsequent hospitalization stay. Reimbursement cannot be made to a provider unless the service provided was medically necessary. Readmission may be reviewed on a retrospective basis to determine if additional payment for the case is warranted. If complications have arisen because of premature discharge and/or other treatment errors, then the APR-DRG payment for the first admission must be combined with the current admission before billing Montana Healthcare Programs. If the readmission is for the treatment of conditions that could or should have been treated during the previous admission, the two admissions must be combined into one admission for payment purposes.
A member readmission occurring in an inpatient rehabilitation hospital or distinct part unit three days after the initial date of discharge must be combined into one admission for payment purposes, with the exception of discharge to an acute care hospital for surgical APR-DRGs. Inpatient readmissions within 24 hours must be combined if the same condition is coded.
Same Day Readmission
If a member is readmitted on the same day of discharge for the same condition, the entire stay must be billed as one admission.
If a member is readmitted on the same day of discharge for a separate condition, Montana Healthcare Programs may be billed for the new condition. The claim for the new condition and a letter of explanation including documentation for the separate condition must be sent directly to the Hospital Program Officer for review.
A member readmission occurring in an inpatient rehabilitation hospital or distinct part unit three days after the initial date of discharge must be combined into one admission for payment purposes, with the exception of discharge to an acute care hospital for surgical APR-DRGs. Inpatient readmissions within 24 hours must be combined if the same condition is coded.
Sterilization (ARM 37.86.104)
Elective Sterilization
Elective sterilizations are sterilizations done for the purpose of becoming sterile. Montana Healthcare Programs covers elective sterilization for men and women when all of the following requirements are met:
- Member must complete and sign the Informed Consent to Sterilization (MA-38) form at least 30 days, but not more than 180 days, prior to the sterilization procedure. This form is the only form Montana Healthcare Programs accepts for elective sterilizations. If this form is not properly completed, payment will be denied. See the Forms page on the Provider Information website for the form and instructions for completing.
- Member must be at least 21 years of age when signing the form.
- Member must not have been declared mentally incompetent by a federal, state, or local court, unless the member has been declared competent to specifically consent to sterilization.
- Member must not be confined under civil or criminal status in a correctional or rehabilitative facility, including a psychiatric hospital or other correctional facility for the treatment of the mentally ill.
The 30-day waiting period may be waived for either of the following reasons:
- Premature Delivery. The Informed Consent to Sterilization must be completed and signed by the member at least 30 days prior to the estimated delivery date and at least 72 hours prior to the sterilization.
- Emergency Abdominal Surgery. The Informed Consent to Sterilization form must be completed and signed by the member at least 72 hours prior to the sterilization procedure.
All forms required for sterilizations can be downloaded from the Provider Information website,
Before performing a sterilization, the following requirements must be met:
- The member must have the opportunity to have questions regarding the sterilization procedure answered to his/her satisfaction.
- The member must be informed of his/her right to withdraw or withhold consent any time before the sterilization without being subject to retribution or loss of benefits.
- The member must be made aware of available alternatives of birth control and family planning.
- The member must understand the sterilization procedure being considered is irreversible.
- The member must be made aware of the discomforts and risks which may accompany the sterilization procedure being considered.
- The member must be informed of the benefits and advantages of the sterilization procedure.
- The member must know that he/she must have at least 30 days to reconsider his/her decision to be sterilized.
- An interpreter must be present and sign for those members who are blind, deaf, or do not understand the language to assure the person has been informed.
Informed consent for sterilization may not be obtained under the following circumstances:
- If the member is in labor or childbirth.
- If the member is seeking or obtaining an abortion.
- If the member is under the influence of alcohol or other substance which affects his/her awareness.
Medically Necessary Sterilization
When sterilization results from a procedure performed to address another medical problem, it is considered a medically necessary sterilization. These procedures include hysterectomies, oophorectomies, salpingectomies and orchiectomies. Every claim submitted to Montana Healthcare Programs for a medically necessary sterilization must be accompanied by one of the following:
- A completed Montana Healthcare Programs Hysterectomy Acknowledgement form (MA-39). It is the provider’s responsibility to obtain a copy of the form from the primary or attending physician. Complete only one section of this form. When no prior sterility (Section B) or no life-threatening emergency (Section C) exists, the member and physician must sign and date Section A of this form prior to the procedure. (See 42 CFR 441.250 for the federal policy on hysterectomies and sterilizations). Also, for Section A, signatures dated after the surgery date require manual review of medical records by the Department. The Department must verify that the member (and representative, if any) was informed orally and in writing, prior to the surgery, that the procedure would render the member permanently incapable of reproducing. The member does not need to sign this form when Sections B or C are used.
- For members who have become retroactively eligible for Montana Healthcare Programs, the physician must certify in writing that the surgery was performed for medical reasons and must document one of the following:
- The individual was informed prior to the hysterectomy that the operation would render them permanently incapable of reproducing.
- The reason for the hysterectomy was a life-threatening emergency.
- The member was already sterile at the time of the hysterectomy and the reason for prior sterility.
When submitting claims for retroactively eligible members, attach a copy of the 160-M to the claim if the date of service is more than 12 months earlier than the date the claim is submitted.
Transfers (ARM 37.86.2918)
All diagnostic services are included in the APR-DRG payment. Diagnostic services that are performed at a second APR-DRG hospital, because the services are not available at the first hospital (e.g., a CT scan), are included in the first hospital’s APR-DRG payment. This includes transportation to the second hospital and back to the first hospital. Arrangement for payment to the transportation provider and the second hospital where the services were actually performed must be between the first and second hospital and the transportation provider.
All transfers are subject to review for medical necessity. The initial hospitalization, all subsequent hospitalizations, and the medical necessity for the transfer itself may be reviewed. For information on billing and payment for transfers, see this manual’s Billing Procedures and How Payment Is Calculated chapters.
Transplants (ARM 37.86.4701–ARM 37.86.4706)
Montana Healthcare Programs covers organ and tissue transplants that are medically necessary and not considered experimental or investigational. Organ transplants must be performed in a Medicare-certified facility. If Medicare has not designated a facility as being certified, the transplant must be performed by a program located in a hospital or parts of a hospital certified by the Organ Procurement and Transplantation Network (OPTN) for the specific organ being transplanted. A list of CMS-certified facilities is on the CMS website at http://www.cms.hhs.gov. (Search for transplant program certification.)
Organ and tissue transplantation includes the transplant surgery and those activities directly related to the transplantation. These activities may include:
- Evaluation of the member as a potential transplant candidate
- Pre-transplant preparation including histo-compatibility testing procedures
- Post-surgical hospitalization
- Outpatient care, including Federal Drug Administration (FDA) approved medications deemed necessary for maintenance or because of resulting complications
- Associated medical expenses for the successful donor only. (These will be bundled into the Montana Healthcare Programs member’s inpatient transplant hospitalization.)
These activities are covered by Montana Healthcare Programs as long as the member remains Montana Healthcare Programs-eligible and transplantation is prior approved. Services must comply with Medicare coverage guidelines for organ and tissue transplant services. If Medicare coverage guidelines are not available, the Department or their designated review organization will review the requested transplant surgery to determine if the surgery is experimental or investigational.
Non-Covered Services (ARM 37.85.207 and ARM 37.86.2902)
The following medical and nonmedical services, except as otherwise specified in program-specific rules as a waiver service or an EPSDT service, are explicitly excluded from the Montana Healthcare Programs, except for those services specifically available, as listed in ARM 37.40.1406, 37.90.402, and Title 37, Chapter 34, Subchapter 9, to persons eligible for home and community-based services; and except for those Medicare-covered services as listed in ARM 37.83.812 to qualified Medicare beneficiaries for whom the Montana Healthcare Programs pays the
Medicare premiums, deductible, and coinsurance.
- Acupuncture
- Autopsies
- Bariatric services and surgery-related services (including bypass and revisions)
- Chiropractic services
- Circumcisions not authorized by the Department as medically necessary
- Delivery services not provided in a licensed healthcare facility or nationally accredited birthing center unless as an emergency service
- Dietary supplements
- Dietician services (some services covered per ARM 37.86.3002)
- Donor search expenses
- Erectile dysfunction products, including but not limited to injections, devices, and oral medications used to treat impotence
- Experimental services, services that do not comply with national standards of medical practice, non-FDA-approved drugs, biologicals and devices, and clinical trials are excluded from coverage.
- Experimental services or services that are generally regarded by the medical profession as unacceptable treatment not medically necessary for the purposes of the Montana Healthcare Programs.
- Homemaker services
- Infertility treatment services, including sterilization reversals
- Masseur/Masseuse services
- Medical services furnished to Montana Healthcare Programs-eligible members who are absent from the state including a child residing in another state for whom Montana makes adoption assistance or foster care maintenance payments are covered as in each program-specific rule and subject to the applicable conditions of those rules.
- Naturopathic services
- Nutritional services
- Physical therapy aide services
- Services that are not directly related to patient care including, but not limited to, car repair and/or modification of automobile, mileage for travel expenses for providers, missed or canceled appointments, plumbing service, preparation of medical or insurance reports, remodeling of home, service charges or delinquent payment fees, telephone services in the home).
- Services that are not medically necessary. The Department may review for medical necessity at any time before or after payment. The Montana Healthcare Programs member is financially responsible for these services if the member agrees in writing before the services are provided. See the When to Bill Montana Healthcare Programs Members section in the Billing Procedures chapter of the General Information for Providers manual
- Sexual aids including, but not limited to, devices, injections and oral medications
- Surgical technician services (technicians who are not physicians or mid-level practitioners)
End of Covered Services Chapter
Prior Authorization
What is Prior Authorization (ARM 37.86.2801)
Prior authorization is the approval process required before certain services are paid by Montana Healthcare Programs. If a service requires prior authorization, the requirement exists for all Montana Healthcare Programs members. When prior authorization is granted, the provider is issued a prior authorization number, which must be on the claim.
Distinct authorization numbers are issued for Passport approval and prior authorization, and both must be recorded on the claim in the appropriate location.
Prior authorization is not a guarantee of payment. When requesting prior authorization, keep in mind the following:
- The referring provider should initiate all authorization requests.
- For members with partial eligibility, request prior authorization from the first date the member was Montana Healthcare Programs-eligible, not from the first date of the member’s hospital stay.
- Have all required documentation included in the packet before submitting a request for prior authorization. The Prior Authorization Information link on the Provider Information website lists some services that require prior authorization, who to contact, and specific documentation requirements. Also refer to the fee schedules.
- Prior authorization must be obtained before a member receives services. See the fee schedules for procedure codes that have Y as the prior authorization indicator. Prior authorization is also required for:
- All psych inpatient services except if patient has Medicare.
- All out-of-state inpatient services except if the patient has Medicare and the only reason for prior authorization is for out-of-state services.
- Interim claims for Prospective Payment System (PPS).
Montana Healthcare Programs does not pay for services when prior authorization or Passport requirements are not met.
- When prior authorization is granted, providers receive notification containing a prior authorization number, which must be included on the claim.
Prior authorization is not required in emergency situations.
It is not the intent of the Montana Healthcare Program to interfere or delay a transfer when a physician has determined a situation to be emergent. Prior authorization is not required in emergency situations. Emergency inpatient admissions must be authorized within three working days (Monday–Friday) of admission to an out-of-state hospital.
Retrospective authorization may be granted only under the following circumstances:
- The Montana Healthcare Programs member qualifies for retroactive eligibility for Montana Healthcare Programs hospital benefits.
- The hospital is retroactively enrolled as a Montana Healthcare Programs provider during the dates of service for which authorization is requested.
- The hospital can document that at the time of admission it did not know, or have any basis to assume that the member was a Montana Healthcare Programs member.
For more information, see the Prior Authorization chapter in the General Information for Providers manual, fee schedules, and the Prior Authorization Information page on the Provider Information website.
End of Prior Authorization Chapter
Billing Procedures
Claim Forms
Services provided by the healthcare professionals covered in this manual must be billed either electronically or on UB-04 claim forms, which are available from various publishing companies; they are not available from the Department or Provider Relations.
Hospital Services Beyond Medical Necessity
The Montana Healthcare Programs member who chooses to remain in the hospital beyond the period of medical necessity may choose to pay for continued inpatient care as a Montana Healthcare Programs noncovered service. The member must have been informed in writing and agreed in writing prior to provision of services to accept financial responsibility. The agreement must state the specific services the Montana Healthcare Programs member has agreed to pay for. In this case, a routine agreement will not suffice. Montana Healthcare Programs may not be billed for hospital services that are not medically necessary.
A hospital’s utilization review plan must provide written notice to Montana Healthcare Programs if a Montana Healthcare Programs member decides to stay in the hospital when it is not medically necessary. This written notice must be sent to the hospital program officer. (See Key Contacts in this manual or the Contact Us link in the left menu on the Provider Information website.)
Member Co-Payment (ARM 37.83.825 and 37.83.826)
Effective for all claims paid on or after January 1, 2020 copayment will not be assessed.
Medicare Benefits Exhausted
Medicare crossovers are claims for hospital patients who are eligible for Medicare Part A benefits and Montana Healthcare Programs. For these members, Montana Healthcare Programs pays the deductibles and coinsurance related to the inpatient hospital services. Should a Medicare/Montana Healthcare Programs member exhaust the Medicare benefit (including Lifetime Reserve Days), the claim will be treated as a Montana Healthcare Programs-only claim from the date the Medicare benefits were exhausted. The claim should be submitted reflecting a covered stay from the day the Medicare benefits were exhausted to discharge. This situation is the only instance in which a hospital should submit a split bill for a case that will be paid using prospective payment principles.
Services Provided to Passport to Health Members
A Montana Healthcare Programs member covered by the Passport to Health program must have inpatient hospital services approved by the member’s primary care provider (PCP). The Passport provider number must be on the claim or the service will be denied.
Services That Require Prior Authorization
Prior authorization is required for some hospital services. Passport and prior authorization are different, and some services may require both. See the Passport chapter in the General Information for Providers manual and/or the Prior Authorization chapter in this manual and the Prior Authorization Information page of the Provider Information website. Different codes are issued for each type of approval and must be included on the claim form, or the claim will be denied. See the Submitting a Claim chapter in this manual.
Discharges and Transfers
Claims can be filed only after the member has been discharged. A member is considered discharged when he or she is:
- Formally released from the hospital
- Transferred to another hospital or rehabilitation unit
- Dies in the hospital
- Leaves the hospital against medical advice (AMA)
- Discharge to hospice
- Transferred to a LTCF, SNF, ICF, or swing bed
The hospital that ultimately discharges the member bills Montana Healthcare Programs. When a member is transferred from one hospital to another for services the first hospital does not provide (e.g., CT scan) and then back to the first hospital, all diagnostic services are included in the APR-DRG payment to the first hospital. Also included in the same payment are the services that were provided at the second hospital and transportation to the second hospital and back to the first hospital. Arrangement for payment to the transportation provider and the second hospital must be arranged between the first and second hospital and the transportation provider.
Providers must notify the Department when a member chooses to stay in the hospital when it is not medically necessary.
All transfers are subject to review for medical necessity. Initial hospitalizations, subsequent hospitalizations, and transfers may be reviewed for medical necessity. Reimbursement cannot be made to a provider unless the service provided was medically necessary.
The patient status code should contain the appropriate discharge status code. The following discharge status codes are valid for Montana Healthcare Programs.
Discharge Status Codes
01 Discharged to home or self-care (routine discharge)
02 Discharge/Transfer to another short-term general hospital for inpatient care
03 Discharge/Transfer to skilled nursing facility (SNF)
04 Discharge/Transfer to an intermediate care facility (ICF)
05 Discharge/Transfer to another type of institution for inpatient care
06 Discharge/Transfer to home under care of organized home health service organization
07 Left against medical advice or discontinued care
08 Discharge/Transfer to home under care of a Home IV provider
09 Admitted as an inpatient to this hospital 63 Discharge/Transfer to a long-term care hospital
20 Expired (death) 64 Discharge/Transfer to nursing facility certified under Montana Healthcare Programs, but not Medicare
30 Still a patient (Neonate providers discharge status code for interim billing.)
40 Expired (death) at home
41 Expired in a medical facility (e.g., hospital, SNF, ICF, or free standing hospice)
42 Expired – place unknown
43 Discharge/Transfer to Federal hospital
50 Hospice – home
51 Discharge/Transfer to hospice medical facility
61 Discharge/Transfer within this institution to hospital-based Medicare-approved swing bed
62 Discharge/Transfer to another rehabilitation facility including rehabilitation distinct part units of a hospital
63 Discharge/Transfer to a long-term care hospital
64 Discharge/Transfer to nursing facility certified under Montana Healthcare Programs, but not Medicare
65 Discharge/Transfer to a psychiatric hospital or psychiatric distinct part unit of a hospital
Bundled Services
Services that are included in the APR-DRG payment are considered bundled and include the following:
- Services provided on the day of admission or on the day preceding admission.
- All routine services. (See Coverage of Specific Services in the Covered Services chapter of this manual.)
- All diagnostic services (e.g., radiology). This includes diagnostic services that are performed at a second hospital because the services are not available at the first hospital (e.g., CT scan) as well as transportation between the two hospitals. See the Transfers section in this chapter.
- Donor/Harvesting.
- All ancillary services provided by the hospital or performed by another entity under contract with the hospital (e.g., hospital has a contractual agreement with an enrolled independent laboratory).
Always refer to the long descriptions in coding books.
Unbundled Services (ARM 37.86.2905(5))
Services that are not included in the APR-DRG payment and can be billed separately include the following:
- Dialysis: Effective October 1, 2008.
- Long-Acting Reversible Contraception (LARC): Effective January 1, 2015, Montana Healthcare Programs allows PPS hospitals to unbundle LARC devices (e.g., IUDs and contraceptive implants) and the insertion from the inpatient delivery claim. These services can be billed as an outpatient service on a 13X type of bill and will be paid at the OPPS rates. The following HCPCS/CPT codes are allowed:
- J7300 – Paragard, intrauterine copper contraceptive.
- J7301 – Skyla, levonorgestrel-releasing intrauterine contraceptive, 13.5 mg
- J7302 – Mirena, levonorgestrel-releasing intrauterine contraceptive, 52 mg
- J7307 – Implanon/Nexplanon, etonogestrel (contraceptive) implant system, including implant and supplies
- 11981 – Insertion of drug delivery implant
- 58300 – Insertion of intrauterine device
Split/Interim Billing
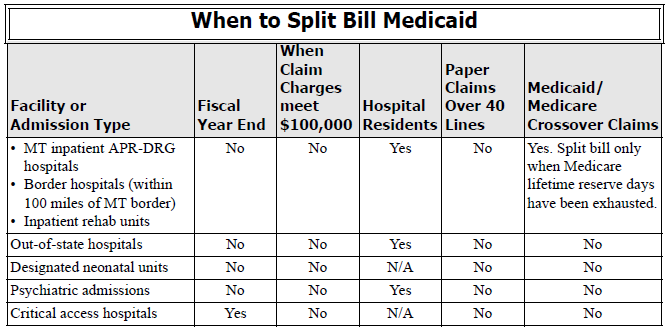
Some inpatient hospital services necessitate the use of split or interim bills for Montana Healthcare Programs reimbursement. In general, providers cannot split bill APR-DRG claims, except in a few cases:
- When Medicare lifetime reserve days have been exhausted, inpatient claims must be submitted to the Department for review. Documentation of exhaustion must be attached to the claim.
- For members classified as hospital residents. Claims for members approved and classified as hospital residents may be interim billed on a monthly basis after the first 180 days. These claims must be sent to the Department with a letter of explanation for manual pricing. The Department may approve the special billing and forward the claim to the claims processing contractor for processing with pricing instructions. Before billing for residents, the provider must obtain resident status for the member. (See Obtaining Resident Status in this manual’s Covered Services chapter.)
- Hospitals subject to the inpatient hospital prospective payment reimbursement method may only interim bill when the member has been a patient in the same facility at least 30 days, is Montana Healthcare Programs-eligible for a minimum of these 30 days, and has received prior authorization, in which case the hospital may bill every 30 days. Interim claims are paid by a per diem amount
multiplied by the number of covered Montana Healthcare Programs eligible days. Upon patient discharge, the interim claims will be voided or credited by the hospital and the hospital must bill a single admit through a discharge claim which will be paid by APR-DRG. - The Department will not accept late charges (Type of bill = 115). Instead, hospitals are instructed to adjust earlier claims if appropriate.
Partial Eligibility
APR-DRG hospitals do not split bill. Bill the entire claim from the date of admit, and the claim will be prorated during processing.
Incurment
All APR-DRG hospitals must bill from the date of admission. For more information on incurment, see the Member Eligibility and Responsibilities chapter in the General Information for Providers manual.
Billing for Abortions and Sterilizations
In order to be covered by Montana Healthcare Programs, abortions and sterilizations require specific forms to be completed and submitted with the claim. For more information on abortion and sterilization requirements, see the Covered Services chapter in this manual. Forms are available on the Provider Information website.
Abortions
A completed Montana Healthcare Programs Physician Certification for Abortion Services (MA-37) form must be attached to every abortion claim or payment will be denied. Complete only one part of this form. This is the only form Montana Healthcare Programs accepts for abortions.
Sterilization
- For elective sterilizations, a completed Informed Consent to Sterilization (MA-38) form must be attached to the claim for each provider involved or payment will be denied. This form must be legible, complete, and accurate, and revisions are not accepted. It is the provider’s responsibility to obtain a copy of the form from the primary or attending physician.
- For medically necessary sterilizations (including hysterectomies), one of the following must be attached to the claim, or payment will be denied:
- A completed Montana Healthcare Programs Hysterectomy Acknowledgement form (MA-39) for each provider submitting a claim. It is the billing provider’s responsibility to obtain a copy of the form from the primary or attending physician. Complete only one section of this form. When no prior sterility or life-threatening emergency exists, the member and physician must sign and date Section A of this form prior to the procedure. (See 42 CFR 441.250 for the federal policy on hysterectomies and sterilizations.) Also, for Section A, signatures dated after the surgery date require manual review of medical records by the Department. The Department must verify that the member (and representative, if any) was informed orally and in writing, prior to the surgery, that the procedure would render the member permanently incapable of reproducing. The member does not need to sign this form when Sections B or C are used.
- For members who have become retroactively eligible for Montana Healthcare Programs, the physician must certify in writing that the surgery was performed for medical reasons and must document one of the following:
- The member was informed prior to the hysterectomy that the operation would render him/her permanently incapable of reproducing.
- The reason for the hysterectomy was a life-threatening emergency.
- The member was already sterile at the time of the hysterectomy and the reason for prior sterility.
When billing for retroactively eligible members, attach a copy of the 160-M to the claim if the date of service is more than 12 months earlier than the date the claim is submitted. For more information, see the Covered Services chapter in this manual.
Billing Unlisted Services or Procedures
Providers should use the most specific HCPCS code when billing a service or procedure to enable proper reimbursement. In the event an unlisted service or procedure code must be used, Montana Healthcare Programs urges providers to send medical records with the claim. Reviewing the medical records with the claim allows the claims processing personnel to understand the situation and apply appropriate reimbursement, as well as decreases claims processing time. Medical records can be sent with electronic claims through the use of the paperwork attachment.
When submitting claims that require additional supporting documentation, the Attachment Control Number field must be populated with an identifier. Identifier formats can be designed by software vendors or clearinghouses, but the preferred method is the provider's Montana Healthcare Programs ID number followed by the member's ID number and the date of service, each separated by a dash.
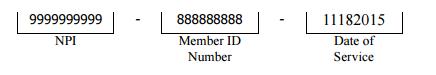
The supporting documentation must be submitted with a Paperwork Attachment Cover Sheet. The number in the paper Attachment Control Number field must match the number on the cover sheet.
End Billing Procedures Chapter
Submitting a Claim
Paper Claims
The services described in this manual are billed on UB-04 claim forms. Use this chapter with the UB-04 claim instructions on the Provider Information website.
Claims submitted with all of the necessary information are referred to as clean and are usually paid in a timely manner. (See the Billing Procedures chapter in the General Information for Providers manual.)
Field 7 is used for cost Passport referral number and sharing indicators. See the table below and UB-04 claim instructions on the Provider Information website.
Passport Indicators
Passport to Health Indicators
Code - Used When Providing
FPS - Family planning services
OBS - Obstetrical services
TCM - Targeted case management services
Present on Admission
The present on admission (POA) indicator is required for all inpatient claims. The claim will deny if there is no valid POA indicator for each diagnosis. Valid values for POA are:
Y = Present at the time of inpatient admission
N = Not present at the time of inpatient admission
U = Documentation is insufficient to determine whether condition is present on admission.
W = Provider is unable to clinically determine whether condition was present on admission.
End Submitting a Claim Chapter
How Payment Is Calculated
Overview
Though providers do not need the information in this chapter to submit claims to the Department, the information allows providers to understand how payment is calculated and to predict approximate payment for particular claims.
The Inpatient Prospective Payment System (PPS)
Several methods of payment are used for inpatient hospital services. These include prospective payment using the All Patient Refined Diagnosis-Related Group (APR-DRG), cost-based payment that is retrospectively adjusted at the end of a reporting period and payment based on a percentage of allowed charges.
- Prospective payment using the APR-DRG method is used for:
- In-State Prospective Payment System Hospitals
- Border hospitals (within 100 miles of Montana’s border)
- Distinct-part units of Montana APR-DRG hospitals and border hospitals.
- Acute care psychiatric hospitals
- Center of Excellence Facilities
- Out-of-state hospitals
- Hospitals and services subject to the cost based payment method include:
- In-state critical access hospitals (CAHs)
The Inpatient Prospective Payment Method Using All Patient Refined Diagnosis Related Groups (APR-DRG)
For most cases, payment equals the relative weight for the APR-DRG times the base price plus the applicable additive factors, such as cost outliers and disproportionate share hospital payment. The overall method is patterned after similar payment policies used by Medicare. When specific details of the payment method differ between Medicare and Montana Healthcare Programs, then the Montana Healthcare Programs policy prevails. Hospitals are not required to purchase grouping software and need not indicate the APR-DRG on the claim.
Upon the discharge or transfer of each member, hospitals submit a claim to Montana Healthcare Programs. The Department reimburses hospitals a per-stay rate based on All Patient Refined Diagnosis Related Groups (APR-DRGs). The claim will provide, among other information, the member’s principal diagnosis, additional diagnoses, principal and secondary procedures, age, sex and discharge status. These variables are passed through an APR-DRG grouper program to determine the appropriate APR-DRG for each discharge. Although hospitals may indicate the anticipated APR-DRG on the billing invoice, the Montana Healthcare Programs grouper program is the final determinant in assigning the payable APR-DRG to each case. Interim billing is only allowed in specific situations noted in this chapter.
After Montana Healthcare Programs has determined the allowed payment amount, that amount is reduced by any reported third party liability (TPL) amount, cost share amount, Medicare Part A payment amount and member responsibility (Incurment), then Montana Healthcare Programs pays the remainder.
Hospitals reimbursed using the inpatient prospective payment method are not subject to retrospective cost reimbursement.
Ungroupable DRG
Claims may sometimes deny for an ungroupable DRG, which is an error in DRG assignment. These errors occur when an invalid or non-existent ICD code is used. Providers should use the ICD codes applicable to the member’s dates of service. For claims that deny due to an ungroupable DRG, providers should re-code thee claim to a more specific and accurate code for the service provided.
Relative Weights and Reimbursement Data
APR-DRG Relative Weights
For each APR-DRG, a relative weight factor is assigned. The relative weight is applied to determine the APR-DRG Base Payment that will be paid for each admit-through-discharge case regardless of the specific services provided or the length of stay. The APR-DRG relative weight is a weight assigned that reflects the typical resources consumed.
APR-DRG weights are reviewed and updated periodically by the Department. The weights are adapted from national databases of millions of inpatient stays and are then “re-centered” so that the average Montana Healthcare Programs stay in a base year has a weight of 1.00.
When the Department determines that adjustments to relative weights for specific APR-DRGs are appropriate to meet Montana Healthcare Programs policy goals related to access to quality care, a policy adjustor may be explicitly applied to increase or decrease these relative weights. Policy adjustors are intended to be budget neutral, that is, they change payments for one type of service relative to other types without increasing or decreasing payments overall.
DRG Base Price
There are two different base prices for stays in acute care hospitals and Center of Excellence hospitals. The base price is a dollar amount that is reviewed by the Department each year. Changes in the APR-DRG Base Price are subject to the public notice requirements of the Montana Code Annotated.
APR-DRG Base Payment
For each stay, the DRG Base Payment equals the DRG Relative Weight multiplied by the DRG Base Price.
Computational Formulas and Definitions
- Covered Charges = Sum of line item charges minus line noncovered charges from the claim.
- Out-of-state statewide Cost-to-Charge Ratio.
- Base Price = Statewide average cost per discharge. The base price is published in the Administrative Rules of Montana.
- Gross APR-DRG Amount = Base price multiplied by APR-DRG relative weight.
- Cost Outlier Amount = (Allowed charges multiplied by the statewide/ hospital-specific cost-to-charge ratio) minus the cost outlier threshold) multiplied by the marginal cost outlier percentage.
- Allowed Montana Healthcare Programs APR-DRG payment = Gross APR-DRG amount plus cost outlier amount.
- Per Diem = Allowed Montana Healthcare Programs APR-DRG payment / national average length of stay for the APR-DRG.
- Transferring hospitals: First Day = 2 x Gross / LOS + outlier Subsequent Days = Gross/LOS.
- Partial eligibility = APR-DRG per diem x eligible days
- Hospital Specific Cost-to-Charge Ratio.
The posted APR-DRG Fee Schedule contains all of the above information.
Payment Factors
Capital Related Costs
Capital cost is included in the DRG-based payment and will not be paid separately.
Cost Outlier Payments
It is recognized that there are occasional stays that are extraordinarily costly in relation to other stays within the same APR-DRG because of the severity of the illness or complicating conditions. These variations are recognized by the cost outlier payment which is an add-on payment for expenses that are not predictable by the diagnosis, procedures performed, and other statistical data captured by the APR-DRG grouper.
Cost outlier stays are stays that exceed the cost outlier threshold for the APR-DRG. To determine if a hospital stay exceeds the cost outlier threshold, the Montana Healthcare Programs program excludes all services that are not medically necessary. Montana Healthcare Programs then converts the charge information for medical necessary services into the estimated cost of the stay by applying the statewide average PPS inpatient cost-to-charge radio (CCR). The estimated cost for medically necessary services is then compared to the cost outlier threshold for the appropriate APR-DRG to determine if the stay qualifies for reimbursement as a cost outlier. Costs exceeding the threshold are multiplied by a marginal cost ratio to determine the cost outlier payment.
Transfer Payment Adjustments
The transfer payment adjustment applies when a patient is transferred to another acute care hospital. It does not apply when a patient is discharged to a post-acute setting such as a skilled nursing facility. The receiving hospital is not impacted by the transfer payment adjustment unless it transfers the patient to another hospital.
In the transfer payment adjustment, payment is calculated as if the beneficiary were not a transfer, then payment is adjusted. The APR-DRG Gross Payment is divided by the nationwide average length of stay for the assigned APR-DRG to arrive at a per diem amount. The per diem amount is then multiplied by the actual length of stay, except that payment is doubled for the first day to reflect costs related to the admitting process. If the transfer payment adjustment results in an amount greater than the amount without the adjustment, the transfer payment adjustment is disregarded. The cost outlier payment, if applicable, is then added to the APR-DRG base payment, with the transfer adjustment made as needed.
The transfer payment adjustment is not applicable to providers and services that are exempt from the Inpatient Prospective Payment Method.
Prorated Payment Adjustment
When a beneficiary has Montana Healthcare Programs coverage for fewer days than the length of stay, the payment is prorated. The APR-DRG Gross Payment plus cost outlier payments, if applicable, is divided by the nationwide average length of stay for the assigned APR-DRG to arrive at a per diem amount. The per diem amount is then multiplied by the number of days the beneficiary is eligible for Montana Healthcare Programs during the stay. If the prorated payment adjustment results in a payment amount greater than the amount without the adjustment, the prorated payment is disregarded.
The Prorated Payment Adjustment is not applicable to providers and services that are exempt from the Inpatient Prospective Payment Method. See the section titled Exempt Services and Costs.
The Cost-Based Payment Method for Exempt Hospitals and Services
The following providers are exempt from the Inpatient Prospective Payment Method. In the interest of clarity, this list includes acute care hospitals as well as facilities that provide similar inpatient services.
- Indian Health Service hospitals
- The Montana State Hospital
- Psychiatric residential treatment facilities
- Critical access hospitals
Exempt Services and Costs
The following services are exempt from the Inpatient Prospective Payment method even when provided by hospitals that are otherwise subject to prospective payment.
- Services where Medicare is the primary payer (crossover claims)
- Certified Registered Nurse Anesthetist costs as defined by Medicare
- Health Care Acquired Conditions as defined by the Centers for Medicare and Montana Healthcare Programs Services (CMS).
Reasonable Cost Reimbursement
Hospitals exempt from prospective payment will continue to use the Title XVIII retrospective reasonable cost principals for reimbursing Montana Healthcare Programs inpatient hospitals services. Allowable costs will be determined in accordance with generally accepted accounting principals as defined by the American Institute of Certified Public Accountants. Such definition of allowable costs is further defined in accordance with the Medicare Provider Reimbursement Manual, CMS Pub. 15-1, subject to the exceptions and limitations provided in the Department’s Administrative Rules. Pub. 15 is a manual published by the United States Department of Health and Human Services, CMS, which provides guidelines and policies to implement Medicare regulations which set forth principals for determining the reasonable cost of provider services furnished under the Health Insurance for Aged Act of 1965, as amended.
Hospitals subject to retrospective reasonable cost reimbursement shall receive interim payments weekly or biweekly during the facility’s fiscal year by submitting claims to the Department’s fiscal intermediary. The interim payment rate will be based on a percentage of customary (billed) charges to costs as determined by the facility’s most recently settled Montana Healthcare Programs cost report. If a provider fails to submit financial information to compute the rate, the provider will be reimbursed at 50 percent of its usual and customary billed charges. Hospital providers are required to submit the CMS 2552-96 to the Medicare Fiscal Intermediary (FI) and the Department within five months of their fiscal year end. The FI either audits or desk reviews the cost report, then sends the Department the “as adjusted” cost report. Montana Healthcare Programs settlements are made from the “as adjusted” cost report.
For each hospital that is a critical access hospital, reimbursement for reasonable costs of inpatient hospital services shall be limited to the lesser of 101 percent of allowable costs or the upper payment limit.
Services where Medicare is the primary payer (crossover claims) are not reimbursed using retrospective cost principles. Reimbursement for these services is the remaining coinsurance and deductible. The Department shall reimburse cost-based inpatient hospital service providers for certified registered nurse anesthetists costs on a reasonable cost basis.
Hospital Residents
Payment for hospital residents will be made as follows:
- Payment for at least the first 180 days of inpatient care at the same facility will be the APR-DRG payment plus any appropriate outliers; and
- Payment for all medically necessary member care subsequent to the request date, which must be greater than 180 days, will be reimbursed at 80% of the hospital-specific estimated cost-to-charge ratio as computed by the Department without cost settlement.
- Services must be prior authorized.
How Payment Is Calculated on TPL Claims
When a member has coverage from both Montana Healthcare Programs and another insurance company, the other insurance company is often referred to as third party liability (TPL). In these cases, the other insurance is the primary payer, and Montana Healthcare Programs makes a payment as the secondary payer. Montana Healthcare Programs will make a payment only when the TPL payment is less than the Montana Healthcare Programs allowed amount.
How Payment Is Calculated on Medicare Crossover Claims
When a member has coverage from both Medicare and Montana Healthcare Programs, Medicare is the primary payer. Montana Healthcare Programs will pay the coinsurance and deductible, less any TPL or
incurment, on inpatient hospital claims for these dually eligible individuals.
Payment Examples for Dually Eligible Members
Member Has Medicare and Montana Healthcare Programs Coverage. A provider submits an inpatient hospital claim for a member with Medicare and Montana Healthcare Programs. The Medicare coinsurance and deductible are $65.00 and $185.00. This total ($250.00) becomes the Montana Healthcare Programs allowed amount. Montana Healthcare Programs will pay this amount ($250.00) as long as no TPL or incurment amounts are applicable.
Member Has Medicare, Montana Healthcare Programs coverage, and TPL. A provider submits an inpatient hospital claim for a member with Medicare, Montana Healthcare Programs, and TPL. The Medicare coinsurance and deductible are $65.00 and $185.00. This total ($250.00) becomes the Montana Healthcare Programs allowed amount. The other insurance company paid $225.00. This amount is subtracted from the Montana Healthcare Programs allowed amount leaving $25.00. Montana Healthcare Programs pays $25.00 for this claim. If the TPL payment had been $250.00 or more, this claim would have paid at $0.00.
Disproportionate Share Hospital (DSH) Payments (ARM 37.86.2925)
Disproportionate Share Hospital (DSH) payments, including routine and supplemental DSH payments, will be limited to the cap established by the Federal Centers for Medicare and Montana Healthcare Programs Services (CMS) for Montana.
Routine DSH shall receive an additional payment amount equal to the product of the hospital’s prospective base rate x the adjustment percent of 4% rural hospital and 10% urban hospitals. All Supplemental Disproportionate Share Hospitals (SDSH) shall receive an SDSH payment. DSH payments will only be given to eligible in-state hospitals.
End How Payment is Calculated Chapter
Appendix A: Forms
The forms listed below are found on the Forms page of the Provider Information website.
- Physician Certification for Abortion Services (MA-37)
- Informed Consent to Sterilization (MA-38)
- Medicaid Hysterectomy Acknowledgment (MA-39)
End of Appendix A: Forms Chapter
Definitions and Acronyms
Acute Care Psychiatric Hospital
A psychiatric facility accredited by the Joint Commission on Accreditation of Health Care Organizations that is devoted to the provision of inpatient psychiatric care for persons under the age of 21 and licensed as a hospital by the Department or an equivalent agency in the state in which the facility is located.
Administratively Necessary Days
“Inappropriate level of care services” means those services for which alternative placement of a patient is planned and/or effected and for which there is no medical necessity for acute level inpatient hospital care.
APR-DRG
All Patient Refined Diagnosis Related Group.
Authorization
An official approval for action taken for, or on behalf of, a Medicaid member. This approval is only valid if the member is eligible on the date of service.
Bad Debt
Inpatient and outpatient hospital services provided in which full payment is not received from the patient or from a third party payer, for which the provider expected payment and the persons are unable or unwilling to pay their bill.
Base Price
Statewide average cost per stay.
Border Hospital
A hospital located outside Montana, but no more than 100 miles from the border.
Capital Related Costs
A cost incurred in the purchase of land, buildings, construction, and equipment as provided in 42 CFR 413.130.
Center of Excellence
A hospital specifically designated by the Department as being able to provided a higher level multi-specialty of comprehensive care and meets the criteria in ARM 37.86.2901.
Charity Care
Inpatient and outpatient hospital services in which hospital policies determine the patient is unable to pay and did not expect to receive full reimbursement.
Clinical Trials
Trials that are directly funded or supported by centers or cooperating groups funded by the National Institutes of Health (NIH), Center for Disease Control (CDC), Agency for Healthcare Research and Quality (AHRQ), Center for Medicare and Medicaid Services (CMS), Department of Defense (DOD), or the Veterans Administration (VA).
Cost-Based Hospital
A licensed acute care hospital that is reimbursed on the basis of allowable costs.
Cost Outlier
An added payment for an unusually high cost case that exceeds the cost outlier thresholds.
Critical Access Hospital (CAH)
A limited-service rural hospital licensed by DPHHS.
Direct Nursing Care
The care given directly to a member that requires the skills and expertise of an RN or LPN.
Discharging Hospital
A hospital, other than a transferring hospital, that formally discharges an inpatient. The release of a patient to another hospital or a leave of absence from the hospital is not considered a discharge.
Disproportionate Share Hospital
A hospital serving a disproportionate share of low income members as defined in Section 1923 of the Social Security Act.
Distinct Part Rehabilitation Unit
A unit of an acute care general hospital that meets the requirements in 42 CFR 412.25 and 42 CFR 412.29.
Graduate Medical Education (GME)
A postgraduate primary care residency program approved by the Accreditation Council for Graduate Medical Education (ACGME) offered by an eligible in-state hospital for the purpose of providing formal hospital-based training and education under the supervision of a licensed medical physician.
Healthcare Acquired Condition
For non-payment, means hospital-acquired conditions as identified by Medicare other than deep vein thrombosis (DVT)/pulmonary embolism (PE) following total knee replacement or hip replacement surgery in pediatric and obstetric patients; and wrong surgical or other invasive procedure performed on a patient, surgical or other invasive procedure performed on the wrong body part, or surgical or other invasive procedure performed on the wrong patient.
Hospital Acquired Condition
A condition that occurs during an inpatient hospital stay and results in high cost or high volumes of care or both; results in a claim being assigned to a diagnose-related group (DRG) that has a higher payment when present as a secondary diagnosis; and could have reasonably been prevented through the application of evidence based on guidelines defined in Section 5001(c) of the Deficit Reduction Act of 2005.
Hospital Reimbursement Adjustor (HRA)
A payment to a Montana hospital as specified in ARM 37.86.2928 and ARM 37.86.2940. All hospitals located in Montana that provide inpatient hospital services are eligible for a hospital reimbursement adjustment payment. The payment consists of two separately calculated amounts: Medicaid inpatient utilization and total Medicaid billed charges.
Hospital Resident
A member who is unable to be cared for in a setting other than the acute care hospital. See Obtaining Resident Status in the Covered Services chapter of this manual.
Inpatient
A member who has been admitted to a hospital with the expectation that he/she will remain more than 24 hours.
Inpatient Hospital Services
Services that are ordinarily furnished in a hospital for the care and treatment of an inpatient under the direction of a physician, dentist, or other practitioner as permitted by federal law.
Interim Claim
In a prospective payment system (PPS), hospital means a claim being billed for an inpatient hospital stay equal to or exceeding 30 days at the same facility as referenced in ARM 37.86.2905.
Low Income Utilization Rate
A hospital’s percentage rate as specified in ARM 37.86.2935.
Medical Inpatient Utilization Rate
A hospital’s percentage rate as specified in ARM 37.86.2932.
Mentally Incompetent
According to CFR 441.251, a mentally incompetent individual means an individual who has been declared mentally incompetent by a federal, state, or local court of competent jurisdiction for any purpose, unless the individual has been declared competent for purposes which include the ability to consent to sterilization.
Partial Eligibility
A member who is only eligible for Medicaid benefits during a portion of the inpatient hospital stay as specified in ARM 37.86.2918.
Present on Admission (POA)
An indicator used to show if a diagnosis was present when the member was admitted to the facility or if the diagnosis appeared after the member was admitted.
Relative Weight
Weight assigned that reflects the resources used in a particular procedure or service.
Routine Disproportionate Share Hospital
A hospital in Montana which meets the criteria of ARM 37.86.2931.
Routine Podiatric Care
Routine podiatric care includes the cutting or removing of corns and calluses, the trimming and debridement of nails, the application of skin creams, and other hygienic, preventive maintenance care.
Rural Hospital
For the purposes of determining disproportionate share hospital payments, an acute care hospital that is located within a “rural area” as defined in 42 CFR 412.62(f)(iii).
Sole Community Hospital
A DRG-reimbursed hospital classified as such by the Centers for Medicare and Medicaid Services (CMS) in accordance with 42 CFR 412.92(a)–(d) and/or hospitals with less than 51 beds.
Supplemental Disproportionate Share Hospital
A hospital in Montana which meets the criteria of ARM 37.86.2925.
Transplant
To transfer either tissue or an organ from one body or body part to another as referenced in ARM 37.86.4701. A transplant may be either an organ transplantation which is the implantation of a living, viable, and functioning human organ for the purpose of maintaining all or a major part of that organ function in the client; or a tissue transplantation which is the implantation of living, human tissue.
Transferring Hospital
A hospital that formally releases an inpatient to another inpatient hospital or inpatient unit of a hospital.
Uncompensated Care
Hospital services provided for which no payment is received from the patient or from a third party payer. Uncompensated care includes charity care and bad debts.
Urban Hospital
An acute care hospital that is located within a metropolitan statistical area, as defined in 42 CFR 412.62(f)(2).
End of Definitions and Acronyms Chapter
Index
Previous editions of this manual contained an index.
This edition has three search options.
- Search the whole manual. Open the Complete Manual pane. From your keyboard press the Ctrl and F keys at the same time. A search box will appear. Type in a descriptive or key word (for example "Denials". The search box will show all locations where denials discussed in the manual.
- Search by Chapter. Open any Chapter tab (for example the "Billing Procedures" tab). From your keyboard press the Ctrl and F keys at the same time. A search box will appear. Type in a descriptive or key word (for example "Denials". The search box will show where denials discussed in just that chapter.
- Site Search. Search the manual as well as other documents related to a particular search term on the Montana Healthcare Programs Site Specific Search page.
End of Index Chapter
End of Hospital Inpatient Services Manual
Update Log
Publication History
This publication supersedes all previous Hospital Inpatient Services handbooks. Published by the Montana Department of Public Health & Human Services, January 2005.
Updated October 2017, June 2018, January 2020, and July 2020.
CPT codes, descriptions and other data only are copyright 2014 American Medical Association (or such other date of publication of CPT). All Rights reserved. Applicable FARS/DFARS Apply.
Update Log
01/01/2020
Cost Share references removed from Billing Procedures, Submitting A Claim, and How Payments Is Calculated Chapters.
Term "Medicaid" replaced with "Montana Healthcare Programs" throughout the manual.
07/01/2020
A duplicate line was removed from the Billings Procedure chapter.
06/05/2018
Definitions and the How Payment is Calculated chapters were revised.
10/16/2017
Hospital Inpatient Services Manual converted to an HTML format and adapted to 508 Accessibility Standards.
End Update Log Chapter
Table of Contents
Key Contacts
Introduction
Manual Organization
Manual Maintenance
Rule References
Claims Review (MCA 53-6-111, ARM 37.85.406)
Getting Questions Answered
Covered Services
General Coverage Principles
- Hospital Inpatient Services (ARM 37.86.2801–2950)
- Services for Children (ARM 37.86.2201-2235)
- Importance of Fee Schedules
Physician Attestation and Acknowledgement (ARM 37.86.2904)
Utilization Reviews (42 CFR 456)
Obtaining Resident Status (ARM 37.86.2921)
Nursing Facility Placement (ARM 37.40.202)
Coverage of Specific Services
- Elective Deliveries
- Clinical Trials (ARM 37.86.2902)
- Inpatient Hospital Services
- Abortions (ARM 37.86.104)
- Air Transports
- Chemical Dependency Treatment
- Discharges
- Donor Transplants
- Emergency Department Admissions
- Mental Health Services
- Observation Bed
- Out-of-State Inpatient Services (ARM 37.86.2801)
- Readmissions (ARM 37.86.2918)
- Same Day Readmission
- Sterilization/Hysterectomy (ARM 37.86.104)
- Transfers (ARM 37.86.2918)
- Transplants (ARM 37.86.4701 and ARM 37.86.2902)
Non-Covered Services (ARM 37.85.207 and ARM 37.86.2902)
Prior Authorization
What is Prior Authorization (ARM 37.86.2801)
Billing Procedures
Claim Forms
Hospital Services Beyond Medical Necessity
Member Cost Sharing (ARM 37.83.825. 37.85.402)
Medicare Benefits Exhausted
Services Provided to Passport to Health Members
Services That Require Prior Authorization
Discharges and Transfers
Bundled Services
Unbundled Services (ARM 37.86.2905(5))
Split/Interim Billing
- Partial Eligibility
- Incurment
Billing for Abortions and Sterilizations
- Abortions
- Sterilizations
Billing Unlisted Services or Procedures
Billing Electronically with Paper Attachments
Submitting a Claim
Paper Claims
Present on Admission
How Payment Is Calculated
Overview
The Inpatient Prospective Payment System (PPS)
The Inpatient Prospective Payment Method Using All Patient Refined Diagnosis Related Groups (APR-DRG)
Ungroupable DRG
Relative Weights and Reimbursement Data
- APR-DRG Relative Weights
- DRG Base Price
- APR-DRG Base Payment
Computational Formulas and Definitions
Payment Factors
- Capital Related Costs
- Cost Outlier Payments
- Transfer Payment Adjustments
- Prorated Payment Adjustment
- The Cost-Based Payment Method for Exempt Hospitals and Services
- Exempt Services and Costs
- Reasonable Cost Reimbursement
Hospital Residents
How Payment Is Calculated on TPL Claims
How Payment Is Calculated on Medicare Crossover Claims
Payment Examples for Dually Eligible Members
Disproportionate Share Hospital (DSH) Payments (ARM 37.86.2925)
Appendix A: Forms
Definitions and Acronyms
Index/How To Search This Manual
End of Table of Contents Chapter
Key Contacts
Hours for Key Contacts are 8 a.m. to 5 p.m. Monday through Friday (Mountain Time), unless otherwise stated. The phone numbers designated only “In state” will not work outside Montana. For additional contacts and websites, see the Contact Us link in the left menu on the Provider Information website.
CLIA Certification
For questions regarding CLIA certification, call or write:
(406) 444-1451 Phone
(406) -444-3456 Fax
Quality Assurance Division
Certification Bureau
DPHHS
2401 Colonial Drive
P.O. Box 202953
Helena, MT 59620-2953
Hospital Program
To qualify a member for residency status or to submit claims for hospital residents:
(406) 444-7018 Phone
(406) 444-4441 Fax
Hospital Program Officer
Health Resources Division
P.O. Box 202951
Helena, MT 59620
Lab
Public Health Lab assistance:
(800) 821-7284 In state
(406) 444-3444 Helena/Out of state
DPHHS Public Health Lab
1400 Broadway
P.O. Box 6489
Helena, MT 59620
Nursing Facility/Swing Bed Pre-Admission Screening
For Level I screening and Level of Care (LOC) screening for members entering a nursing facility or swing bed hospital, contact:
(800) 219-7035 Phone In/Out of state
(406) 443-0320 Phone Helena
(800) 413-3890 Fax In/Out of state
(406) 513-1921 Fax Helena
Mountain-Pacific Quality Health
3404 Cooney Drive
Helena, MT 59602
End Key Contacts Chapter
Introduction
Thank you for your willingness to serve members of the Montana Healthcare Programs and other medical assistance programs administered by the Department of Public Health and Human Services.
Manual Organization
This manual provides information specifically for hospital inpatient services. Other essential information for providers is contained in the separate General Information for Providers manual. Providers are responsible for reviewing both manuals.
A table of contents and an index allow you to quickly find answers to most questions. The margins contain important notes with extra space for writing notes. There is a list of contacts at the beginning of each manual. There is also space on the inside of the front cover to record your NPI for quick reference when calling Provider Relations.
Manual Maintenance
Manuals must be kept current. Changes to manuals are provided through provider notices and replacement pages. Manual replacement pages can be downloaded from the provider type pages on the Provider Information website and are identified by a note at the top of the page indicating Replacement Page and the date. They are designed to be printed on the front and back of each page, so they are always in sets of two beginning with an odd page followed by an even page, even though one of the pages may not have any changes. When replacing a page in a paper manual, file the old pages and provider notices in the back of the manual for use with claims that originated under the old policy.
Rules References
Providers must be familiar with all current rules and regulations governing the Montana Healthcare Programs. Provider manuals are to assist providers in billing Montana Healthcare Programs; they do not contain all Montana Healthcare Programs rules and regulations. Rule citations in the text are a reference tool; they are not a summary of the entire rule. In the event that a manual conflicts with a rule, the rule prevails. Links to rules are available on the Provider Information website. Paper copies of rules are available through the Secretary of State’s office. See the Contact Us link in the left menu on the Provider Information website.
Providers are responsible for knowing and following current Montana Healthcare Programs rules and regulations.
In addition to the general Montana Healthcare Programs rules outlined in the General Information for Providers manual, the following rules and regulations are also applicable to the hospital inpatient program:
- Code of Federal Regulations (CFR)
- 42 CFR 440.10, Inpatient Hospital Services, Other Than Services in an Institution for Mental Disease
- Montana Codes Annotated (MCA)
- MCA Title 50-5-101–50-5-1205, Hospitals and Related Facilities
- Administrative Rules of Montana (ARM)
- ARM Title 37.86.2801–37.86.2950, Inpatient Hospital Services
Claims Review (MCA 53-6-111 and ARM 37.85.406)
The Department is committed to paying Montana Healthcare Programs providers’ claims as quickly as possible. Montana Healthcare Programs claims are electronically processed and usually are not reviewed by medical experts prior to payment to determine if the services provided were appropriately billed. Although the computerized system can detect and deny some erroneous claims, there are many erroneous claims it cannot detect. For this reason, payment of a claim does not mean the service was correctly billed or the payment made to the provider was correct. Periodic retrospective reviews are performed that may lead to the discovery of incorrect billing or incorrect payment. If a claim is paid and the Department later discovers the service was incorrectly billed or paid or the claim was erroneous in some other way, the Department is required by federal regulation to recover any overpayment, regardless of whether the incorrect payment was the result of Department or provider error or other cause.
Getting Questions Answered
The provider manuals are designed to answer most questions; however, questions may arise that require a call to a specific group (such as a program officer, Provider Relations, or a prior authorization unit). A list of key contacts and websites is available online. On the Provider Information website, choose the Contact Us link in the left menu. Providers should also read the monthly Claim Jumper newsletter for Montana Healthcare Programs updates and changes. Montana Healthcare Programs provider manuals, provider notices, replacement pages, fee schedules, forms, and more are available on the Provider Information website.
End of Introduction Chapter
Covered Services
General Coverage Principles
Montana Healthcare Programs covers inpatient hospital services when they are medically necessary. This chapter provides covered services information that applies specifically to inpatient hospital services. Like all healthcare services received by Montana Healthcare Programs members, these services must also meet the general requirements listed in the Provider Requirements chapter of the General Information for Providers manual.
Hospital Inpatient Services (ARM 37.86.2801–2950)
Inpatient hospital services are provided to Montana Healthcare Programs members who are formally admitted as an inpatient and whose expected hospital stay is greater than 24 hours. Inpatient services must be ordered by a licensed physician or dentist and provided in an institution maintained primarily for treatment and care of patients with disorders other than tuberculosis or mental diseases. The institution must be currently licensed by the designated state licensing authority in the state where the institution is located, must meet the requirements for participation in Medicare as a hospital, and must have in effect a utilization review plan that meets the requirements of 42 CFR 482.30.
Services for Children (ARM 37.86.2201–2235)
The Early and Periodic Screening, Diagnostic, and Treatment (EPSDT) Services program is a comprehensive approach to healthcare for Montana Healthcare Programs members ages 20 and under. It is designed to prevent, identify, and then treat health problems before they become disabling. Under EPSDT, Montana Healthcare Programs eligible children may receive any medically necessary covered service, including all inpatient hospital services described in this manual. All applicable Passport to Health and prior authorization requirements apply.
Importance of Fee Schedules
The easiest way to verify coverage for a specific service is to check the Department’s fee schedule for your provider type. In addition to being listed on the fee schedule, all services provided must also meet the coverage criteria listed in the Provider Requirements chapter of the General Information for Providers manual and in this chapter. Use the fee schedule in conjunction with the more detailed coding descriptions listed in the current ICD coding book. Take care to use the fee schedule and coding books that pertain to the date of service. Fee schedules are available on the Provider Information website.
Physician Attestation and Acknowledgment (ARM 37.86.2904)
At the time a claim is submitted, the hospital must have on file a signed and dated acknowledgment from the attending physician that the physician has received the following notice:
Notice to physicians: Montana Healthcare Programs payment to hospitals is based on all of each patient’s diagnoses and the procedures performed on the patient, as attested to by the patient's attending physician by virtue of his or her signature in the medical record. Anyone who misrepresents, falsifies or conceals essential information required for payment of federal funds, may be subject to fine, imprisonment or civil penalty under applicable federal laws.
The acknowledgement must be completed by the physician at the time that the physician is granted admitting privileges at the hospital, or before or at the time the physician admits his/her first member to the hospital. Existing acknowledgments signed by physicians already on staff remain in effect as long as the physician has admitting privileges at the hospital. The provider may, at its discretion, add to the language of this statement the word Medicare so that two separate forms will not be required by the provider to comply with state and federal requirements.
Utilization Reviews (42 CFR 456)
The Department or its contractor may at any time review paid claims, provider documentation for medical necessity, appropriate billing, etc. Providers must maintain documentation of medical necessity for services such as initial hospitalization, transfers, and readmissions. For more information on provider requirements for maintaining documentation, see the Record Keeping section in the Provider Requirements chapter of the General Information for Providers manual. Also see the Claims Review section in the Introduction chapter of this manual.
Obtaining Resident Status (ARM 37.86.2921)
Providers must contact the Department to obtain hospital residence status prior to billing Montana Healthcare Programs. To qualify for residency status, a member must meet the following requirements:
- Use a ventilator for a continuous period of not less than 8 hours in a 24-hour period or require at least 10 hours of direct nursing care in a 24-hour period.
- Must have been an inpatient in an acute care hospital for a minimum of 6 continuous months within the requesting facility.
It is the provider’s responsibility to determine whether services could be provided in a skilled nursing care facility or by the Home and Community-Based Waiver Program. The provider must maintain written records of inquiries and responses about the present and future availability of openings in nursing facilities and the Home and Community-Based Waiver Program. A redetermination of nursing facility or waiver availability must be made at least every 6 months.
Nursing Facility Placement (ARM 37.40.202)
Hospitalized Montana Healthcare Programs members and Montana Healthcare Programs applicants being considered for nursing facility placement from the hospital shall be referred in a timely manner to the preadmission screening team. The preadmission screening form (Form DPHHS-SLTC-61) must be completed before placement and payment is made on their behalf.
Coverage of Specific Services
Elective Deliveries
Effective July 1, 2014, all facilities must have a hard-stop policy in place regarding non-medically necessary inductions prior to 39 weeks and nonmedically necessary Cesarean sections at any gestational age. The policy must contain the following:
- No non-medically necessary inductions and Cesarean sections prior to39 weeks and 0/7 days gestation, and no non-medically necessary Cesarean sections at any gestational age.
- Confirmation of weeks gestation by ACOG guidelines (at least one of the following guidelines must be met to show gestational age):
- Fetal heart tones have been documented for 20 weeks by non-electronic fetoscope or 30 weeks by Doppler;
- 36 weeks since a positive serum or urine pregnancy test that was performed by a reliable laboratory; or
- An ultrasound prior to 20 weeks that confirms the gestational age of at least 39 weeks.
- If pregnancy care was not initiated prior to 20 weeks gestation, the gestational age may be documented from first day of the last menstrual period (LMP).
- Policy must have a multistep review process prior to all inductions and Cesarean Sections including final decision being made by the Perinatology Chair/Obstetrical Chair, OB Director, or Medical Director.
Effective October 1, 2014, Montana Healthcare Programs will reduce reimbursement rates for non-medically necessary inductions prior to 39 weeks, and non-medically necessary Cesarean sections at any gestational ages. All hospital claims with an admit date on or after October 1, 2014, will require coding changes to delivery claims.
Hospital inpatient claims and birthing center claims will require the use of condition codes for all induction and Cesarean section deliveries. These claims will be reviewed for medical necessity based on an approved list of diagnosis codes. The condition codes are:
- 81 − Cesarean section or induction performed at less than 39 weeks gestation for medical necessity.
- 82 − Cesarean section or induction performed at less than 39 weeks gestation elective.
- 83 − Cesarean section or induction performed at 39 weeks gestation or greater.
Clinical Trials (ARM 37.86.2902)
Clinical trial drugs, devices, and procedures are not reimbursable. Clinical trials are limited to Montana Healthcare Programs coverage of routine costs plus reasonable and necessary items and services used to diagnose and treat complications arising from participation in all qualifying clinical trials. Qualifying clinical trials include those that are directly funded or supported by centers or cooperating groups funded by the National Institutes of Health (NIH), Centers for Disease Control (CDC), Agency for Healthcare Research and Quality (AHRQ), Department of Defense (DOD), or Veterans Affairs (VA).
Inpatient Hospital Services
The following are coverage rules for specific inpatient hospital services. Inpatient hospital services included in the All Patient Refined Diagnosis-Related Group (APR-DRG) payment methodology include all routine services such as the following:
- Bed and board
- Nursing services and other related services
- Use of hospital facilities
- Medical social services
- Drugs, biologicals, supplies, appliances, and equipment furnished by the hospital for the care and treatment of inpatients
- Other diagnostic or therapeutic items or services provided in the hospital that are not specifically excluded (ARM 37.85.207). See the Non-Covered Services section in this chapter.
- Outpatient services provided by the hospital facility the day of admission or the day before.
Abortions (ARM 37.86.104)
Abortions are covered when one of the following conditions are met:
- The member’s life would be endangered if the fetus is carried to term.
- The pregnancy is the result of rape or incest.
- The abortion is determined by the attending physician to be medically necessary, even if the member’s life is not endangered if the fetus is carried to term.
A completed Montana Healthcare Programs Physician Certification for Abortion Services (MA-37) form must be submitted with every abortion claim or payment will be denied. Complete only one section of this form. This form is the only form Montana Healthcare Programs accepts for abortion services.
When using mifepristone (Mifeprex or RU 486) to terminate a pregnancy, it must be administered within 49 days from the beginning of the last menstrual period by or under the supervision of a physician who:
- Can assess the duration of a pregnancy.
- Can diagnose ectopic pregnancies.
- Can provide surgical intervention in cases of incomplete abortion or severe bleeding, or can provide such care through other qualified physicians.
- Can assure access to medical facilities equipped to provide blood transfusion and resuscitation.
- Has read, understood, and explained to the member the prescribing information for mifepristone.
Air Transports
Air transport providers must be registered with Montana Healthcare Programs as an ambulance provider. Claims for these services are billed on a CMS-1500 claim form. See the Ambulance Services manual available on the Provider Information website.
Chemical Dependency Treatment
Chemical dependency services are limited. Providers must be approved by the Department before providing this service. Contact the Chemical Dependency Bureau for information. (See the Contact Us link on the Provider Information website.)
Discharges
A hospital’s utilization review (UR) committee must comply with the Code of Federal Regulations 42 CFR 456.131 through 42 CFR 456.137 prior to notifying a Montana Healthcare Programs member that he/she no longer needs medical care. The hospital is not required to obtain approval from Montana Healthcare Programs at the member’s discharge; however, a hospital’s UR plan must provide written notice to Montana Healthcare Programs if a member decides to stay in the hospital when it is not medically necessary. (See the Hospital Services Beyond Medical Necessity section in the Billing Procedures chapter of this manual.)
Donor Transplants
Montana Healthcare Programs covers successful donor-related testing and services and organ acquisition services, which are bundled into the Montana Healthcare Programs member’s transplant hospitalization, and are covered in this APR-DRG payment.
Emergency Department Admissions
Emergency medical services are those services required to evaluate, treat and stabilize an emergency medical condition.
Mental Health Services
Montana Healthcare Programs covers inpatient mental health services for Montana Healthcare Programs-enrolled members when prior authorized. (See the Prior Authorization chapter in this manual. and refer to the mental health manual available on the Provider Information website.)
Observation Bed
Members in observation beds (admission of 72 hours or less) are considered outpatients and claims should be filed accordingly. (See the Hospital Outpatient Services manual available on the Provider Information website.)
Out-of-State Inpatient Services (ARM 37.86.2801)
Montana Healthcare Programs covers treatment in an out-of-state facility only when all of the following requirements are met:
- The member cannot be treated in state, and the provider contacts the prior authorization designated review organization to determine if services are available in Montana before considering placement in an out-of-state facility.
- The provider received prior authorization for out-of-state services before the member is sent to an out-of-state hospital. See the Prior Authorization chapter in this manual for more information.
It is not the intent of the Montana Healthcare Programs to interfere or delay a transfer when a physician has determined a situation to be emergent. Prior authorization is not required in emergency situations. Emergency inpatient admissions must be authorized within 2 working days (Monday–Friday) of admission to an out-of-state hospital.
If a hospital that is located over 100 miles outside of the borders of Montana or a Center for Excellence hospital fails to obtain prior authorization before providing services to a Montana Healthcare Programs member, retrospective authorization may be granted under the following circumstances only: The person to whom services were provided was determined by the Department to be retrospectively eligible for Montana Healthcare Programs benefits;
- The hospital can document that the admission was an emergency admit for the purpose of stabilization or stabilization for transfer;
- The hospital must call for authorization within three working days (Monday-Friday) of the admission or knowledge of the member’s Montana Healthcare Programs eligibility;
- Interim claims equal to or greater than 30 days of continuous inpatient services at the same facility; or
- The hospital is retroactively enrolled as a Montana Healthcare Programs provider, and the enrollment includes the dates of service for which authorization is requested; provided the hospital’s retroactive enrollment is completed, allowing time for the hospital to obtain prior authorization and to submit a clean claim within timely filing deadlines in accordance with ARM 37.85.406.
Readmissions (ARM 37.86.2918)
All readmissions are subject to review for medical necessity of the initial stay as well as the subsequent hospitalization stay. Reimbursement cannot be made to a provider unless the service provided was medically necessary. Readmission may be reviewed on a retrospective basis to determine if additional payment for the case is warranted. If complications have arisen because of premature discharge and/or other treatment errors, then the APR-DRG payment for the first admission must be combined with the current admission before billing Montana Healthcare Programs. If the readmission is for the treatment of conditions that could or should have been treated during the previous admission, the two admissions must be combined into one admission for payment purposes.
A member readmission occurring in an inpatient rehabilitation hospital or distinct part unit three days after the initial date of discharge must be combined into one admission for payment purposes, with the exception of discharge to an acute care hospital for surgical APR-DRGs. Inpatient readmissions within 24 hours must be combined if the same condition is coded.
Same Day Readmission
If a member is readmitted on the same day of discharge for the same condition, the entire stay must be billed as one admission.
If a member is readmitted on the same day of discharge for a separate condition, Montana Healthcare Programs may be billed for the new condition. The claim for the new condition and a letter of explanation including documentation for the separate condition must be sent directly to the Hospital Program Officer for review.
A member readmission occurring in an inpatient rehabilitation hospital or distinct part unit three days after the initial date of discharge must be combined into one admission for payment purposes, with the exception of discharge to an acute care hospital for surgical APR-DRGs. Inpatient readmissions within 24 hours must be combined if the same condition is coded.
Sterilization (ARM 37.86.104)
Elective Sterilization
Elective sterilizations are sterilizations done for the purpose of becoming sterile. Montana Healthcare Programs covers elective sterilization for men and women when all of the following requirements are met:
- Member must complete and sign the Informed Consent to Sterilization (MA-38) form at least 30 days, but not more than 180 days, prior to the sterilization procedure. This form is the only form Montana Healthcare Programs accepts for elective sterilizations. If this form is not properly completed, payment will be denied. See the Forms page on the Provider Information website for the form and instructions for completing.
- Member must be at least 21 years of age when signing the form.
- Member must not have been declared mentally incompetent by a federal, state, or local court, unless the member has been declared competent to specifically consent to sterilization.
- Member must not be confined under civil or criminal status in a correctional or rehabilitative facility, including a psychiatric hospital or other correctional facility for the treatment of the mentally ill.
The 30-day waiting period may be waived for either of the following reasons:
- Premature Delivery. The Informed Consent to Sterilization must be completed and signed by the member at least 30 days prior to the estimated delivery date and at least 72 hours prior to the sterilization.
- Emergency Abdominal Surgery. The Informed Consent to Sterilization form must be completed and signed by the member at least 72 hours prior to the sterilization procedure.
All forms required for sterilizations can be downloaded from the Provider Information website,
Before performing a sterilization, the following requirements must be met:
- The member must have the opportunity to have questions regarding the sterilization procedure answered to his/her satisfaction.
- The member must be informed of his/her right to withdraw or withhold consent any time before the sterilization without being subject to retribution or loss of benefits.
- The member must be made aware of available alternatives of birth control and family planning.
- The member must understand the sterilization procedure being considered is irreversible.
- The member must be made aware of the discomforts and risks which may accompany the sterilization procedure being considered.
- The member must be informed of the benefits and advantages of the sterilization procedure.
- The member must know that he/she must have at least 30 days to reconsider his/her decision to be sterilized.
- An interpreter must be present and sign for those members who are blind, deaf, or do not understand the language to assure the person has been informed.
Informed consent for sterilization may not be obtained under the following circumstances:
- If the member is in labor or childbirth.
- If the member is seeking or obtaining an abortion.
- If the member is under the influence of alcohol or other substance which affects his/her awareness.
Medically Necessary Sterilization
When sterilization results from a procedure performed to address another medical problem, it is considered a medically necessary sterilization. These procedures include hysterectomies, oophorectomies, salpingectomies and orchiectomies. Every claim submitted to Montana Healthcare Programs for a medically necessary sterilization must be accompanied by one of the following:
- A completed Montana Healthcare Programs Hysterectomy Acknowledgement form (MA-39). It is the provider’s responsibility to obtain a copy of the form from the primary or attending physician. Complete only one section of this form. When no prior sterility (Section B) or no life-threatening emergency (Section C) exists, the member and physician must sign and date Section A of this form prior to the procedure. (See 42 CFR 441.250 for the federal policy on hysterectomies and sterilizations). Also, for Section A, signatures dated after the surgery date require manual review of medical records by the Department. The Department must verify that the member (and representative, if any) was informed orally and in writing, prior to the surgery, that the procedure would render the member permanently incapable of reproducing. The member does not need to sign this form when Sections B or C are used.
- For members who have become retroactively eligible for Montana Healthcare Programs, the physician must certify in writing that the surgery was performed for medical reasons and must document one of the following:
- The individual was informed prior to the hysterectomy that the operation would render them permanently incapable of reproducing.
- The reason for the hysterectomy was a life-threatening emergency.
- The member was already sterile at the time of the hysterectomy and the reason for prior sterility.
When submitting claims for retroactively eligible members, attach a copy of the 160-M to the claim if the date of service is more than 12 months earlier than the date the claim is submitted.
Transfers (ARM 37.86.2918)
All diagnostic services are included in the APR-DRG payment. Diagnostic services that are performed at a second APR-DRG hospital, because the services are not available at the first hospital (e.g., a CT scan), are included in the first hospital’s APR-DRG payment. This includes transportation to the second hospital and back to the first hospital. Arrangement for payment to the transportation provider and the second hospital where the services were actually performed must be between the first and second hospital and the transportation provider.
All transfers are subject to review for medical necessity. The initial hospitalization, all subsequent hospitalizations, and the medical necessity for the transfer itself may be reviewed. For information on billing and payment for transfers, see this manual’s Billing Procedures and How Payment Is Calculated chapters.
Transplants (ARM 37.86.4701–ARM 37.86.4706)
Montana Healthcare Programs covers organ and tissue transplants that are medically necessary and not considered experimental or investigational. Organ transplants must be performed in a Medicare-certified facility. If Medicare has not designated a facility as being certified, the transplant must be performed by a program located in a hospital or parts of a hospital certified by the Organ Procurement and Transplantation Network (OPTN) for the specific organ being transplanted. A list of CMS-certified facilities is on the CMS website at http://www.cms.hhs.gov. (Search for transplant program certification.)
Organ and tissue transplantation includes the transplant surgery and those activities directly related to the transplantation. These activities may include:
- Evaluation of the member as a potential transplant candidate
- Pre-transplant preparation including histo-compatibility testing procedures
- Post-surgical hospitalization
- Outpatient care, including Federal Drug Administration (FDA) approved medications deemed necessary for maintenance or because of resulting complications
- Associated medical expenses for the successful donor only. (These will be bundled into the Montana Healthcare Programs member’s inpatient transplant hospitalization.)
These activities are covered by Montana Healthcare Programs as long as the member remains Montana Healthcare Programs-eligible and transplantation is prior approved. Services must comply with Medicare coverage guidelines for organ and tissue transplant services. If Medicare coverage guidelines are not available, the Department or their designated review organization will review the requested transplant surgery to determine if the surgery is experimental or investigational.
Non-Covered Services (ARM 37.85.207 and ARM 37.86.2902)
The following medical and nonmedical services, except as otherwise specified in program-specific rules as a waiver service or an EPSDT service, are explicitly excluded from the Montana Healthcare Programs, except for those services specifically available, as listed in ARM 37.40.1406, 37.90.402, and Title 37, Chapter 34, Subchapter 9, to persons eligible for home and community-based services; and except for those Medicare-covered services as listed in ARM 37.83.812 to qualified Medicare beneficiaries for whom the Montana Healthcare Programs pays the
Medicare premiums, deductible, and coinsurance.
- Acupuncture
- Autopsies
- Bariatric services and surgery-related services (including bypass and revisions)
- Chiropractic services
- Circumcisions not authorized by the Department as medically necessary
- Delivery services not provided in a licensed healthcare facility or nationally accredited birthing center unless as an emergency service
- Dietary supplements
- Dietician services (some services covered per ARM 37.86.3002)
- Donor search expenses
- Erectile dysfunction products, including but not limited to injections, devices, and oral medications used to treat impotence
- Experimental services, services that do not comply with national standards of medical practice, non-FDA-approved drugs, biologicals and devices, and clinical trials are excluded from coverage.
- Experimental services or services that are generally regarded by the medical profession as unacceptable treatment not medically necessary for the purposes of the Montana Healthcare Programs.
- Homemaker services
- Infertility treatment services, including sterilization reversals
- Masseur/Masseuse services
- Medical services furnished to Montana Healthcare Programs-eligible members who are absent from the state including a child residing in another state for whom Montana makes adoption assistance or foster care maintenance payments are covered as in each program-specific rule and subject to the applicable conditions of those rules.
- Naturopathic services
- Nutritional services
- Physical therapy aide services
- Services that are not directly related to patient care including, but not limited to, car repair and/or modification of automobile, mileage for travel expenses for providers, missed or canceled appointments, plumbing service, preparation of medical or insurance reports, remodeling of home, service charges or delinquent payment fees, telephone services in the home).
- Services that are not medically necessary. The Department may review for medical necessity at any time before or after payment. The Montana Healthcare Programs member is financially responsible for these services if the member agrees in writing before the services are provided. See the When to Bill Montana Healthcare Programs Members section in the Billing Procedures chapter of the General Information for Providers manual
- Sexual aids including, but not limited to, devices, injections and oral medications
- Surgical technician services (technicians who are not physicians or mid-level practitioners)
End of Covered Services Chapter
Prior Authorization
Prior Authorization Requirements
Many services require prior authorization before they may be provided. These requirements have been established after consultation with the Department’s DUR Board. Criteria listed for each therapy are derived from reviews completed by the University of Montana’s School of Pharmacy and approved by the DUR Board. Prior Authorization requests are reviewed for medical necessity. When seeking prior authorization, keep in mind the following:
- Prior authorization does not guarantee payment.
- Always refer to the applicable Montana Healthcare Programs fee schedule to verify if prior authorization is required for specific services. The table on the following page, Prior Authorization Criteria for Specific Services, lists services that require prior authorization and the corresponding criteria.
- Remember to bill for only the number of units that were prior authorized.
- To request prior authorization, providers must submit the information requested on the Mountain-Pacific Quality Health Request for Drug Prior Authorization form to the Prior Authorization Unit. This form is available on the Forms page of the Provider Information website.
- Physicians, home infusion therapy providers, or pharmacy providers may submit prior authorization requests by mail, telephone, or fax to the Prior Authorization Unit.
- Requests are reviewed and decisions made immediately in most cases. Decisions on requests with special circumstances that require further peer review are made within 24 hours. Requests received after the Prior Authorization Unit’s regular working hours of 8 a.m. to 5 p.m. Monday through Friday or on weekends or holidays are considered received at the start of the next working day.
- If the weekend/holiday request is for an emergency situation, providers may supply therapies shown on the Montana Healthcare Programs fee schedule and payment will be authorized up to a maximum of 3 days. Montana Healthcare Programs may routinely audit these emergency authorizations for validity and appropriateness. Therapies in the “other infusion therapies” category will not be authorized on an emergency basis. Provider who are billing point-of-sale should refer to the Prescription Drug Program manual when billing for emergency therapies.
- The Prior Authorization Unit notifies the provider when prior authorization has been granted or denied. Upon approval, providers will receive a prior authorization number that must be recorded on the claim.
Prior Authorization for Retroactively Eligible Members
When submitting claims for retroactively eligible members in which the date of service is more than 12 months earlier than the date the claim is submitted, attach a copy of the Provider Notice of Eligibility (Form 160-M). To obtain Form 160-M the provider needs to contact the member’s local Office of Public Assistance and request the form. For a list of local Offices of Public Assistance, see the DPHHS website, https://dphhs.mt.gov/hcsd/OfficeofPublicAssistance.
Prior Authorization Criteria for Specific Services
Service: Alpha 1 proteinase inhibitor (Prolastin)
Criteria: Alpha 1 antitrypsin deficiency must be documented via laboratory information.
Service: Anticoagulant therapy
Criteria:
- Member must not be a candidate for low molecular weight heparin therapy, either due to therapy failure, member status, or diagnosis.
- A plan for oral therapy must be submitted, if appropriate.
Service: Antiemetic therapy
Criteria: Member must have failed all other forms of antiemetic therapy including oral, rectal, and intermittent subcutaneous injection.
Service: Anti-infective therapy (antibiotics/antifungals/antivirals)
Criteria:
- IV antibiotic therapy for two weeks or less will be authorized upon request.
- IV antibiotic therapy for more than two weeks will be considered on an individual basis depending on diagnosis and member condition.
- IV antibiotic therapy using IV fluoroquinolones or metronidazole has not been found to have any therapeutic advantage over oral therapies and also requires prior authorization.
Service: Antispasmodic therapy
Criteria: Member must have failed oral forms of antispasmodic therapy.
Service: Anti-tumor necrosis factor (Remicaid)
Criteria: The indication must be FDA-approved or have good published studies supporting the indication for use.
Service: Chemotherapy
Criteria:
- The indication must be FDA-approved or have good published studies supporting the indication for use.
- The drugs must not be considered vesicants, which cause severe local necrosis (tissue damage) and should not be given in the home; extravasation (leaking out of the vein into local tissue) needs to be recognized and treated immediately. Too dangerous a side-effect for the home administration.
Service: Chelation (desferal therapy)
Criteria: Documentation of hemochromatosis, acute iron poisoning, or abnormal storage of iron due to multiple blood transfusions.
Service: Immunomodulating agents
Criteria:
- Prior authorization is required for the use of any intravenous immunoglobulin (IVIG) products.
- Must be a diagnosis of one of the following:
- Primary immunodeficiency disorders with a history of recurrent infections
- Idiopathic thrombocytopenic purpura (ITP):
- Children with newly diagnosed ITP who are not a risk for serious hemorrhage
- Chronic ITP
- Adult-onset ITP in those members who do not respond to initial corticosteroid therapy
- Allogeneic bone marrow transplantation
- Symptomatic pediatric HIV infection and CD4 lymphocyte count greater than 200
- Chronic lymphocytic leukemia with a history of at least one serious bacterial infection
- Guillain-Barre syndrome
- Kawasaki syndrome
Service: Inotropic agents (dobutamine therapy)
Criteria: Must be a diagnosis of chronic refractory CHF which meets these criteria:
- Member shows no clinical improvement (FC-III or FC-IV) despite treatment with maximum or near-maximum tolerated doses of standard oral therapy for CHF (unless allergic or intolerant).
- Member is clinically stable on the dosage to be administered at home prior to discharge from the hospital.
- Member demonstrates either an improvement in FC from IV to III or an improvement in symptoms (less dyspnea, improved diuresis, improved renal function, and/or reduction in weight) and hemodynamic parameters (at least 20 percent increase in cardiac output, decreased pulmonary artery pressure, and/or a decrease in pulmonary capillary wedge pressure, measured invasively within six months prior to the initiation of therapy).
- Member demonstrates a clinical dependence on the inotrope as evidenced by deterioration in clinical status when the drug is tapered or discontinued.
Service: Pain management
Criteria:
- All other forms of pain therapy must have failed, including but not limited to oral, sublingual, rectal, or topical.
- The member must not be a candidate for or member of hospice services.
Service: Total parenteral nutrition (TPN)
Criteria:
- Recertification is required at 3 months, 9 months, and 24 months after the initiation of therapy. After 2 years, authorization will be determined on a case-by-case basis. If, at any time, there is a break in service to the member of two consecutive months, the entire review process will begin again.
- Members must meet the following criteria:
- A member must be unable to meet nutrient requirements via the GI tract safely and adequately. Adequate nutrition cannot be completely possible by dietary adjustment, oral supplements, or tube enteral nutrition.
- The member’s GI tract must be severely diseased, preventing absorption of adequate nutrients to maintain weight and strength consistent with the member’s overall status. TPN must be necessary to sustain the member’s life. Examples of conditions and/or functional impairments that may qualify for coverage include, but are not limited to:
- Massive small bowel resection
- Crohn’s disease
- Sprue disease
- Short bowel syndrome
- Radiation enteritis
- Malabsorption documented by a physician
- GI tract mechanical obstruction
- A total caloric intake of 20–35 kcal/kg (of ideal body weight)/day constitutes nutritional dependence.
- Peripheral parenteral nutrition may be used in selected members to provide partial or total nutrition support for up to 2 weeks in members who cannot ingest or absorb adequate oral or enteral tube-delivered nutrients, or when central-vein parenteral nutrition is not feasible.
- The member should not have pulmonary edema, congestive heart failure (New York Heart Association Functional Class 3 or 4), or any other medical condition that would increase the risk of home administration.
- Central-vein parenteral nutrition support, including support via a PICC line, is provided when parenteral feeding is indicated for longer than 2 weeks, peripheral venous access is limited, or nutrient needs are large or fluid restriction is required.
Service: Other therapies
Criteria: Anticipating that new infusion therapies will be developed or that a current therapy has been overlooked, the Department will consider authorization of other therapies on an individual basis. These special requests may require literature documentation, peer review, as well as review by the DUR Board. In addition, the request will require cost information for setting a per diem rate. Contact the Prior Authorization Unit. See Key Contacts.
End of Prior Authorization Chapter
Billing Procedures
Claim Forms
Services provided by the healthcare professionals covered in this manual must be billed either electronically or on UB-04 claim forms, which are available from various publishing companies; they are not available from the Department or Provider Relations.
Hospital Services Beyond Medical Necessity
The Montana Healthcare Programs member who chooses to remain in the hospital beyond the period of medical necessity may choose to pay for continued inpatient care as a Montana Healthcare Programs noncovered service. The member must have been informed in writing and agreed in writing prior to provision of services to accept financial responsibility. The agreement must state the specific services the Montana Healthcare Programs member has agreed to pay for. In this case, a routine agreement will not suffice. Montana Healthcare Programs may not be billed for hospital services that are not medically necessary.
A hospital’s utilization review plan must provide written notice to Montana Healthcare Programs if a Montana Healthcare Programs member decides to stay in the hospital when it is not medically necessary. This written notice must be sent to the hospital program officer. (See Key Contacts in this manual or the Contact Us link in the left menu on the Provider Information website.)
Member Co-Payment (ARM 37.83.825 and 37.83.826)
Effective for all claims paid on or after January 1, 2020 copayment will not be assessed.
Medicare Benefits Exhausted
Medicare crossovers are claims for hospital patients who are eligible for Medicare Part A benefits and Montana Healthcare Programs. For these members, Montana Healthcare Programs pays the deductibles and coinsurance related to the inpatient hospital services. Should a Medicare/Montana Healthcare Programs member exhaust the Medicare benefit (including Lifetime Reserve Days), the claim will be treated as a Montana Healthcare Programs-only claim from the date the Medicare benefits were exhausted. The claim should be submitted reflecting a covered stay from the day the Medicare benefits were exhausted to discharge. This situation is the only instance in which a hospital should submit a split bill for a case that will be paid using prospective payment principles.
Services Provided to Passport to Health Members
A Montana Healthcare Programs member covered by the Passport to Health program must have inpatient hospital services approved by the member’s primary care provider (PCP). The Passport provider number must be on the claim or the service will be denied.
Services That Require Prior Authorization
Prior authorization is required for some hospital services. Passport and prior authorization are different, and some services may require both. See the Passport chapter in the General Information for Providers manual and/or the Prior Authorization chapter in this manual and the Prior Authorization Information page of the Provider Information website. Different codes are issued for each type of approval and must be included on the claim form, or the claim will be denied. See the Submitting a Claim chapter in this manual.
Discharges and Transfers
Claims can be filed only after the member has been discharged. A member is considered discharged when he or she is:
- Formally released from the hospital
- Transferred to another hospital or rehabilitation unit
- Dies in the hospital
- Leaves the hospital against medical advice (AMA)
- Discharge to hospice
- Transferred to a LTCF, SNF, ICF, or swing bed
The hospital that ultimately discharges the member bills Montana Healthcare Programs. When a member is transferred from one hospital to another for services the first hospital does not provide (e.g., CT scan) and then back to the first hospital, all diagnostic services are included in the APR-DRG payment to the first hospital. Also included in the same payment are the services that were provided at the second hospital and transportation to the second hospital and back to the first hospital. Arrangement for payment to the transportation provider and the second hospital must be arranged between the first and second hospital and the transportation provider.
Providers must notify the Department when a member chooses to stay in the hospital when it is not medically necessary.
All transfers are subject to review for medical necessity. Initial hospitalizations, subsequent hospitalizations, and transfers may be reviewed for medical necessity. Reimbursement cannot be made to a provider unless the service provided was medically necessary.
The patient status code should contain the appropriate discharge status code. The following discharge status codes are valid for Montana Healthcare Programs.
Discharge Status Codes
01 Discharged to home or self-care (routine discharge)
02 Discharge/Transfer to another short-term general hospital for inpatient care
03 Discharge/Transfer to skilled nursing facility (SNF)
04 Discharge/Transfer to an intermediate care facility (ICF)
05 Discharge/Transfer to another type of institution for inpatient care
06 Discharge/Transfer to home under care of organized home health service organization
07 Left against medical advice or discontinued care
08 Discharge/Transfer to home under care of a Home IV provider
09 Admitted as an inpatient to this hospital 63 Discharge/Transfer to a long-term care hospital
20 Expired (death) 64 Discharge/Transfer to nursing facility certified under Montana Healthcare Programs, but not Medicare
30 Still a patient (Neonate providers discharge status code for interim billing.)
40 Expired (death) at home
41 Expired in a medical facility (e.g., hospital, SNF, ICF, or free standing hospice)
42 Expired – place unknown
43 Discharge/Transfer to Federal hospital
50 Hospice – home
51 Discharge/Transfer to hospice medical facility
61 Discharge/Transfer within this institution to hospital-based Medicare-approved swing bed
62 Discharge/Transfer to another rehabilitation facility including rehabilitation distinct part units of a hospital
63 Discharge/Transfer to a long-term care hospital
64 Discharge/Transfer to nursing facility certified under Montana Healthcare Programs, but not Medicare
65 Discharge/Transfer to a psychiatric hospital or psychiatric distinct part unit of a hospital
Bundled Services
Services that are included in the APR-DRG payment are considered bundled and include the following:
- Services provided on the day of admission or on the day preceding admission.
- All routine services. (See Coverage of Specific Services in the Covered Services chapter of this manual.)
- All diagnostic services (e.g., radiology). This includes diagnostic services that are performed at a second hospital because the services are not available at the first hospital (e.g., CT scan) as well as transportation between the two hospitals. See the Transfers section in this chapter.
- Donor/Harvesting.
- All ancillary services provided by the hospital or performed by another entity under contract with the hospital (e.g., hospital has a contractual agreement with an enrolled independent laboratory).
Always refer to the long descriptions in coding books.
Unbundled Services (ARM 37.86.2905(5))
Services that are not included in the APR-DRG payment and can be billed separately include the following:
- Dialysis: Effective October 1, 2008.
- Long-Acting Reversible Contraception (LARC): Effective January 1, 2015, Montana Healthcare Programs allows PPS hospitals to unbundle LARC devices (e.g., IUDs and contraceptive implants) and the insertion from the inpatient delivery claim. These services can be billed as an outpatient service on a 13X type of bill and will be paid at the OPPS rates. The following HCPCS/CPT codes are allowed:
- J7300 – Paragard, intrauterine copper contraceptive.
- J7301 – Skyla, levonorgestrel-releasing intrauterine contraceptive, 13.5 mg
- J7302 – Mirena, levonorgestrel-releasing intrauterine contraceptive, 52 mg
- J7307 – Implanon/Nexplanon, etonogestrel (contraceptive) implant system, including implant and supplies
- 11981 – Insertion of drug delivery implant
- 58300 – Insertion of intrauterine device
Split/Interim Billing
Some inpatient hospital services necessitate the use of split or interim bills for Montana Healthcare Programs reimbursement. In general, providers cannot split bill APR-DRG claims, except in a few cases:
- When Medicare lifetime reserve days have been exhausted, inpatient claims must be submitted to the Department for review. Documentation of exhaustion must be attached to the claim.
- For members classified as hospital residents. Claims for members approved and classified as hospital residents may be interim billed on a monthly basis after the first 180 days. These claims must be sent to the Department with a letter of explanation for manual pricing. The Department may approve the special billing and forward the claim to the claims processing contractor for processing with pricing instructions. Before billing for residents, the provider must obtain resident status for the member. (See Obtaining Resident Status in this manual’s Covered Services chapter.)
- Hospitals subject to the inpatient hospital prospective payment reimbursement method may only interim bill when the member has been a patient in the same facility at least 30 days, is Montana Healthcare Programs-eligible for a minimum of these 30 days, and has received prior authorization, in which case the hospital may bill every 30 days. Interim claims are paid by a per diem amount
multiplied by the number of covered Montana Healthcare Programs eligible days. Upon patient discharge, the interim claims will be voided or credited by the hospital and the hospital must bill a single admit through a discharge claim which will be paid by APR-DRG. - The Department will not accept late charges (Type of bill = 115). Instead, hospitals are instructed to adjust earlier claims if appropriate.
Partial Eligibility
APR-DRG hospitals do not split bill. Bill the entire claim from the date of admit, and the claim will be prorated during processing.
Incurment
All APR-DRG hospitals must bill from the date of admission. For more information on incurment, see the Member Eligibility and Responsibilities chapter in the General Information for Providers manual.
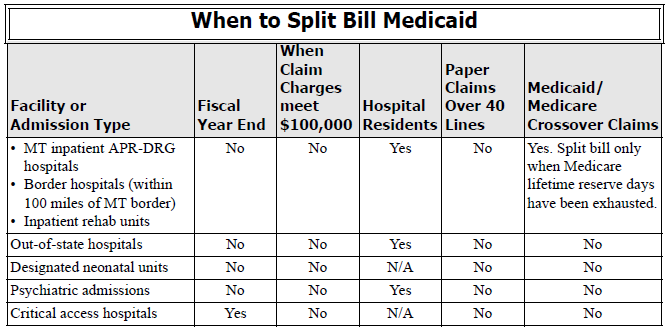
Billing for Abortions and Sterilizations
In order to be covered by Montana Healthcare Programs, abortions and sterilizations require specific forms to be completed and submitted with the claim. For more information on abortion and sterilization requirements, see the Covered Services chapter in this manual. Forms are available on the Provider Information website.
Abortions
A completed Montana Healthcare Programs Physician Certification for Abortion Services (MA-37) form must be attached to every abortion claim or payment will be denied. Complete only one part of this form. This is the only form Montana Healthcare Programs accepts for abortions.
Sterilization
- For elective sterilizations, a completed Informed Consent to Sterilization (MA-38) form must be attached to the claim for each provider involved or payment will be denied. This form must be legible, complete, and accurate, and revisions are not accepted. It is the provider’s responsibility to obtain a copy of the form from the primary or attending physician.
- For medically necessary sterilizations (including hysterectomies), one of the following must be attached to the claim, or payment will be denied:
- A completed Montana Healthcare Programs Hysterectomy Acknowledgement form (MA-39) for each provider submitting a claim. It is the billing provider’s responsibility to obtain a copy of the form from the primary or attending physician. Complete only one section of this form. When no prior sterility or life-threatening emergency exists, the member and physician must sign and date Section A of this form prior to the procedure. (See 42 CFR 441.250 for the federal policy on hysterectomies and sterilizations.) Also, for Section A, signatures dated after the surgery date require manual review of medical records by the Department. The Department must verify that the member (and representative, if any) was informed orally and in writing, prior to the surgery, that the procedure would render the member permanently incapable of reproducing. The member does not need to sign this form when Sections B or C are used.
- For members who have become retroactively eligible for Montana Healthcare Programs, the physician must certify in writing that the surgery was performed for medical reasons and must document one of the following:
- The member was informed prior to the hysterectomy that the operation would render him/her permanently incapable of reproducing.
- The reason for the hysterectomy was a life-threatening emergency.
- The member was already sterile at the time of the hysterectomy and the reason for prior sterility.
When billing for retroactively eligible members, attach a copy of the 160-M to the claim if the date of service is more than 12 months earlier than the date the claim is submitted. For more information, see the Covered Services chapter in this manual.
Billing Unlisted Services or Procedures
Providers should use the most specific HCPCS code when billing a service or procedure to enable proper reimbursement. In the event an unlisted service or procedure code must be used, Montana Healthcare Programs urges providers to send medical records with the claim. Reviewing the medical records with the claim allows the claims processing personnel to understand the situation and apply appropriate reimbursement, as well as decreases claims processing time. Medical records can be sent with electronic claims through the use of the paperwork attachment.
When submitting claims that require additional supporting documentation, the Attachment Control Number field must be populated with an identifier. Identifier formats can be designed by software vendors or clearinghouses, but the preferred method is the provider's Montana Healthcare Programs ID number followed by the member's ID number and the date of service, each separated by a dash.
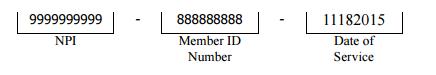
The supporting documentation must be submitted with a Paperwork Attachment Cover Sheet. The number in the paper Attachment Control Number field must match the number on the cover sheet.
End Billing Procedures Chapter
Submitting a Claim
Paper Claims
The services described in this manual are billed on UB-04 claim forms. Use this chapter with the UB-04 claim instructions on the Provider Information website.
Claims submitted with all of the necessary information are referred to as clean and are usually paid in a timely manner. (See the Billing Procedures chapter in the General Information for Providers manual.)
Field 7 is used for cost Passport referral number and sharing indicators. See the table below and UB-04 claim instructions on the Provider Information website.
Passport Indicators
Passport to Health Indicators
Code - Used When Providing
FPS - Family planning services
OBS - Obstetrical services
TCM - Targeted case management services
Present on Admission
The present on admission (POA) indicator is required for all inpatient claims. The claim will deny if there is no valid POA indicator for each diagnosis. Valid values for POA are:
Y = Present at the time of inpatient admission
N = Not present at the time of inpatient admission
U = Documentation is insufficient to determine whether condition is present on admission.
W = Provider is unable to clinically determine whether condition was present on admission.
End Submitting a Claim Chapter
How Payment Is Calculated
Overview
Though providers do not need the information in this chapter to submit claims to the Department, the information allows providers to understand how payment is calculated and to predict approximate payment for particular claims.
The Inpatient Prospective Payment System (PPS)
Several methods of payment are used for inpatient hospital services. These include prospective payment using the All Patient Refined Diagnosis-Related Group (APR-DRG), cost-based payment that is retrospectively adjusted at the end of a reporting period and payment based on a percentage of allowed charges.
- Prospective payment using the APR-DRG method is used for:
- In-State Prospective Payment System Hospitals
- Border hospitals (within 100 miles of Montana’s border)
- Distinct-part units of Montana APR-DRG hospitals and border hospitals.
- Acute care psychiatric hospitals
- Center of Excellence Facilities
- Out-of-state hospitals
- Hospitals and services subject to the cost based payment method include:
- In-state critical access hospitals (CAHs)
The Inpatient Prospective Payment Method Using All Patient Refined Diagnosis Related Groups (APR-DRG)
For most cases, payment equals the relative weight for the APR-DRG times the base price plus the applicable additive factors, such as cost outliers and disproportionate share hospital payment. The overall method is patterned after similar payment policies used by Medicare. When specific details of the payment method differ between Medicare and Montana Healthcare Programs, then the Montana Healthcare Programs policy prevails. Hospitals are not required to purchase grouping software and need not indicate the APR-DRG on the claim.
Upon the discharge or transfer of each member, hospitals submit a claim to Montana Healthcare Programs. The Department reimburses hospitals a per-stay rate based on All Patient Refined Diagnosis Related Groups (APR-DRGs). The claim will provide, among other information, the member’s principal diagnosis, additional diagnoses, principal and secondary procedures, age, sex and discharge status. These variables are passed through an APR-DRG grouper program to determine the appropriate APR-DRG for each discharge. Although hospitals may indicate the anticipated APR-DRG on the billing invoice, the Montana Healthcare Programs grouper program is the final determinant in assigning the payable APR-DRG to each case. Interim billing is only allowed in specific situations noted in this chapter.
After Montana Healthcare Programs has determined the allowed payment amount, that amount is reduced by any reported third party liability (TPL) amount, cost share amount, Medicare Part A payment amount and member responsibility (Incurment), then Montana Healthcare Programs pays the remainder.
Hospitals reimbursed using the inpatient prospective payment method are not subject to retrospective cost reimbursement.
Ungroupable DRG
Claims may sometimes deny for an ungroupable DRG, which is an error in DRG assignment. These errors occur when an invalid or non-existent ICD code is used. Providers should use the ICD codes applicable to the member’s dates of service. For claims that deny due to an ungroupable DRG, providers should re-code thee claim to a more specific and accurate code for the service provided.
Relative Weights and Reimbursement Data
APR-DRG Relative Weights
For each APR-DRG, a relative weight factor is assigned. The relative weight is applied to determine the APR-DRG Base Payment that will be paid for each admit-through-discharge case regardless of the specific services provided or the length of stay. The APR-DRG relative weight is a weight assigned that reflects the typical resources consumed.
APR-DRG weights are reviewed and updated periodically by the Department. The weights are adapted from national databases of millions of inpatient stays and are then “re-centered” so that the average Montana Healthcare Programs stay in a base year has a weight of 1.00.
When the Department determines that adjustments to relative weights for specific APR-DRGs are appropriate to meet Montana Healthcare Programs policy goals related to access to quality care, a policy adjustor may be explicitly applied to increase or decrease these relative weights. Policy adjustors are intended to be budget neutral, that is, they change payments for one type of service relative to other types without increasing or decreasing payments overall.
DRG Base Price
There are two different base prices for stays in acute care hospitals and Center of Excellence hospitals. The base price is a dollar amount that is reviewed by the Department each year. Changes in the APR-DRG Base Price are subject to the public notice requirements of the Montana Code Annotated.
APR-DRG Base Payment
For each stay, the DRG Base Payment equals the DRG Relative Weight multiplied by the DRG Base Price.
Computational Formulas and Definitions
- Covered Charges = Sum of line item charges minus line noncovered charges from the claim.
- Out-of-state statewide Cost-to-Charge Ratio.
- Base Price = Statewide average cost per discharge. The base price is published in the Administrative Rules of Montana.
- Gross APR-DRG Amount = Base price multiplied by APR-DRG relative weight.
- Cost Outlier Amount = (Allowed charges multiplied by the statewide/ hospital-specific cost-to-charge ratio) minus the cost outlier threshold) multiplied by the marginal cost outlier percentage.
- Allowed Montana Healthcare Programs APR-DRG payment = Gross APR-DRG amount plus cost outlier amount.
- Per Diem = Allowed Montana Healthcare Programs APR-DRG payment / national average length of stay for the APR-DRG.
- Transferring hospitals: First Day = 2 x Gross / LOS + outlier Subsequent Days = Gross/LOS.
- Partial eligibility = APR-DRG per diem x eligible days
- Hospital Specific Cost-to-Charge Ratio.
The posted APR-DRG Fee Schedule contains all of the above information.
Payment Factors
Capital Related Costs
Capital cost is included in the DRG-based payment and will not be paid separately.
Cost Outlier Payments
It is recognized that there are occasional stays that are extraordinarily costly in relation to other stays within the same APR-DRG because of the severity of the illness or complicating conditions. These variations are recognized by the cost outlier payment which is an add-on payment for expenses that are not predictable by the diagnosis, procedures performed, and other statistical data captured by the APR-DRG grouper.
Cost outlier stays are stays that exceed the cost outlier threshold for the APR-DRG. To determine if a hospital stay exceeds the cost outlier threshold, the Montana Healthcare Programs program excludes all services that are not medically necessary. Montana Healthcare Programs then converts the charge information for medical necessary services into the estimated cost of the stay by applying the statewide average PPS inpatient cost-to-charge radio (CCR). The estimated cost for medically necessary services is then compared to the cost outlier threshold for the appropriate APR-DRG to determine if the stay qualifies for reimbursement as a cost outlier. Costs exceeding the threshold are multiplied by a marginal cost ratio to determine the cost outlier payment.
Transfer Payment Adjustments
The transfer payment adjustment applies when a patient is transferred to another acute care hospital. It does not apply when a patient is discharged to a post-acute setting such as a skilled nursing facility. The receiving hospital is not impacted by the transfer payment adjustment unless it transfers the patient to another hospital.
In the transfer payment adjustment, payment is calculated as if the beneficiary were not a transfer, then payment is adjusted. The APR-DRG Gross Payment is divided by the nationwide average length of stay for the assigned APR-DRG to arrive at a per diem amount. The per diem amount is then multiplied by the actual length of stay, except that payment is doubled for the first day to reflect costs related to the admitting process. If the transfer payment adjustment results in an amount greater than the amount without the adjustment, the transfer payment adjustment is disregarded. The cost outlier payment, if applicable, is then added to the APR-DRG base payment, with the transfer adjustment made as needed.
The transfer payment adjustment is not applicable to providers and services that are exempt from the Inpatient Prospective Payment Method.
Prorated Payment Adjustment
When a beneficiary has Montana Healthcare Programs coverage for fewer days than the length of stay, the payment is prorated. The APR-DRG Gross Payment plus cost outlier payments, if applicable, is divided by the nationwide average length of stay for the assigned APR-DRG to arrive at a per diem amount. The per diem amount is then multiplied by the number of days the beneficiary is eligible for Montana Healthcare Programs during the stay. If the prorated payment adjustment results in a payment amount greater than the amount without the adjustment, the prorated payment is disregarded.
The Prorated Payment Adjustment is not applicable to providers and services that are exempt from the Inpatient Prospective Payment Method. See the section titled Exempt Services and Costs.
The Cost-Based Payment Method for Exempt Hospitals and Services
The following providers are exempt from the Inpatient Prospective Payment Method. In the interest of clarity, this list includes acute care hospitals as well as facilities that provide similar inpatient services.
- Indian Health Service hospitals
- The Montana State Hospital
- Psychiatric residential treatment facilities
- Critical access hospitals
Exempt Services and Costs
The following services are exempt from the Inpatient Prospective Payment method even when provided by hospitals that are otherwise subject to prospective payment.
- Services where Medicare is the primary payer (crossover claims)
- Certified Registered Nurse Anesthetist costs as defined by Medicare
- Health Care Acquired Conditions as defined by the Centers for Medicare and Montana Healthcare Programs Services (CMS).
Reasonable Cost Reimbursement
Hospitals exempt from prospective payment will continue to use the Title XVIII retrospective reasonable cost principals for reimbursing Montana Healthcare Programs inpatient hospitals services. Allowable costs will be determined in accordance with generally accepted accounting principals as defined by the American Institute of Certified Public Accountants. Such definition of allowable costs is further defined in accordance with the Medicare Provider Reimbursement Manual, CMS Pub. 15-1, subject to the exceptions and limitations provided in the Department’s Administrative Rules. Pub. 15 is a manual published by the United States Department of Health and Human Services, CMS, which provides guidelines and policies to implement Medicare regulations which set forth principals for determining the reasonable cost of provider services furnished under the Health Insurance for Aged Act of 1965, as amended.
Hospitals subject to retrospective reasonable cost reimbursement shall receive interim payments weekly or biweekly during the facility’s fiscal year by submitting claims to the Department’s fiscal intermediary. The interim payment rate will be based on a percentage of customary (billed) charges to costs as determined by the facility’s most recently settled Montana Healthcare Programs cost report. If a provider fails to submit financial information to compute the rate, the provider will be reimbursed at 50 percent of its usual and customary billed charges. Hospital providers are required to submit the CMS 2552-96 to the Medicare Fiscal Intermediary (FI) and the Department within five months of their fiscal year end. The FI either audits or desk reviews the cost report, then sends the Department the “as adjusted” cost report. Montana Healthcare Programs settlements are made from the “as adjusted” cost report.
For each hospital that is a critical access hospital, reimbursement for reasonable costs of inpatient hospital services shall be limited to the lesser of 101 percent of allowable costs or the upper payment limit.
Services where Medicare is the primary payer (crossover claims) are not reimbursed using retrospective cost principles. Reimbursement for these services is the remaining coinsurance and deductible. The Department shall reimburse cost-based inpatient hospital service providers for certified registered nurse anesthetists costs on a reasonable cost basis.
Hospital Residents
Payment for hospital residents will be made as follows:
- Payment for at least the first 180 days of inpatient care at the same facility will be the APR-DRG payment plus any appropriate outliers; and
- Payment for all medically necessary member care subsequent to the request date, which must be greater than 180 days, will be reimbursed at 80% of the hospital-specific estimated cost-to-charge ratio as computed by the Department without cost settlement.
- Services must be prior authorized.
How Payment Is Calculated on TPL Claims
When a member has coverage from both Montana Healthcare Programs and another insurance company, the other insurance company is often referred to as third party liability (TPL). In these cases, the other insurance is the primary payer, and Montana Healthcare Programs makes a payment as the secondary payer. Montana Healthcare Programs will make a payment only when the TPL payment is less than the Montana Healthcare Programs allowed amount.
How Payment Is Calculated on Medicare Crossover Claims
When a member has coverage from both Medicare and Montana Healthcare Programs, Medicare is the primary payer. Montana Healthcare Programs will pay the coinsurance and deductible, less any TPL or
incurment, on inpatient hospital claims for these dually eligible individuals.
Payment Examples for Dually Eligible Members
Member Has Medicare and Montana Healthcare Programs Coverage. A provider submits an inpatient hospital claim for a member with Medicare and Montana Healthcare Programs. The Medicare coinsurance and deductible are $65.00 and $185.00. This total ($250.00) becomes the Montana Healthcare Programs allowed amount. Montana Healthcare Programs will pay this amount ($250.00) as long as no TPL or incurment amounts are applicable.
Member Has Medicare, Montana Healthcare Programs coverage, and TPL. A provider submits an inpatient hospital claim for a member with Medicare, Montana Healthcare Programs, and TPL. The Medicare coinsurance and deductible are $65.00 and $185.00. This total ($250.00) becomes the Montana Healthcare Programs allowed amount. The other insurance company paid $225.00. This amount is subtracted from the Montana Healthcare Programs allowed amount leaving $25.00. Montana Healthcare Programs pays $25.00 for this claim. If the TPL payment had been $250.00 or more, this claim would have paid at $0.00.
Disproportionate Share Hospital (DSH) Payments (ARM 37.86.2925)
Disproportionate Share Hospital (DSH) payments, including routine and supplemental DSH payments, will be limited to the cap established by the Federal Centers for Medicare and Montana Healthcare Programs Services (CMS) for Montana.
Routine DSH shall receive an additional payment amount equal to the product of the hospital’s prospective base rate x the adjustment percent of 4% rural hospital and 10% urban hospitals. All Supplemental Disproportionate Share Hospitals (SDSH) shall receive an SDSH payment. DSH payments will only be given to eligible in-state hospitals.
End How Payment is Calculated Chapter
Appendix A - Forms
These forms are available on the Forms page of the Provider Information website.
- Request for Medicaid Home Infusion Therapy Authorization
- Individual Adjustment Request
- Paperwork Attachment Cover Sheet
End of Appendix A Chapter
Definitions and Acronyms
Bolus
A small volume of drug, which is administered directly into the vein, usually over a time period of 3–5 minutes.
Continuous
A controlled method of prolonged drug administration that includes the ability to control the delivery rate. This system permits the drug to be available to the body at a constant level.
Infusion
A parenteral solution administered intravenously or subcutaneously over an extended period of time. Typically requires an infusion pump, but may be accomplished by gravity feed.
Infusion Device/Infusion Pump
Electronic or mechanical device designed to provide continuous, intermittent, circadian, cyclical and/or bolus delivery of medications or nutrients via parenteral. Infusion pumps are generally considered to be closed systems, which helps to prevent inadvertent contact with sterile solutions. Infusion devices may be disposable or reusable. All are covered within the per diem.
Intravenous (IV)
Injection of a solution directly into the vein, usually the cephalic or median basilica vein of the arm.
National Drug Code (NDC)
An 11-digit number the manufacturer assigns to a pharmaceutical product and attaches to the product container at the time of packaging that identifies the product’s manufacturer, dose form and strength, and package size.
Parenteral
Denoting any medication route other than the alimentary canal, such as intravenous, subcutaneous, intramuscular, or mucosal.
Subcutaneous
Infusion of solutions into the subcutaneous tissue beneath the skin.
End of Definitions and Acronyms Chapter
Index
Previous editions of this manual contained an index.
This edition has three search options.
- Search the whole manual. Open the Complete Manual pane. From your keyboard press the Ctrl and F keys at the same time. A search box will appear. Type in a descriptive or key word (for example "Denials". The search box will show all locations where denials discussed in the manual.
- Search by Chapter. Open any Chapter tab (for example the "Billing Procedures" tab). From your keyboard press the Ctrl and F keys at the same time. A search box will appear. Type in a descriptive or key word (for example "Denials". The search box will show where denials discussed in just that chapter.
- Site Search. Search the manual as well as other documents related to a particular search term on the Montana Healthcare Programs Site Specific Search page.
End of Index Chapter
End of Hospital Inpatient Services Manual